The impact of monitor distance on task performance in minimal access surgery
The Impact Of Monitor Distance On Task Performance In Minimal Access Surgery
Submitted By Dr.Awadalla Musa Abbakar Matar Roll No: Tgou (N) /005/Pg//M.Mas/2011d
To The Department Of Minimal Access Surgery (Mas) Of The Global Open (Tgo) University Of Nagaland, India
To The Department Of Minimal Access Surgery (Mas) Of The Global Open (Tgo) University Of Nagaland, India (Established
Under The Global Open University Act 2006, Government Of Nagaland)
In Partial Fulfillment For The Award Of Masters Degree In Minimal Access Surgery (M.Mas) February 2015
Submitted By Dr.Awadalla Musa Abbakar Matar Roll No: Tgou (N) /005/Pg//M.Mas/2011d
To The Department Of Minimal Access Surgery (Mas) Of The Global Open (Tgo) University Of Nagaland, India
To The Department Of Minimal Access Surgery (Mas) Of The Global Open (Tgo) University Of Nagaland, India (Established
Under The Global Open University Act 2006, Government Of Nagaland)
In Partial Fulfillment For The Award Of Masters Degree In Minimal Access Surgery (M.Mas) February 2015
In Partial Fulfillment For The Award Of Masters Degree In Minimal Access Surgery (M.MAS) February 2015 World Laparoscopy Hospital, X-100, Cyber City, Gurgaon-122002 NCR Delhi, (INDIA) Ph. +919811416838, +91-0124-2351555 Email: contact@laparoscopyhospital.com Website: www. Laparoscopyhospital.com
CERTIFICATION We have participated and supervised this research done by Dr. Awadalla Musa Abbakar Matar on “The Impact of Monitor Distance on Task Performance in Minimal Access Surgery”
Guide:
DR (PROF) R. K. MISHRA MBBS, MS, M.MAS, F.MAS, DMAS, FICR, PhD Professor and Head of Minimal Access Surgery TGO University of Nagaland and Director, World Laparoscopy Hospital, Gurgaon, India
Co-Guide:
Dr. J. S. CHAUHAN MBBS, MS, FMAS, DMAS, PGDHHM Faculty and Consultant Surgeon World Laparoscopy Hospital, Gurgaon, India Member of the Association of Surgeons of India
DR. AWADALLA MUSA ABBAKAR MTAR MBBS, MD, F.MAS, D.MAS
DR. AWADALLA MUSA ABBAKAR MTAR MBBS, MD, F.MAS, D.MAS
DECLARATION: I Dr. Awadalla Musa Abbakar Matar do hereby certify I had personally carried out the work depicted in the thesis titled “The Impact of Monitor Distance on Task Performance in Minimal Access Surgery” No part of thesis has been submitted for the award of any other degree or diploma prior to this date. And I have no objection for this thesis to be copied in part or whole, or used for research purposes. Dr. Awadalla Musa Abbakar Matar MD, F.MAS, D. MAS.
AKNOWLEGEMENTS: I would like to express the deepest appreciation to my research supervisor Professor R. K. Mishra who has shown the attitude and the substance of a genius: he continually and persuasively conveyed a spirit of adventure in regard to research and scholarship, and an excitement in regard to teaching. Without his supervision and constant help this dissertation would not have been possible. I’m also indebted to him for allowing me to include copyright part from his book in the history of laparoscopy as part of my dissertation. I would like to thank my co-supervisor, Professor J. S. Schauhan whose work demonstrated to me that concern for medicine in general supported by an “engagement” in minimal access surgery, should always transcend academia and provide a quest for our times. My special gratitude also goes to my colleagues in Al-Bijadiyah and Al-Quayiya Hospitals, Saudi Arabia, who willingly participated in this study. I’m greatly indebted to Dr. Sara of the National Guard hospital, Riyadh, Saudi Arabia, and to Dr. Yuhua Su, Head of Yuhua Su consulting Statistics, USA, for validating, analyzing and interpreting the data. I would like to take this opportunity to thank my friend Dr. Osman Ahmed who proved to me that a friend in need a friend indeed. Last, but not least I must show my greatest indebtedness to my wife Yousra, my son Mosab and my daughter Nena for adding the dimension of love, passion and warmth to my life. Their continuous support provided me with the energy to cope with the endeavor to complete this project.
DEDICATION: To the greatest love story of my life The one whom Allah has placed paradise beneath her feet To my mother May Allah the almighty give her all the blessings.
ABSTRACT:
Background: The distance and location of the image displayed on the monitor screen affects the efficiency of task execution in minimal access surgery. It also carries direct impact on the surgeon by causing musculoskeletal injury and ocular discomfort. This compromises patient safety and affects the well-being of the surgeon.
Methods: 20 physicians with no experience in minimal access surgery participated in beads transfer in a pelvi-trainer. Correctly placed beads count was taken as the measure of task performance. The monitor was placed co-axially, with 10-15 degrees down-gaze at three distances from the physician: DX2, DX3 and DX4, where D is the diameter of the monitor screen. Subjective rating of eye and neck discomfort on a 0-10 pain score was obtained from the participants. The participants also answered a question on the preferred monitor distance.
Results: Beads count was significantly higher at DX2 compared to D4. The relationship between eye discomfort and beads count was also significant. Older participants performed better than the younger in beads count. However, they developed more eye and neck discomfort. 40% of the participants preferred DX2, 40% preferred DX3 and 20% preferred Dx4.
Conclusion: Monitor distance and eye discomfort affected task performance. Middle aged physicians performed better task, however, they developed more eye discomfort and neck muscle fatigue.
- Introduction: Surgery moved dramatically from its conventional open methods to an era where therapeutic interventions are increasingly carried out from images of the operative site. In minimal access surgery the image display system is the visual interface between the surgeon and the operative field. The quality and the attributes of the displayed visual information are critical to safe execution of the operation conducted by this approach. The current video-endoscopic system is monocular. This is to be contrasted with the binocular vision. This carries its inherent limitations which will result in image degradation. Some of these limitations are related to ergonomics of the imaging of the operative field and others are related to quality of the image display 1, 2 . Minimally invasive surgery has been a great benefit to the patient in the form of less operative trauma, smaller scar, speedy recovery and resumption of normal activity when compared to open surgery. However this type of surgery requires the surgeon to assume atypical postures for extended periods of time compared to open surgery. As a result surgeon experiences extensive muscle fatigue and chronic injury 2 . Among several factors, monitor placement contributes to the precision of task performance. The optimal visual display system is yet to be established. With regard to location of the image display, the best task performance is obtained when the monitor is placed in front of the surgeon, at the level of the surgeon hands and close to the operative field 2, 3 . Front viewing of the monitor permits correct alignment of the visual and motor access. The 10-15 degrees gaze down frontal viewing restores alignment of the visual and motor axes of the surgeon and permits both sensory signals and motor control to have a closer spatial location thus bringing visual signals in correspondence with instrument manipulation, similar to the situation experienced in conventional open surgery 1, 2 . Viewing distance is highly dependent on monitor size. It should be far enough to avoid extensive accommodation of the eyes and conversion by the extra-ocular musculature and it should be close enough to avoid staring and loss of detail.
Historical background: The concept of minimal access surgery can be traced back to Hippocrates (460-370 BC).In his scriptures Hippocrates examined the rectum of a patient with a speculum. Ibn Sinna used candles and sunlight in surgical operations, s at the beginning of the 6th century4.
Several surgeons and gynecologists contributed in the milestone of minimal access surgery, in the areas of visualization, instrument design and pneumoperitonium. A brief account of the optics milestones is given herein 4 .
Several surgeons and gynecologists contributed in the milestone of minimal access surgery, in the areas of visualization, instrument design and pneumoperitonium. A brief account of the optics milestones is given herein 4 .
1585 Arnazi was the first to use a light source for an endoscopic procedure, focusing sunlight through a flask of water and projecting the light into the nasal cavity.
1806 Philip Bozzini, built an instrument that could be introduced in the human body to visualize the internal organs. He called this instrument “LICHTLEITER”. Bozzini used an aluminum tube to visualize the genitourinary tract. The tube illuminated with wax candle, he fitted mirrors to reflect images. 1
867 Desormeaux, used an open tube to examine the genitourinary tract, combining alcohol and turpentine with a flame in order to generate a brighter, more condensable beam of light.
1901 Dimitri Ott, a Petrograd gynecologist used head mirrors to reflect light and augment visualization.
1929 Kalk, a German physician introduced the forward oblique (135 degrees).
1953 The rigid lens system was discovered by Professor John Hopkins. The credit of videoscopic surgery goes to this surgeon who has revolutionized the concept by making this instrument.
1983 Semm, German gynecologist, performed the first laparoscopic appendectomy.
1985 The first documented laparoscopic cholecystectomy was performed by Erich Muhe in Germany. Cholecystectomy is the laparoscopic procedure which revolutionized the general surgery.
1994 First robotic arm was designed to hold the telescope with the goal of improving safety and reducing the need of a skilled camera operator. 3
2001 the Lindbergh operation, named in honor of the American Aviator Charled Lindberghm was first ever transatlantic surgery. Doctors Michel Ganger and Jacques Marescaux removed the gallbladder of 68-year women in Strasbourg, France from New York. The surgeon used a ZEUS Robotic system from Computormotion Inc. and ATM fibreoptic connection provide by France Telecom.
1585 Arnazi was the first to use a light source for an endoscopic procedure, focusing sunlight through a flask of water and projecting the light into the nasal cavity.
1806 Philip Bozzini, built an instrument that could be introduced in the human body to visualize the internal organs. He called this instrument “LICHTLEITER”. Bozzini used an aluminum tube to visualize the genitourinary tract. The tube illuminated with wax candle, he fitted mirrors to reflect images. 1
867 Desormeaux, used an open tube to examine the genitourinary tract, combining alcohol and turpentine with a flame in order to generate a brighter, more condensable beam of light.
1901 Dimitri Ott, a Petrograd gynecologist used head mirrors to reflect light and augment visualization.
1929 Kalk, a German physician introduced the forward oblique (135 degrees).
1953 The rigid lens system was discovered by Professor John Hopkins. The credit of videoscopic surgery goes to this surgeon who has revolutionized the concept by making this instrument.
1983 Semm, German gynecologist, performed the first laparoscopic appendectomy.
1985 The first documented laparoscopic cholecystectomy was performed by Erich Muhe in Germany. Cholecystectomy is the laparoscopic procedure which revolutionized the general surgery.
1994 First robotic arm was designed to hold the telescope with the goal of improving safety and reducing the need of a skilled camera operator. 3
2001 the Lindbergh operation, named in honor of the American Aviator Charled Lindberghm was first ever transatlantic surgery. Doctors Michel Ganger and Jacques Marescaux removed the gallbladder of 68-year women in Strasbourg, France from New York. The surgeon used a ZEUS Robotic system from Computormotion Inc. and ATM fibreoptic connection provide by France Telecom.
Figure 1.1: Dr. Harold Hopkins (1918-1940)
1.3 Aims and objectives of the study
1.4 General objective: The general objective of this study is to test the relationship between monitor distance and the efficiency of task performance.
1.5 Specific objectives:
1. To compare the efficiency of task performance through beads transfer counting at 3 monitor distances; Dx2, Dx3 and Dx4 where D is the diameter of the Monitor.
2. To find out the optimal distance between the monitor and surgeon.
3. To perform subjective comparison of surgeon fatigue in the form of neck pain and eye discomfort in relation to the three monitor distances.
2.1 Literature review
2.2 Ergonomics of imaging operative field: Ergonomics may be defined as “the science that deals with the considerations of human characteristics, expectations and behaviors in the design of things people use in their work and everyday lives and of the environment in which they work and live” 5 . With minimal Access surgery (MAS) a man-machine environment was brought into the operating room. This brought physical and mental changes for the operating team. The science of ergonomics analyzes these challenges and formulates guidelines for creating a work environment that is safe and comfortable for its operators while effectiveness and efficiency of the process are maintained.
As MAS has become established, significant research and development (R & D) on the ergonomics and the optimization for the “imaging chain” for MAS has been undertaken in recent years in order to facilitate execution of these operations by the surgeon. The stimulus to this R & D and related technology research has been the identification of current visual limitations in MAS. Concurrent with R & D, evaluation of novel/ emerging technology is essential for real progress that translates into clinical benefit. Progress thus entails a multidisciplinary approach involving surgeons, ergonomists, psychologists and physical scientists and engineers involved in technical R & D related to MAS1 .
Optimum task performance is obtained when the optical axis of the endoscope is perpendicular to the Target plane1 . The body built of the patient and location of the operative site would vary from one occasion to another. Therefore the placement of the optical port and the selection of endoscope are important considerations.
Zero degree, 30 degree and 45 degree endoscopes are commonly used. The direction of view of the endoscope has no significant effect on task performance as far as the optical axis is perpendicular to the surface. However in practice only oblique viewing endoscopes will obtain an angle closer to 90 degree and thus are preferred to the forward viewing endoscopes.
As MAS has become established, significant research and development (R & D) on the ergonomics and the optimization for the “imaging chain” for MAS has been undertaken in recent years in order to facilitate execution of these operations by the surgeon. The stimulus to this R & D and related technology research has been the identification of current visual limitations in MAS. Concurrent with R & D, evaluation of novel/ emerging technology is essential for real progress that translates into clinical benefit. Progress thus entails a multidisciplinary approach involving surgeons, ergonomists, psychologists and physical scientists and engineers involved in technical R & D related to MAS1 .
Optimum task performance is obtained when the optical axis of the endoscope is perpendicular to the Target plane1 . The body built of the patient and location of the operative site would vary from one occasion to another. Therefore the placement of the optical port and the selection of endoscope are important considerations.
Zero degree, 30 degree and 45 degree endoscopes are commonly used. The direction of view of the endoscope has no significant effect on task performance as far as the optical axis is perpendicular to the surface. However in practice only oblique viewing endoscopes will obtain an angle closer to 90 degree and thus are preferred to the forward viewing endoscopes.
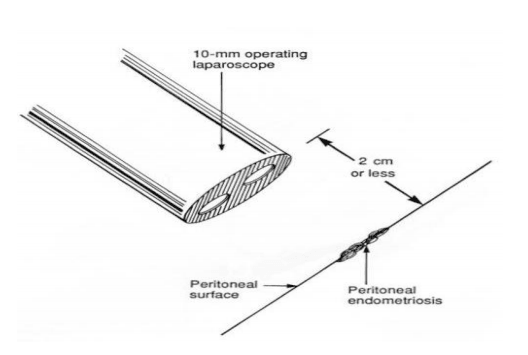
Figure 2.1: Direction of view of the endoscope.
In addition to that rotating the oblique viewing endoscope can add more visual perspectives and hence enhance correct interpretation of anatomy and allows execution of advanced laparoscopic procedures. In bimanual endoscopic tasks the best task performance is obtained when azimuth angle are equal on both sides of the endoscope .This is difficult to obtain in practice, but wide azimuth angle inequalities should be avoided as this will degrade efficiency of task execution.
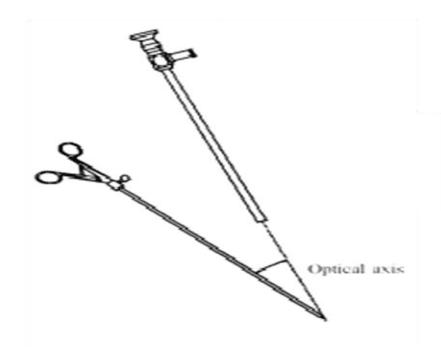
Figure 2.2: Azimuth Angle
Moreover, port positioning should avoid performing under mirror imaging. This will lead to reverse alignment and major degradation of task performance. Realignment can be obtained electronically (Reverse Digi – video STORZ Tubingen Germany) 1 , by rotating the image displayed by the monitor to 180 degrees or simply by rotating the camera with respect to the 6 endoscope. The beneficial effect of camera rotation is maintained with different optical axis to target views1 .
2.3 Safety, hazards and ergonomics in the operating room:
The operating room (OR) is one the most expensive areas in the hospital 6 . For this reason the optimization of the OR should be given priority at the time of financial stringency. The growing number of complex devices had led to increase interaction between man and technology. Ergonomics should thus address Hazards issues to patient staff and environment and necessary safety measures. In one study by Ulrich Matern et al .from Germany a survey was conducted among surgeons working in German hospitals. The survey consisted of 60 questions related to personal profile, the architectural situation, the devices and instruments as well as working posture and associated pain. The results showed elementary ergonomic deficiency within all fields. Surgeons stated that these deficiencies led to hazards for patients and personnel. 97 % of the surveyed surgeons see ergonomic improvement in the OR as necessary 6 .
Optimal position of monitors, OR lighting, devices and equipment, instruments and working posture of the surgeon are all important ergonomic issues to consider.
2.4 The laparoscopic video System
The video image plays the most crucial role in giving the surgeon information about the performance of the operation. Image quality depends on each component of the laparoscopic imaging unit which includes the camera, the laparoscope, the light source and light cable, the video monitor and the wiring system, the so called the magnificent chain 4,8 . Moreover the surgeon also needs to have an idea about the basic principles and specifications of the surgical video systems (i.e. the charged couple device (CCD) camera, monitors and digitizers. An insight into the future of laparoscopic video systems is also necessary for the practicing surgeon as well as methods to improving the quality of imaging and troubleshooting.
The operating room (OR) is one the most expensive areas in the hospital 6 . For this reason the optimization of the OR should be given priority at the time of financial stringency. The growing number of complex devices had led to increase interaction between man and technology. Ergonomics should thus address Hazards issues to patient staff and environment and necessary safety measures. In one study by Ulrich Matern et al .from Germany a survey was conducted among surgeons working in German hospitals. The survey consisted of 60 questions related to personal profile, the architectural situation, the devices and instruments as well as working posture and associated pain. The results showed elementary ergonomic deficiency within all fields. Surgeons stated that these deficiencies led to hazards for patients and personnel. 97 % of the surveyed surgeons see ergonomic improvement in the OR as necessary 6 .
Optimal position of monitors, OR lighting, devices and equipment, instruments and working posture of the surgeon are all important ergonomic issues to consider.
2.4 The laparoscopic video System
The video image plays the most crucial role in giving the surgeon information about the performance of the operation. Image quality depends on each component of the laparoscopic imaging unit which includes the camera, the laparoscope, the light source and light cable, the video monitor and the wiring system, the so called the magnificent chain 4,8 . Moreover the surgeon also needs to have an idea about the basic principles and specifications of the surgical video systems (i.e. the charged couple device (CCD) camera, monitors and digitizers. An insight into the future of laparoscopic video systems is also necessary for the practicing surgeon as well as methods to improving the quality of imaging and troubleshooting.
2.5 How monitors work
Surgical video system monitors reproduce the images through the horizontal linear scanning concept, like the ordinary TV sets ,which have a picture tube with an electron gun and a glass faceplate with a fluorescent coating on its inside surface. When the electron beam strikes the phosphor coated screen, electrons are generated and the electron beam sweeps along one horizontal line covering all picture elements (Pixels) and returning very quickly to the left side to begin scanning the next horizontal line.
The larger the number of lines scanned the better is the resolution, but other factors limit this choice, and the required number of lines has been standardized at 525 for one complete picture or frame in the National Television System Committee (NTSC) transmission in the United States.
Time need to complete one frame with 525 lines is 1/30th of a second. The picture repetition rate equals 30 frames per second. The AC power frequency is 60 Hz which equal double the picture repetition rate and this should create flicker of the picture due to mismatching. To overcome this problem each frame is divided into two parts so that 60 views with even or odd lines are presented each second. Each group of odd or even lines is called a field this process of alternate line field scanning is called interlacing.
Surgical video system monitors reproduce the images through the horizontal linear scanning concept, like the ordinary TV sets ,which have a picture tube with an electron gun and a glass faceplate with a fluorescent coating on its inside surface. When the electron beam strikes the phosphor coated screen, electrons are generated and the electron beam sweeps along one horizontal line covering all picture elements (Pixels) and returning very quickly to the left side to begin scanning the next horizontal line.
The larger the number of lines scanned the better is the resolution, but other factors limit this choice, and the required number of lines has been standardized at 525 for one complete picture or frame in the National Television System Committee (NTSC) transmission in the United States.
Time need to complete one frame with 525 lines is 1/30th of a second. The picture repetition rate equals 30 frames per second. The AC power frequency is 60 Hz which equal double the picture repetition rate and this should create flicker of the picture due to mismatching. To overcome this problem each frame is divided into two parts so that 60 views with even or odd lines are presented each second. Each group of odd or even lines is called a field this process of alternate line field scanning is called interlacing.
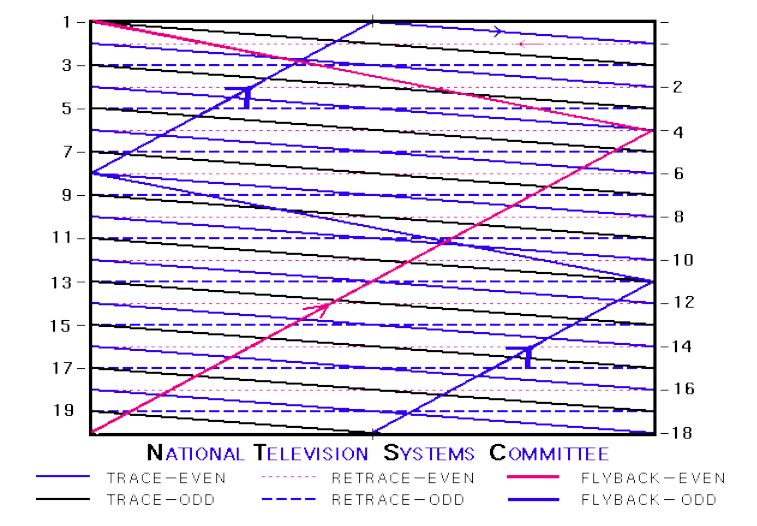
Figure 2.3: NTSC alternate field scanning (interlacing)
The detail of the video image is determined by lines of resolution, scanning lines, Pixels and dot pitch. Pixels are picture elements, each point of information on a picture is a pixel and the number of pixels governs the details of the picture. Pixels are represented by an individual photodiode on the camera chip. A raw of pixels is the digital representative of the scanning line. The dot pitch refers to the size of the phosphor elements on the monitor. It limits the amount of information in a scanning line.
2.6 Color information and video signal formats:
Color image information includes, essentially, the addition of color information to a preexisting black and white image. The color video signal is a combination of the monochrome black and white signal and the composite color signal. The monochrome signal is named the luminance signal as it includes only the brightness variations in the picture information. The color signal with the red, green and blue (RGB) information is the chrominance signal. Reproduction of the many different colors is accomplished by the addition of the primary colors (red, green, blue).
2.6 Color information and video signal formats:
Color image information includes, essentially, the addition of color information to a preexisting black and white image. The color video signal is a combination of the monochrome black and white signal and the composite color signal. The monochrome signal is named the luminance signal as it includes only the brightness variations in the picture information. The color signal with the red, green and blue (RGB) information is the chrominance signal. Reproduction of the many different colors is accomplished by the addition of the primary colors (red, green, blue).
2.7 Other television systems:
In the NTSC system the resolution of the monitor is limited to 525 horizontal lines. Other available television systems offer somewhat improved resolution as compared to NTSC. The Phase alternation by line (PAL) system used in the European countries offers monitor resolution with 625 lines very 1/25 second. The sequential color and memory storage (SECAM) is a French system offering 819 lines of resolution each1/25 second. These latter two systems are called combined because they combine color and brightness into one signal.
2.8 High Resolution Digital TV (HDTV) :
Digital Television (DTV) is based on the transmission of pure digital signals along with the reception and display of those signals on a digital monitor [10]. HDTV is the highest resolution DTV in the new standards. It offers 720 or 1080 lines of resolution compared to the 525 lines of resolution of the NTSC system of the United States. The result is a very detailed bright picture “almost” similar to three dimensional (3D). The impact of this technology on improving task performance or its preference over a three chip camera generated images is not yet objectively proved. In one study by M. A. Veelen et al from the Netherlands, twelve surgeons performed cholecystectomy using flat screen monitor in the optimal display location and cathode ray tube monitor on tower next to the operating table (current situation). The study concluded that the use of flat screen monitors was better for the physical and psychological comforts of the users, even though the technical performance was inferior in the comparison with that of regular monitors7 . The routine use of HDTV is limited by its high price. Because of incompatibility between the standard formats and HDTV monitors in the operating room video system has to be replaced at a high cost. In addition to this the image data obtained has to be stored only in compatible systems.
2.9 The camera signal:
The laparoscopic camera, being one of the most important instruments should be of good quality.
2.8 High Resolution Digital TV (HDTV) :
Digital Television (DTV) is based on the transmission of pure digital signals along with the reception and display of those signals on a digital monitor [10]. HDTV is the highest resolution DTV in the new standards. It offers 720 or 1080 lines of resolution compared to the 525 lines of resolution of the NTSC system of the United States. The result is a very detailed bright picture “almost” similar to three dimensional (3D). The impact of this technology on improving task performance or its preference over a three chip camera generated images is not yet objectively proved. In one study by M. A. Veelen et al from the Netherlands, twelve surgeons performed cholecystectomy using flat screen monitor in the optimal display location and cathode ray tube monitor on tower next to the operating table (current situation). The study concluded that the use of flat screen monitors was better for the physical and psychological comforts of the users, even though the technical performance was inferior in the comparison with that of regular monitors7 . The routine use of HDTV is limited by its high price. Because of incompatibility between the standard formats and HDTV monitors in the operating room video system has to be replaced at a high cost. In addition to this the image data obtained has to be stored only in compatible systems.
2.9 The camera signal:
The laparoscopic camera, being one of the most important instruments should be of good quality.

Figure 2.4: The Laparoscopic Camera
Modern cameras work with a charged couple device (CCD). The CCD consists of a dense grid of photocell receptors in a single silicon chip. Each photocell receptor passes an electronic signal to an image processor. Picture elements are termed pixels. The pixel represents the smallest element of the video image the compilation of which is ultimately displayed on the monitor. The image resolution depends on the number of pixels carried out on the chip. Current CCDs have approximately 330,000 pixels.
Cameras are either single chip or 3 chips. Single chip cameras supply a composite or super video home service (SVHS) signal are in widespread use. Color separation in single chip cameras is achieved by adding a stripe filter to the optical beam. Each of these filter stripes only accepts a definite color: red (R), green (G) and blue (B) on the definitive color combination principle. The luminance signal and the chrominance signals are generated from the output voltage for R, G or B with the help of a matrix switcher. Three chip cameras do not supply composite SVHS or component signals but also an uncoded RGB signal. In this camera separate CCD is used as an image sensor for each of the red, green and blue image parts. A color separation system consisting of a prisms or dichroic filters separates the image into the basic R, G, and B components.
The three chips supply the output voltage corresponding to chrominance, color saturation and luminance. The RGB signal is fed, without any further encoding over three separate lines into an RGB monitor. Theoretically 3 chip cameras produce better image quality than single chip cameras. Many studies demonstrated no advantage of three chip cameras over a well-designed digitized single chip camera1 .
2.10 Human visual perception and clarity of image:
Cameras are either single chip or 3 chips. Single chip cameras supply a composite or super video home service (SVHS) signal are in widespread use. Color separation in single chip cameras is achieved by adding a stripe filter to the optical beam. Each of these filter stripes only accepts a definite color: red (R), green (G) and blue (B) on the definitive color combination principle. The luminance signal and the chrominance signals are generated from the output voltage for R, G or B with the help of a matrix switcher. Three chip cameras do not supply composite SVHS or component signals but also an uncoded RGB signal. In this camera separate CCD is used as an image sensor for each of the red, green and blue image parts. A color separation system consisting of a prisms or dichroic filters separates the image into the basic R, G, and B components.
The three chips supply the output voltage corresponding to chrominance, color saturation and luminance. The RGB signal is fed, without any further encoding over three separate lines into an RGB monitor. Theoretically 3 chip cameras produce better image quality than single chip cameras. Many studies demonstrated no advantage of three chip cameras over a well-designed digitized single chip camera1 .
The physical principles of video systems are based on the persistence of vision principle, which means that the retina of the human eye holds an image approximately 1/30 of a second (Snapshot) 4, 8 . Continuous series of still images faster than this produce a perception of motion picture.
Within the limits of pixels, scanning lines and dot pitch clarity of the image is a function of contrast, brightness, color balance and edge enhancement and it is measured as resolution. Brightness is the overall or average intensity of illumination and it determines the background level in the reproduced picture on the monitor screen. Contrast is the difference in intensity between the black and white parts. These parameters remain to be subjective. There is no tool to assess for assessing the perceptual impact of these physical measures. Jacob et al9 created a rating scale for seven dimensions of display characteristics these are contrast, detail, brightness, lighting uniformity, focus uniformity, color and sharpness. In his study he found this rating scale sensitive to degradation of image quality at video display edges. He recommended further study for refining this scale to create a psychometric to serve as a composite of perceptual quality in laparoscopy.
2.11 Future strategies:
Within the limits of pixels, scanning lines and dot pitch clarity of the image is a function of contrast, brightness, color balance and edge enhancement and it is measured as resolution. Brightness is the overall or average intensity of illumination and it determines the background level in the reproduced picture on the monitor screen. Contrast is the difference in intensity between the black and white parts. These parameters remain to be subjective. There is no tool to assess for assessing the perceptual impact of these physical measures. Jacob et al9 created a rating scale for seven dimensions of display characteristics these are contrast, detail, brightness, lighting uniformity, focus uniformity, color and sharpness. In his study he found this rating scale sensitive to degradation of image quality at video display edges. He recommended further study for refining this scale to create a psychometric to serve as a composite of perceptual quality in laparoscopy.
Current areas of investigation include micro endoscopes, 3 dimensional (3D) video endoscopy and head mounted video monitors1, 4, 8 However these systems have not yet been able to enter routine clinical use.
In one study, four micro endoscopes with a diameter ranging from 1.2 to 2.0 mm were compared8 . The study concluded that although these endoscopes offered the advantage of smaller wound, they have the inherent disadvantage of providing limited vision. The study further reported that the 5 mm conventional endoscope provided the smallest diameter without seriously compromising image quality. Never the less Scwaitzberg 8 described a micro endoscope with a wide angle of vision and higher availability of light to perform diagnostic laparoscopy and liver biopsy.
2.12 3D/Stereoscopic video:
In one study, four micro endoscopes with a diameter ranging from 1.2 to 2.0 mm were compared8 . The study concluded that although these endoscopes offered the advantage of smaller wound, they have the inherent disadvantage of providing limited vision. The study further reported that the 5 mm conventional endoscope provided the smallest diameter without seriously compromising image quality. Never the less Scwaitzberg 8 described a micro endoscope with a wide angle of vision and higher availability of light to perform diagnostic laparoscopy and liver biopsy.
Depth perception is complex and is based on two distinct groups of mechanisms. The first mechanism is depth perception in monocular vision which is very intuitive. It depends on depth cues like Relative size, overlapping, shade, color and movement analysis. Monocular depth perception is what we use during watching movies and in conventional laparoscopic surgery. The other group is binocular information. Our brain receives two sets of pictures from our eyes that are not identical in angle, and the minute differences in these pictures are processed at 3D picture in a specialized area in the visual cortex10 .
The basic mechanism of 3D camera system consists of two video cameras mounted on the tip of the laparoscope. Two separate image signals are captured and alternately transmitted to a monitor at high frequency. There are two different techniques for directing the correct images to its receptive eye without the other eye seeing it: “with glasses” and “without glasses”. The ‘with glasses” methods require the surgeon to wear an active eye ware made of liquid crystal glasses that receive the signal from an infrared transmitter. A shutter mechanism placed either on the eye ware (active eye ware) or in front of the monitor (passive eye ware) allows the surgeon to see the image of the perspective eye only. The cerebrum composes the two images as a 3D image. The without glasses technique uses lenticular lenses in front of the screen so that the right eye sees only the right eye image and the left eye sees the left eye image.
Several technologies are used to create 3D images with varying degrees of 3D effect together with their inherent advantages and dis advantages. To name without going into detail these are the dual channel video (used in the intuitive Da Vinci robot), the dual chip on the tip, the shutter mechanism and the “Insect eye Technology”10 .
Some studies have reported improved depth perception with 3D images and faster motor performance8 . Other studies failed to show this difference. More over with video endoscopy the image can be perceived only at a fixed focal point from the screen and there is little room for movement. To compensate for loss depth perception the monocular human eye uses a rich array of depth cues such as moving parallax, relative position, accommodation and familiar size.
The head mounted displays (HMD) consists of liquid crystal head mounted video display with an input cable from the laparoscopic camera and an associated power pack which can be placed on the back of the surgeon’s scrub shirt1, 8, 10. Head mounted displays allow an unobstructed view as the operative field is in constant view irrespective of the postural stance of the surgeon in the operating room. This permits good alignment of the visual and motor axes and avoids neck strain. The head mounted display gives good initial subjective impression, but an experimental study using a 3D monitor and head mounted display failed to show any improvement in task performance 1 . In one initial report by W. P. Geis11, HMD was used by the surgeon to perform 74 complex procedures. In this report the HMD allowed increased subjective concentration without subjective muscle strain for as long as 640 minutes. Further research is needed to show any improvement of this method on task performance. A disadvantage of this system was that it caused some surgeons to experience nausea8 .
2.13 Monitor position in laparoscopic surgery :
The basic mechanism of 3D camera system consists of two video cameras mounted on the tip of the laparoscope. Two separate image signals are captured and alternately transmitted to a monitor at high frequency. There are two different techniques for directing the correct images to its receptive eye without the other eye seeing it: “with glasses” and “without glasses”. The ‘with glasses” methods require the surgeon to wear an active eye ware made of liquid crystal glasses that receive the signal from an infrared transmitter. A shutter mechanism placed either on the eye ware (active eye ware) or in front of the monitor (passive eye ware) allows the surgeon to see the image of the perspective eye only. The cerebrum composes the two images as a 3D image. The without glasses technique uses lenticular lenses in front of the screen so that the right eye sees only the right eye image and the left eye sees the left eye image.
Several technologies are used to create 3D images with varying degrees of 3D effect together with their inherent advantages and dis advantages. To name without going into detail these are the dual channel video (used in the intuitive Da Vinci robot), the dual chip on the tip, the shutter mechanism and the “Insect eye Technology”10 .
Some studies have reported improved depth perception with 3D images and faster motor performance8 . Other studies failed to show this difference. More over with video endoscopy the image can be perceived only at a fixed focal point from the screen and there is little room for movement. To compensate for loss depth perception the monocular human eye uses a rich array of depth cues such as moving parallax, relative position, accommodation and familiar size.
The head mounted displays (HMD) consists of liquid crystal head mounted video display with an input cable from the laparoscopic camera and an associated power pack which can be placed on the back of the surgeon’s scrub shirt1, 8, 10. Head mounted displays allow an unobstructed view as the operative field is in constant view irrespective of the postural stance of the surgeon in the operating room. This permits good alignment of the visual and motor axes and avoids neck strain. The head mounted display gives good initial subjective impression, but an experimental study using a 3D monitor and head mounted display failed to show any improvement in task performance 1 . In one initial report by W. P. Geis11, HMD was used by the surgeon to perform 74 complex procedures. In this report the HMD allowed increased subjective concentration without subjective muscle strain for as long as 640 minutes. Further research is needed to show any improvement of this method on task performance. A disadvantage of this system was that it caused some surgeons to experience nausea8 .
One of the key problems in laparoscopy is the ergonomic positioning of the monitor. Due to video transmission during minimal access surgery the familiar three dimension site is lost. Orientation is therefore significantly reduced. The lever action of instruments make them pivot around a fixed point in the anterior abdominal wall. This makes the instruments to move reciprocally to the opposite direction. For example when you move the instrument handle to the right the instrument moves to the left and vice versa. The orientation becomes even more difficult when the instrument, camera and monitor are not oriented in one direction. The position of the monitor is important not only for orientation, but also for the working position of the surgeon. Usually the monitor is standing in an instrument tower without adjustable height. Small surgeons will look up to the monitor while tall surgeons can orient themselves horizontally. In some instance the surgeon has to operate with monitor to one side instead of looking directly in front of the operative field. Because of all of the above mentioned the surgeon frequently find difficulty to orient himself and coordinate his movement12. Furthermore the detection of technical problems such as colliding instruments, distorted tubes and cables and leaks due to open valves may be delayed. This will prolong the operative time and the procedure becomes more strenuous for the operating team than conventional surgery. U. Marten et al12 studied task performance and muscle strain of subjects in relation to monitor position. Three monitor positions were tested, frontal at eye level (A), frontal in the height of the operating field (B) and 45 degrees to the right side at eye level. He found placement of the monitor positioning at eye level is most preferable with regard to EMG activity of neck muscles. The monitor position at the side was not advisable.
2.14 Dedicated Minimal Access Surgery Suits :
At the beginning of the laparoscopic revolution, most of the procedures were cholecystectomies. Soon the laparoscopic approach was applied to the removal of stones from the common bile duct, herniorrhaphy, appendectomy and hence to more advanced surgical procedures such as anti-reflux procedures, splenectomy, colectomy, the management of morbid obesity and the removal of solid organs. Laparoscopic surgery has now expanded to include several other disciplines such as thoracic surgery and urology. As more advanced laparoscopic procedures are included along with mandatory need for new complex equipment with its space occupying monitors, video equipment, wiring, tubing and cords , this has led to increase OR turnover time and decreasing OR efficiency. The concept of designated minimally invasive surgery (MIS) suites was introduced in1993. It involves Monitors and video equipment integrated within the OR on ceiling mounted columns and having their controls on a centralized nursing station. T. A. G. Kenyon et al from Portland 13 demonstrated in an experimental study that the use of MIS suites reduced video set up and put away significantly, with the potential for significant associated cost savings. They believe that this provides just one justification for the high cost of the building of such ORs in the future.
3.1 RESEARCH METHODOLOGY 3.2 JUSTIFICATION FOR THE STUDY :
This study was justified by the fact that the distance and location of the image displayed on the monitor screen did affect the efficiency of task execution in minimal access surgery. It also carried direct impact on the surgeon by producing musculoskeletal injury and ocular discomfort. This compromised patient safety and affected the well-being of the surgeon.
3.4 MATERIAL AND METHODS:
20 physicians with no previous experience in laparoscopic surgery will participate in this study. Background data of the participants will be collected including gender, age, hand dominance, corrected vision defects, previous or current neck pain. Subjects with uncorrected vision defects and untreated neck problems will be excluded from the study. 10 mm diameter Beads placement task, in a laparoscopic trainer box will be used. This task requires depth perception and manual dexterity. Participants should use their dominant hand to perform the test. The test will be repeated at 3 monitor distances; Dx2, Dx3 and D4, where D is the diameter of the monitor. The monitor will be placed co-axially in front of the participants with a down gaze of 10-15◦ . The manipulation angle will be 60◦ . The table height will be adjusted to achieve elevation angle of 15 to 30◦4 .
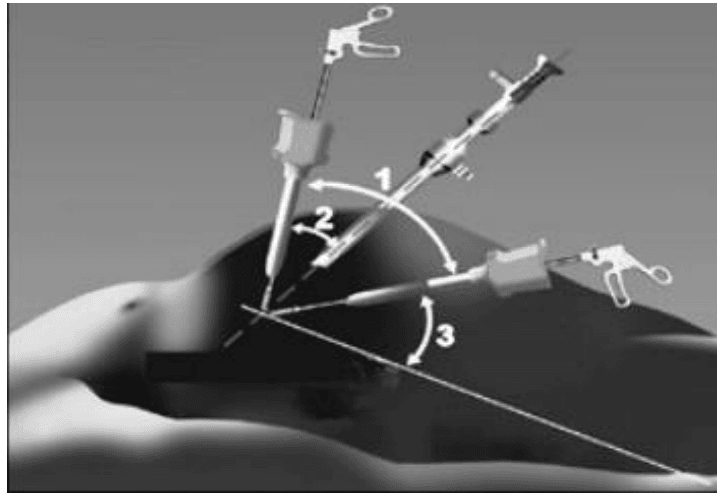
Fig: 3.1: manipulation angle (1), azimuth angle (2) and elevation angle (3).
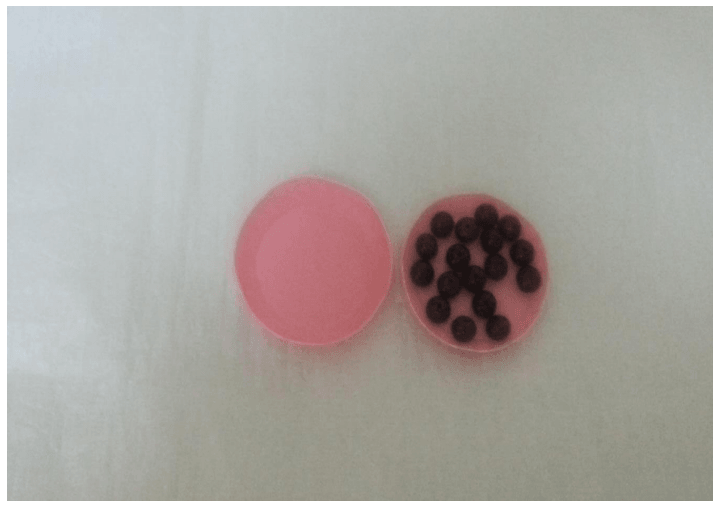
Figure 3.2: Beads transferred from the first plate to the other using grasper
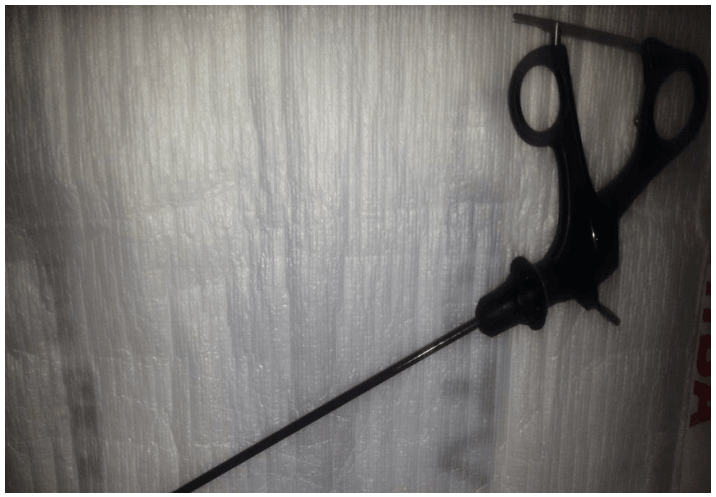
Figure 3.3: Grasper used for the beads transfer.
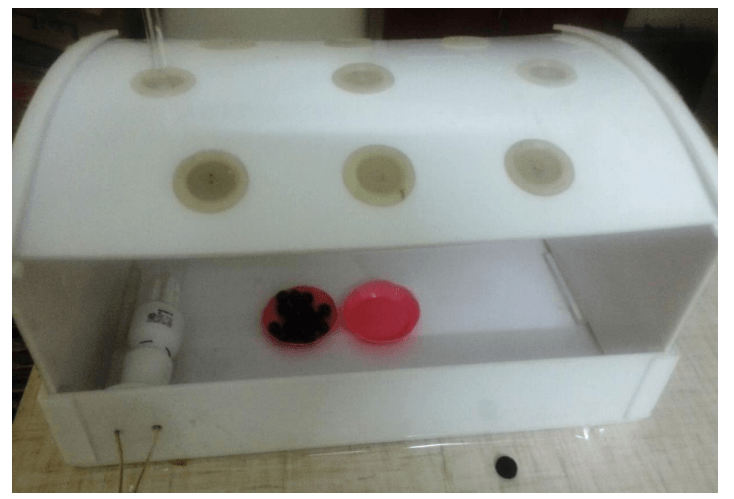
Figure 3.4: Pelvi-trainer used for the experiment.
Figure 3.5: Toshiba LED 32 Monitor
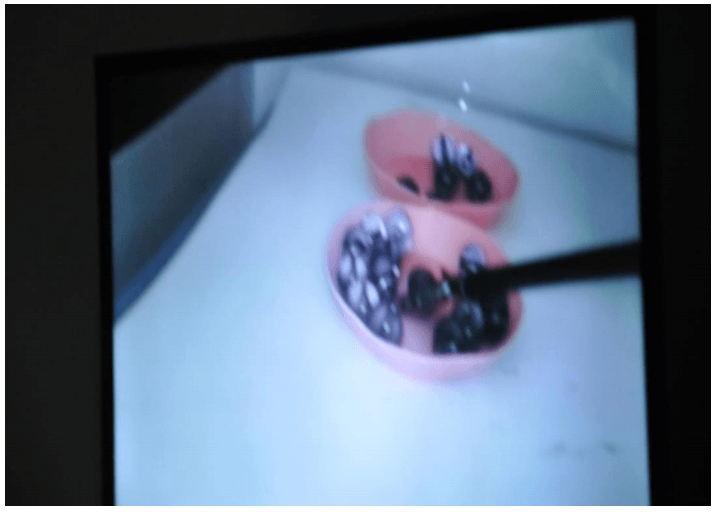
Figure 3.6: Beads Placement
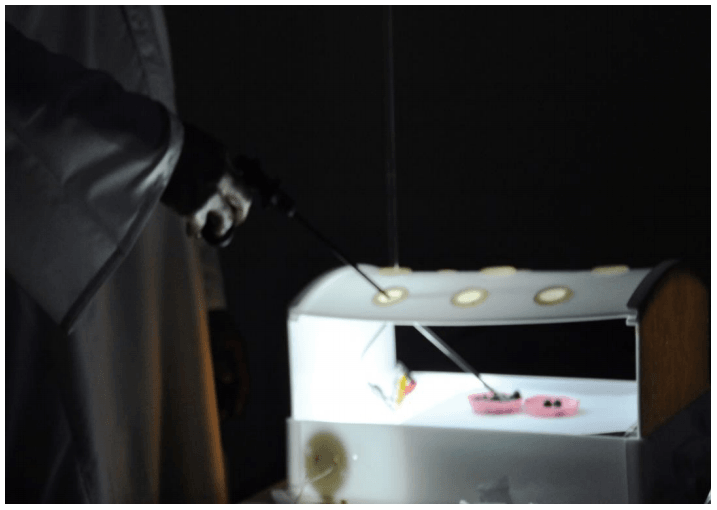
Figure 3.7A: maintaining optimum manipulation angle, elevation angle, azimuth angle and dimming of room light.
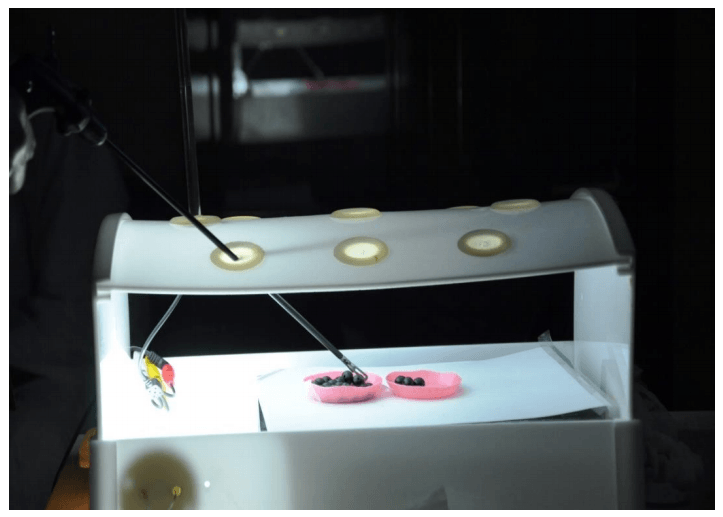
Figure 3.7B: Ergonomics of beads transfer
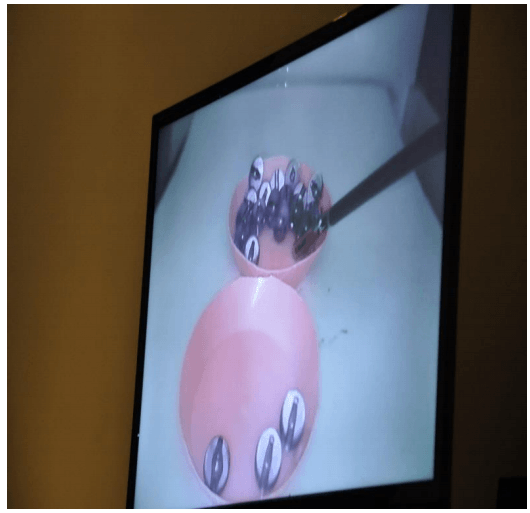
Figure 3.8: High quality Image
Informed Consent
I hereby admit that : 1. I’m participating in this Experiment titled: The Impact of Monitor Distance on Task performance with my own will.
2. All the steps and stages of the study have been explained to me.
3. I have understood all the steps and the stages of this study.
4. I have been informed that this study is carried out for pure learning purpose as thesis for fulfilling Master’s degree requirements for
Awadalla Musa Abbakar Matar .
Date: ……………………………………. Place: ………………………………………………….
Name: ……………………………………………………………………………………………………
Signature: ……………………………………………………………………………………………...
Figure 3.9: Participant informed consent form
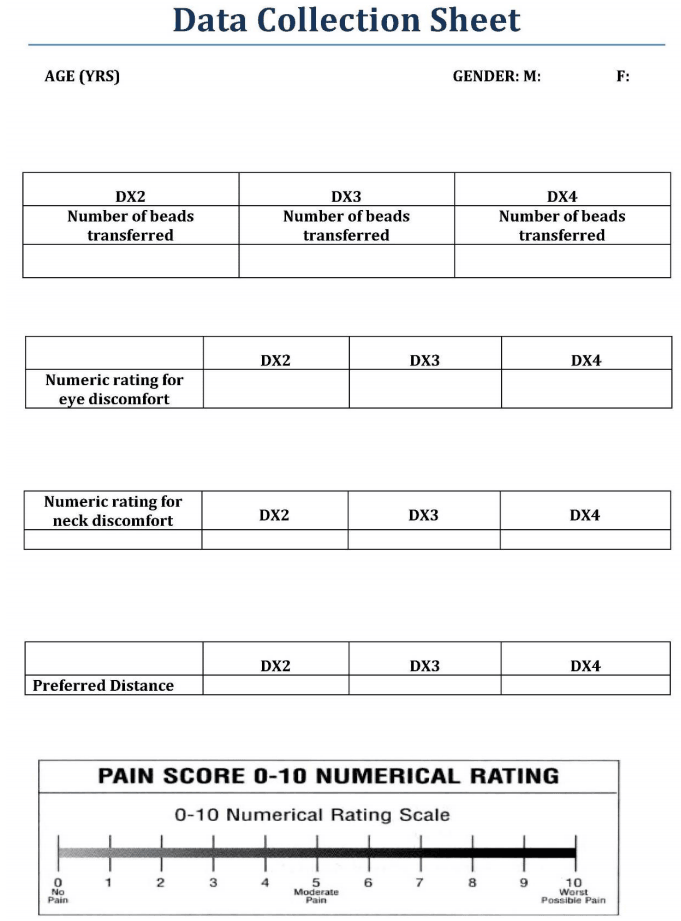
Figure 3.10: Data Collection Sheet
A high resolution image display system, Toshiba LED TV 32 inch monitor will be used. The trainer box used with its HD digital camera and grasper) are from RAN SURGICAL. The number of beads placed correctly will be taken as an indicator of task performance (dropouts will not count).
Data was collected in a predesigned sheet including three sections:
A. Background data about the participant including age and gender.
B. The Experiment
C. Numeric rating scale for eye and neck discomfort
3.5 THE STUDY AREA:
This study was conducted in Al-Bijadiyah General Hospital and Al-Quayiyah General Hospital. Both hospitals are in Riyadh Area, Saudi Arabia. The first hospital is a 50 bed hospital. The second one is a 200 bed hospital with laparoscopy facility.
3.6 SAMPLE SIZE AND STUDY POPULATION:
20 physicians from the fields of surgery and gynecology participated in this experiment. The participating physicians didn’t have any previous experience in laparoscopic surgery.
3.7 ETHICAL CONSIDERATIONS:
Consent from the hospital research committee was obtained. The reason for conducting the study was explained to all participant physicians. All the stages of the experiment were thoroughly explained. A signed informed consent was obtained.
3.8 LIMITATIONS OF THE STUDY:
The study was a small scale including 20 subjects as sample size. The exclusion criteria of subjects with untreated neck or eye problems were performed in a subjective manner. The rating of pain and eye discomfort was also subjective. The task performed (beads transfer) requires depth perception and manual dexterity, but less precision compared to other laparoscopic tasks e. g. a cutting, threading or suturing task.
3.9. CONFLICT OF INTEREST:
The author declares no financial gain or common interest with any commercial body.
4.1 Results
4.2 Statistical Analysis
4.3 Introduction :
There were 20 subjects in this study. There are three monitor distances: DX2, DX3, and DX4. For each type of monitor distance, the following data were collected, number of beads transferred, rating for eye discomfort, and rating for neck discomfort. The rating of discomfort ranges from 0 to 10, with 0 = no pain, 5 = moderate pain, and 10 = worst possible pain. In addition, for each subject, information regarding gender, age, and preferred monitor distance was also collected.
The statistical analysis was conducted against the background of the following 9 categories:
1. Relationship between preferred distance and eye and neck discomfort. (p values)
2. Relationship between bead count and the 3 monitor distance. (p values)
3. Relationship between bead count and eye and neck discomfort. (p values)
4. Age distribution of participants (10 year intervals) and standard deviation
5. Sex distribution (1 = male, 2 = female)
6. Graphic presentations for bead counts for the three distances
7. Graphic presentations of monitor distance, bead count and discomfort scores for the three distances and pain scores in relation to the 3 distances
8. Relationship between age /sex and bead count
9. Relationship between Age/sex and eye and neck discomfort.
10. Any other relevant statistical relations.
4.4. Methods : In this section, analysis methods used for each objective are discussed. All data analyses were conducted using SPSS14 .
4.5 Methods for objectives 4, 5, 6, and 7.
Objectives 4, 5, 6, and 7 are as follows:
4. Age distribution of participants (10 year intervals) and standard deviation
5. Sex distribution .
6. Graphic presentations for bead counts for the three distances
7. Graphic presentations of monitor distance, bead count and discomfort scores for the three distances and pain scores in relation to the 3 distances.
Descriptive statistics, such as mean, standard deviation (SD), minimum, and maximum, were used for age, bead counts, and ratings of discomfort of eye and neck. Histograms, bar charts and box plots were used to present the distribution of each continuous variable, including age, bead counts, and ratings of discomfort of eye and neck. For gender, bar chart and frequency table were used.
Objectives 2, 3, 8, and 10 are as follows:
2. Relationship between bead count and the 3 monitor distance. (p values)
3. Relationship between bead count and eye and neck discomfort. (p values)
8. Relationship between age /sex and bead count
10. Any other relevant statistical relations. The dependent variable was bead count. The independent variables were monitor distance, rating of eye discomfort, rating of neck discomfort, age, sex, and preferred monitor distance.
As the dependent variable, bead count, was measured three times for each monitor distance, for each subject, the three bead counts for each subject were related. A model that takes into account the correlation of the observations within each subject is necessary. Linear mixedeffects models (LMM) were proposed to model the relationship between the dependent variable and the independent variables of interest. In general, a linear mixed-effects model is any model that satisfies15:
