Laparoscopic Cholecystectomy in Cirrhotic Patients
Dr. Shiv Bagchi MBBS MS FRCS (Edin) FMAS DMAS
ABSTRACT:
Any gastrointestinal surgery on Cirrhotic Patient is a challenging, quite formidable task for any surgeon especially Cholecystectomy due to increased risk of severe hemorrhage, higher morbidity, and mortality, post-operative infection, longer hospital stay.
After reviewing various journals on Cholecystectomy in cirrhotic patients, the essence of all the articles suggests it is a challenging task to operate on Cirrhotic patients, Laparoscopic Cholecystectomy or Open Cholecystectomy, mainly due to Intraoperative and Postoperative hemorrhage.
According to authors of various articles published recommend Preoperative INR (International Normalised Ratio) and Platelet Count is more important to anticipate bleeding diathesis preoperative and postoperative, shorter convalescence period than Child-Pugh Classification or MELD Score( Model of End-Stage Liver Disease. Child-Pugh Classification or MELD Score is important for Morbidity and Mortality. Cirrhosis, Hepatocellular failure, Portal hypertension enhances the risk of postoperative complications in gastrointestinal surgery especially Biliary surgery. Reviewing relevant articles it seems Laparoscopic Cholecystectomy ( L.C) is a relatively safer procedure than Open Cholecystectomy ( O.C.) especially Child-Pugh Classification A & B. Gall stones are more common in Cirrhotic Patients, three times higher than non -cirrhotic patients. L.C. has a definitive advantage over O.C.'s shorter convalescence period and hospital stay. Acute Cholecystitis is more common in Cirrhotic patients. Emergency operation carries higher mortality, higher morbidity in comparison to elective surgery for Cholelithiasis.
There is no ambiguity, Laparoscopic Cholecystectomy (L.C) is a relatively safer procedure than Open Cholecystectomy (O.C. ). Laparoscopic Cholecystectomy is a better option due to the magnification of intraabdominal organs, target tissues and applying newer devices like Ultrasonic Shears, the use of Harmonics Scalpel (H.S.). Fibrin Spray will reduce intraoperative and postoperative bleeding, better hemostasis in cirrhotic patients despite Coagulopathy in cirrhotic patients. It is a fact Laparoscopic Cholecystectomy (L.C) has a higher conversion rate to Open Cholecystectomy(O.C.)
INTRODUCTION
The operation of Cholelithiasis in Cirrhotic patients is a high-risk procedure. In the past surgeons were reluctant to operate on cirrhotic patients due to high morbidity and mortality. Intraoperative and postoperative hemorrhage due to coagulopathy was one of the major factors. In the past some of the anesthetic agents were hepatotoxic.
With the advent of Laparoscope, with Ultrasound Shears i.e. Harmonics Slalpel (H.S.) Laparoscopic Cholecystectomy (L.C.) in cirrhotic patients has become a safer option.
.
Preoperative assessment of coagulopathy i.e INR and Platelet Count is paramount important for the successful and safer outcome of Laparoscopic Cholecystectomy(L.C.). MELD Score { Model of End-Stage of Liver Disease ) and Child-Pugh Classification can predict reasonably morbidity and mortality following Laparoscopic Cholecystectomy (L.C.) in the cirrhotic patient. Most of the published data regarding Laparoscopic Cholecystectomy(L.C.) in cirrhotic patients suggest it is safe and effective than open cholecystectomy (O.C.) in the cirrhotic patient which can cause high morbidity, high intraoperative and postoperative bleeding, wound infection and high mortality. Patient selection is vitally important before L.C.in cirrhotic patients. According to published papers MELD Score below 13, Child-Pugh class C carries high mortality and morbidity in any type of operation for Cholelithiasis.
According to published papers, only symptomatic Gall Bladder disease should undergo an operation.
MATERIALS and METHODS:
Review of literature from the year 2006 to 2017 was carried out at least 35 articles from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), Google Search, PubMed, Cross-references, reading the title articles. I have selected 30 articles which are well documented, authentic with comparable data. After going through the articles I have analyzed the demographics, indications of Laparoscopic Cholecystectomy(L.C), the incidence of perioperative and postoperative complications, duration of hospitalization, morbidity, and mortality in L.C. vs Open Cholecystectomy(O.C) in cirrhotic patients.
Laparoscopic Cholecystectomy (L.C) started in the 1980s. Previously Cholecystectomy in cirrhotic patients deemed risky and fatal. Since the introduction of Laparoscopic procedure, modern instruments and devices for L.C. seem relatively safer than open cholecystectomy (O.C) in cirrhotic patient especially Child-Pugh classification A and B.
The number of patients who had undergone L.C. for cholelithiasis in cirrhotic patients varies from center to center as per publication in surgical endoscopic journals. It ranges from 2005 patients to 21 patients as per published articles. Rafael Pinheiro in 2017 published paper where he and his associates did Laparoscopic Cholecystectomy (L.C) in 2005 patients with cirrhosis over the years. According to SAGES publication113 patients had L.C. who had cirrhosis between 1995-2006. Spiros Delis in June 2009 published data with 220 patients with cirrhosis who had undergone L.C. Masayuki Akita et all performed L.C. in 21 patients with cirrhosis. Abdul Shaikh et all performed L.C. in 250 patients with cirrhosis, published a paper in the year 2009. Some centers did a statistical analysis of L.C. in cirrhotic patients using CHI Square, WILCOXON rank-sum.
There are centers where Harmonics Scalpel (H.S.)was used than the traditional method for L.C. ie clips for cystic duct and artery, diathermy for gall bladder bed dissection. Ayman El Nakeeb et all published paper in the year 2009 where H.S. was used in 60 patients for L.C. in cirrhotic patients. Abid Khalid et all performed 350 laparoscopic cholecystectomies in cirrhotic patients, published the data in the year 2016. Chinasammy et all feel safer L.C. in 265 cirrhotic patients using traditional method i.e. clips and diathermy. Luigi Boni et all in 2015 published an article using Indocyanine Green (ICG ) enhanced Fluorescence in Laparoscopy Cholecystectomy(L.C) in 52 patients with cirrhosis.
Overall data shows the majority of cirrhotic patients with symptomatic gall bladder disease who had undergone Laparoscopic Cholecystectomy (L.C) were Child-Pugh Classification Aand B. Very few with C type who had L.C. showed higher morbidity and mortality.
RESULTS:
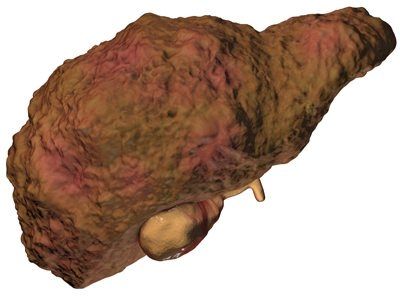
Cirrhosis of the Liver is a serious nature of pathological disorder the Laparoscopic Cholecystectomy (L.C) in symptomatic Cholelithiasis is a safer procedure especially Child-Pugh Aand B, provided INR and Platelet count is within the normal range.
Laparoscopic Cholecystectomy (L.C) in cirrhotic patients causes less intraoperative and postoperative bleeding, less morbidity less mortality, less incidence of postoperative infection, reduced period of hospital stay and early feeding in the postoperative period.
According to the published paper, HarmonicsScalpel (H.S) has more advantages than standard use of Clips and Diathermy in L.C.(El Nakeeb et all 2010). Using H.S. causes less intraoperative bleeding, less gall bladder perforation, less incidence of conversion to Open Cholecystectomy (O.C) and reduced postoperative pain. Jorge M Mancero published a paper in the World Journal of Surgery (in 2008) 23 patients had cirrhosis with Child-Pugh A class 76.7%, B class 23.3%, all these patients had Laparoscopic Cholecystectomy (L.C). All of them undergone L.C. 6 of them with class B developed postoperative Ascites none in A-class, no conversion to Open Cholecystectomy (O.C) in either A or B class.
Another study published by Spiros Delis in June 2009, L.C. was performed in 220 patients who had cirrhosis with symptomatic Cholelithiasis between the year 1995-2008, Child-Pugh A and B both classes had symptomatic gall bladder disease, no death was reported. Intraoperative, Postoperative morbidity occurred in 19% of patients mainly bleeding, wound complications and intraabdominal collection.
Intraoperative bleeding in 19 cases(8.6%), O.C. conversion 12 cases out of 220 patients (5.4%), 22 patients needed postoperative blood transfusion F F P (Fresh Frozen Plasma). In essence MELD Score above 13 showed a higher complication rate postoperatively. Child-Pugh class did not predict morbidity or mortality effectively. It seems MELD Score predicts morbidity more accurately than the Child-Pugh classification system.
According to a published paper in 2009 by Spiros Delis surgeons should pay more attention to MELD Square regarding the predictability of intraoperative and postoperative complications, morbidity and mortality than Child-Pugh classification. Meld score recently introduced and used for the following :
1. To predict survival in cirrhotic patients receiving Trans Jugular Intrahepatic portosystemic shunt (TIPS)
2. To determine priority on the waiting list for a liver transplant
3. To predict the postoperative outcome of cirrhotic patients undergoing surgical procedures.
The MELD score was calculated by using the preoperative values of three laboratory tests: INR, Serum Creatinine and Total Bilirubin.
There was no significant result in MELD Score distribution with gender male or female or Liver cirrhosis etiology alcoholic or nonalcoholic. The article published by W.S.Cobb in the year 2005, 50 patients with cirrhosis ( 27 men and 23 women ) undergone L.C. for symptomatic cholelithiasis. 39 patients were Child-Pugh A, 10 patients were B, one patient class C. The rate of wound infection and wound bleeding were markedly low in those patients who undergone L.C. Evaluating 50 patients by WS Cobb et all who had cirrhosis, the average MELD score was 8.9. According to W.S.Cobb publication although he found L.C. technically challenging because of portal hypertension varies and Thrombocytopenia frequently coexists despite the challenges, advancement in Laparoscopic surgery can safely be performed in patients with mild to moderate cirrhosis of Liver (Child-Pugh A and B Classification). With thorough and proper management of coagulopathy low perioperative and postoperative morbidity, rapid convalescence is achievable for the high-risk groups of patients.
Another published data by Quillin RC et all in 2013 L.C. in 94 patients was carried out in cirrhotic patients with symptomatic gall bladder disease. The median Child-Turcotte-Pugh (CTP) score was 6 and the average MELD score was 11. The average length of stay in the hospital was 2.6 +4-3 days. The conversion rate was 11%. The conversion risk factors were: decreased albumin, increased MELD Score and blood loss. Morbidity occurred in 32 patients.
Predictor of morbidity increases in high INR, high CTP score and number of intraoperative RBC transfusion. Mortality occurred in 4 patients (4.2%). Masayuki Akita et all published paper in the year 2017. 21 patients with cirrhosis of Liver with symptomatic gall bladder disease had undergone L.C. and 74 patients had L.C. without cirrhosis. Despite the Child-Pugh Score being higher in cirrhotic patients, the MELD score was similar in the two groups. There was no difference in operative time or amount of blood transfused. Postoperative hospital stay and postoperative morbidity rates were marked by greater in the cirrhotic group. According to the author,s (Masayuki) opinion safety of Laparoscopic Cholecystectomy in cirrhotic patients are proven and confirmed. Due to the pathological process, the gall bladder is usually completely covered in cirrhotic liver, the French Style approach which allows surgeons more easy access to the gall bladder pocket is supposed to be one of the operative options which are a safer and pragmatic option.
Another study published by Chinnasammy Palanivelee et all in 2006, 265 patients with cirrhosis (Child A and B) with symptomatic gall bladder disease had undergone L.C. between the year 1991 and 2005. The mean operative time in the subtotal cholecystectomy group was 72 minutes, in the standard group was 41 minutes, no mortality reported. 15% of patients postoperative deterioration of Liver function occurred worsening Ascites, port site infection, port site bleeding, intraoperative bleeding and increased bile drainage.
According to Chinnasammy, the author L.C. is a safe and effective treatment for calculous cholecystitis in cirrhotic patients. appropriate modification of subtotal cholecystectomy should be practiced, depending on the risk factors present it is advisable to avoid complications.
Data published by Sleeman et all in 1998 in the Journal of the American college of surgeons. 25 patients with L.C. procedures were carried out in cirrhotic patients from May 1992 till July 1996. There was no mortality in their group. All procedures were successfully performed by L.C., mean length of hospital stay was 1.7 days. Morbidity is consistent with wound hematoma, pneumonia and Ascites(32%) of cases postoperatively. According to Sleeman et all L.C. can be safely be performed in cirrhotic patients with all well-compensated Liver function.
DISCUSSION:
Any abdominal surgery in cirrhotic patients is technically difficult, risky undertaking especially Child-Pugh C, MELD Score over 13, high INR, low Platelet count, coagulopathy which is invariable findings in cirrhotic patients. Open cholecystectomy (O.C. ) in cirrhotic patient carry higher morbidity and mortality, higher incidence of post-operative infection, longer hospital stay. Intraoperative bleeding, postoperative bleeding is a major concern. Cholelithiasis in cirrhotic patients occurs more frequently 3 times more than the general population.
A review of 4895 autopsy records in the literature showed gall stones 29.4% of patients with cirrhosis than 12.8% in noncirrhotic patients. The possible cause of high incidence of gall stone in cirrhotic patients due to intravascular hemolysis, with slowing down of gall bladder emptying and mobility. Reviewing various literature 7-20% mortality and 5-25 % morbidity associated with gall bladder removal in cirrhotic patients are noted. Due to high mortality and morbidity surgeons should carefully think and assess the patient's condition before embarking on cholecystectomy. Cholecystectomy in cirrhotic patients considered as formidable operation. Patients with significant coagulopathy and portal hypertension cholecystectomy should be avoided except in a dire emergency.
Several studies show Laparoscopic Cholecystectomy (L.C. ) in a cirrhotic patient can be safely performed. Preoperative management, patient selection is essential. Child-Pugh A & B, compensated Liver function, normal INR, normal Platelet count, MELD Score below 10 is a good predictor of successful operation, less mortality, and less morbidity. With the advent of new technology ultrasound scan (u/scan ) CAT Scan, preoperative endoscopy can assess the state of Liver failure and cirrhosis of Liver, portal hypertension. Laparoscope also magnifies the operative field, anatomy of biliary and structure, gall bladder bed in case of hemorrhage and portal hypertension.
Using harmonics or ultrasound shears helps to reduce intraoperative bleeding. Pneumoperitoneum during laparoscopy reduces the venous pressure less risk of severe bleeding using harmonics scalpel has definite advantages over clips and it should be Bipolar than Monopolar due to local tissue damage, burn to bowel, remote injury. Using laparoscopy any collection of blood can be easily visualized and any arterial bleeding can be controlled. Laparoscopic cholecystectomy should be performed in symptomatic cholelithiasis patients.
In Child-Pugh C class it is riskier to do either L.C. or O.C. The subcostal incision for O.C. has high risk in cirrhotic patients. Possibility of severe hemorrhage wound infection and delayed wound healing .O.C. has a higher risk of bleeding due to coagulopathy, sepsis, increased morbidity and mortality in Child-Pugh class A and B. Reviewing various literature about L.C. in cirrhotic patients. It seems L.C. is effective, low incidence of intraoperative and postoperative complications, less mortality and less morbidity. first and foremost important is patient selection. There are few parameters that are paramount importance to remember INR, Platelet count, Child-pugh classification, MELD Score, state of Liver failure, portal hypertension. Some centers published data in cirrhotic patients who had undergone L.C. mortality was 10%. in Child-Pugh A class, 30% in B, 82% in C class.
Regarding the operative technique in L.C. place of Port insertion is important. It is advisable to avoid unilateral port in cirrhotic patients due to porta-vena cava shunt using harmonics scalpel reduces the chances of bleeding especially severe adhesions around Callot's Triangle, subtotal cholecystectomy or aspiration of the gall bladder is a safer procedure in case of dense adhesions around Callot's Triangle.
Using Fibrin glue or spray reduces the oozing from the gall bladder bed. Besides Fibrin glue and harmonics scalpel there is a wide variety of bleeding control devices are sold in the market i.e, Tissue -Link, Enseal offers reasonable control of bleeding during dissection of structure and detachment of gall bladder from Liver bed. L.C. provides lower morbidity, reduced operative time, earlier feeding postoperative period, less need for blood transfusion, reduced hospital stay in comparison with O.C. In comparison with the noncirrhotic patient has a higher conversion rate, increased operating time, higher bleeding complications and higher overall morbidity compared with the patient without cirrhosis who had undergone Laparoscopic Cholecystectomy(L.C.)
In 2003 Puggioni and Wong conducted a meta-analysis that included studies of cirrhotic patients submitted Puggioni and Wong about Laparoscopic Cholecystectomy(L.C.), six of patients were cirrhotic and six of them were non-cirrhotic. Puggioni and Wong concluded that although L.C. is a safe procedure for cirrhotic patients, they had a higher rate of conversion to O.C. longer surgery time, more severe bleeding and higher morbidity than noncirrhotic patients. The potential complications of L.C. are damage to the umbilical vein. Trocar should be placed to the right or left of the median line under direct vision to avoid complications. Traction of the gall bladder should be exercised with caution as well as dissection of the Liver, where vessels may be relatively large.
Preoperative imaging with CAT Scan or MRI is important to identify abdominal varices on the abdominal wall. Insertion of the first trocar should be infraumbilical . An experienced surgeon and anesthetist are paramount importance for the proper safe management of cirrhotic patients.
The " Hepatic Arterial buffer response" is impaired in cirrhosis of the Liver. The pressure generated by pneumoperitoneum slows down the hepatic flow in the Liver, which can cause further damage to hepatic cells in cirrhotic patients. To minimize Liver damage using the lowest possible intraabdominal pressure(IAP) that provides good visualization. To minimize Liver damage especially longer operative time, a short period of insufflation every 2 to 3 hours it will reduce the adverse effects on hepatic perfusion may be safer and wise pragmatic steps to take. Bleeding complications are a major cause of adverse outcomes after surgery for patients with Liver cirrhosis and Liver damage. Prothrombin is produced only by the parenchymal cells of the Liver. In reality, its half-life is only 2 days it is a good pointer of hepatocellular decompensation. Several studies have shown Prothrobmin time (P.T)and Partial Thromboplastin time to be a more reliable prognostic indicator. Correcting Coagulopathy and Thrombocytopenia preoperatively is vitally important.
Portal hypertension can be a major concern in L.C.Vascular staples (2mm)to control vascular hilum if indicated, it will reduce blood loss, shorter hospital stay, and fewer wound complications. The laparoscopic procedure reduces the exposure of bloodborne pathogens as compared to open technique(O.C. ) Half of the cirrhotic patients may carry Hepatitis B and C. Many of these patients need Liver Transplant in the future. L.C. surgery may benefit in reducing the severity of postoperative adhesion formation in those patients.
The major difficulties surgeons face during L.C. surgery are the following :
1.Adhesion with new blood vessel formation( Neovascularization)
2. Difficult retraction of the Liver.
3.Inadequate exposure of Callot's Triangle
4. Risky gall bladder bed
5.High-risk Hilum.
The experienced surgeons who have performed numerous L.C. in cirrhotic patients have advised the following safety tips :
Due to the umbilical vein, the recanalization umbilical port should be created away from Falciform ligament. The Liver parenchyma is hard and fibrotic difficult to retract. The retractor should be applied to the body of the gall bladder, just above infundibulum to expose the Callot's Triangle. Rotating Trocars positions to the right If Callot's Triangle not exposed properly then the fundus first method should be used. Bipolar electrosurgery is safe, pragmatic, more useful in cirrhotic patients. Bipolar works more efficiently than the Monopolar instrument to coagulate bleeding area in gall bladder bed and hepatic parenchyma. Harmonics Scalpel (H.S.) or advanced Bipolar devices are helpful especially dissecting peritoneal adhesions. Argon Beam coagulation and Thrombin Spray may also be useful for hemostatic dissection. Minimal blunt dissection is recommended Before completing L.C. all necessary ports should be thoroughly checked for bleeding. All the accessory ports should be closed meticulously even small port 5mm or 3mm.
The separation of the gall bladder from the Liver bed may be difficult and the source of massive bleeding when tortuous, dilated vessels occur in the gall bladder bed. In such cases, the posterior wall may be left intact with the Liver and the remnant either by mucosectomy or by electromigration i.e. Laparoscopic subtotal Cholecystectomy (LSC). LSC type I, II, III can be performed assessing the situation. The use of Harmonics Scalpel (H.S.) markedly reduces bleeding complications in L.C.
Indocyanine Green (ICG )enhanced Fluorescence has possible clinical application in L.C. to improve the view and provide detailed anatomical information during surgery especially where anatomy in Callot's Triangle is blurred, ICG will help for safe L.C.
ICG makes blood vessel and bile duct more prominent looking, delineate the cystic duct, CBD, the cystic artery and hepatic artery. ICG should be injected 45 minutes before the L.C. procedure.
Patients with cirrhosis undergoing nonhepatic surgery have reported mortality in the literature that may be as high as 45%. Over the years surgeons were often reluctant to operate on cirrhotic patients due to the possibility of developing acute or chronic Liver failure especially of anesthetic agents used which could be hepatotoxic also of surgical trauma. The use of less hepatotoxic agents has reduced the risk. The usual risk indicators are Child-Pugh class C, presence of portal hypertension, ascites, encephalopathy, infection, anemia, malnutrition, jaundice, hypoalbuminemia, hypoxemia and Prothrombin Time(P.T.) not resolved by VitaminK or Fresh Frozen Plasma (F FP). The mortality rate of Cholecystectomy is related to the severity of underlying Liver Disease.
The gastrointestinal surgery in cirrhotic patients known to be associated with immense technical difficulty and increased morbidity and mortality. Cirrhosis is a major key intraoperative finding that magnifies the surgical difficulties in L.C. Meta-Analysis of six studies comparing L.C. in cirrhotics and non-cirrhotics patients reported higher conversion rate to open procedure(O.C. )7.06% Vs 3.64 P=0.0237, Odds ratio:1.085-3718, longer operative time 98.2 minutes Vs 70 minutes P=0.00467, Confidence interval(CI): 1.085-3718, increased intraoperative bleeding complications 26.4% Vseve 3.1% P=0.001. The blood loss ( 105.6Vs 35.2ml). Increased overall morbidity 20.86% Vs 7.99% P=0.001.
No statistical difference found regarding wound infection incidence and death. The length of hospital stay was 5.4 Vs 3.5 days. More cirrhotic patients went through emergency procedures for acute cholecystitis. The acute Cholecystitis was evident 47% of patients with cirrhosis Vs 14.7% without cirrhosis.
The Emergency Procedures in cirrhotic patients are associated with higher morbidity, longer postoperative hospitalization and sevenfold higher mortality comparison to elective surgery. According to a systematic review published, identified 2005 patients with cirrhosis undergone Laparoscopic Cholecystectomy(n=1756) and Open Cholecystectomy (n==249). General raw data showed that Laparoscopic Cholecystectomy (L.C. ) procedures compared to O.C. was associated with fewer post op[erative complications 17.6x47.7%, the fewer infection rate of 0.8%x2%. The conversion rate of L.C. was 5.8%. The prevalence of Child-Pugh class A, B, C of patients was similar between L.C. and O.C. L.C. group was A 76.6%, B 21.77%, C 1.59%and O.C. group A 67.2%, B 28.73% and C 4.02% respectively.
The most complications of L.C. found in large case series include postoperative worsening of Ascites 10.6%, Intraoperative bleeding 5.2%, Intraoperative collection 3.5%, pulmonary infection 1.75%, blood transfusion 1.1% and minimal incidence of wound infection. The overall conversion for L.C. in cirrhotic patients ranges from 4.75% to 5.8%. The reason for conversion includes difficulty in identifying anatomy, uncontrolled bleeding, massive intracavitary adherence, the need for common bile duct (CBD) exploration and suspected bile duct injury. It seems MELD Score assessment preoperatively is a more rational approach while considering Conversion from L.C. especially when MELD Score is higher than 14. Population base study Chmilac et all analysis of 2857 L.C. to 38.3 O.C. in cirrhotic patients in the U.S.A. showed uncontrolled bleeding may be a major problem during L.C.It may be caused by abdominal varices and coagulopathy secondary to a reduction of clotting factor synthesis and Thrombocytopenia. Therefore Fresh Frozen Plasma (FFP)and Platelets may be given preoperatively as well as activated recombinant factor VII (rFVII a).
Cholecystectomy in cirrhotic patients used to be an intervention operation procedure with major complications some were fatal. Series from 1980 report mortality rate was 25%, morbidity was 35%. Patient with cirrhosis undergoing Cholecystectomy mortality rate has gone down considerably last two decades due to Laparoscopic procedures(L.C.) Laparoscopic Cholecystectomy offers lower mortality, lower morbidity, shorter operative time, earlier feeding resumption, less need for blood transfusion and reduced hospital stay compared with open cholecystectomy.
Better results are achieved by the following :
1. Magnification of the surgical field gives a clear vision to achieve hemostasis.
2.Suffered venous bleeding control with pneumoperitoneum.
3. Use of Harmonics Scalpel (H.S.) and Laparoscopic ultrasound.
A meta-analysis conducted in 2003 showed that L.C. in cirrhotic patients had less blood loss during operation shorter hospital stay compared with open Cholecystectomy (O.C. ). L.C. performed in cirrhotic patients was associated with a high conversion rate, increased operating time. higher bleeding complications and higher overall morbidity compared with the patient without cirrhosis who received Laparoscopic Cholecystectomy (L.C). Irrespective of better results regarding mortality, reported morbidity remains high. Preoperative prediction of expected post-operative morbidity would be of significant value for preoperative decision making.MELD Score has been used not only for portosystemic shunt and transplanted procedures but also for cardiac and general surgical procedures as well, focussing mainly on the ability of MELD Score to predict mortality.
Cirrhotic patients are operated late in course of their gall bladder disease, present late with severe chronic cholecystitis. Therefore the gall bladder tissue is often woody and friable, hence more extensive surgical dissection is one of the primary steps to surgical success in these patients. Perfect hemostasis is time-consuming in the coagulopathy group. Preoperatively when appropriate correction of coagulopathy was attempted with Fresh Frozen Plasma (FFP) and Vitamin K preinduction and platelets were given post induction as needed. Additional types of modalities can be applied including hemostatic agents such as oxidized cellulose (Gelfoam), Surgical, a topical hemostatic agent like FLoseal, application of ultrasound energy via Harmonics Scalpel (H.S.) All these applications in conjunction with mechanical compression from introduced surgical sponges. Surgical sponges are important for safer and successful surgery in these patients. Finally, a tremendous amount of patience is necessary because of conversion (O.C.)unable to control coagulopathy.
Patients with cirrhosis have a higher risk of postoperative complications. There is a greater risk of patients needing a postoperative blood transfusion, suggestive of increased bleeding tendency. Increased risk of bleeding in cirrhotic patients is due to various factors. In addition, portal hypertension generates Thrombocytopenia due to Hypersplenism and stimulates angiogenesis. The neovascularization in the abdominal wall and around the Liver hilum constitutes a major technical challenge when performing Cholecystectomy in cirrhotic patients. In some cases, percutaneous Cholecystectomy has been suggested for cholecystitis in patients with severe portal hypertension or with Liver cirrhosis grade Child-Pugh C class. Gall stone disease in cirrhotic patients three times higher than noncirrhotic patients. In terms of epidemiology, gall stone disease is a leading cause of hospital admission. The incidence of higher in cirrhotic patients due to changes both to the gall bladder and composition to bile. In most cases a patient with cirrhosis develops black pigmented stones due to increased concentration of unconjugated bilirubin, ionized Ca 2+ in the bile causing supersaturation in calcium bilirubin. Increasing Ca 2+ is due to mucin hypersecretion leading to defective acidification of bile and precipitation of Calcium. The disorder of vascular kinetics consists of hypomobility induced by wall edema and hormonal changes in the context of cirrhosis. Relaxing peptides such as VIP, Somatostatin and Glucagon.
Embarking surgery on the cirrhotic patients faced with certain restraint due to their fragile background and risk of decompensation that can be precipitated by surgery. As Cirrhosis of Liver progresses synthetic dysfunction ensues and cirrhosis becomes " Systemic Disease". Cirrhotic patients have a dynamic circulatory syndrome leading to increased cardiac output and decreased peripheral resistance. It is actually the state of heart failure hidden by decreasing afterload which compensates ventricular filling shortfall but it becomes apparent in conditions of physical or pharmacological stress so-called " Cirrhotic Cardiomyopathy".
Regarding the respiratory function, patients with liver cirrhosis have a degree of hypoxemia caused by ascending diaphragm due to increased abdominal pressure in presence of Ascites. The risk of pulmonary atelectasis is correlated with the presence of ascites and hydrothorax. Hepatopulmonary syndrome as severe functional decompensation of the two organs is characterized by the Triad: Liver failure, severe hypoxemia (PaO2 less than 70 mm Hg) and pulmonary shunts opening carry a very high mortality. Hepatorenal syndrome is a severe renal impairment due to an important reduction in rate given by vasoconstrictors which can be triggered by numerous factors including bacterial infection.
In addition coagulation disorder in cirrhosis deficiency in protein synthesis immune dysfunctions and the fact, these deficiencies increase with the progression of cirrhosis. It becomes obvious why practicing surgery in these patients requires a thorough preoperative evaluation and optimization of patients are blood loss, postoperative Liver failure, and sepsis that may cause a high rate of mortality and morbidity.
Laparoscopic Cholecystectomy (L.C.) has become Gold Standard in the treatment of benign disease of the gall bladder and expanded its indication inpatient with Liver cirrhosis, the major benefit is less traumatic and has lower mortality and morbidity associated with. The main reason the Laparoscopy Cholecystectomy (L.C.) does not require a large opening of the peritoneum and there is less risk of Ascitic fluid leak and sepsis.
CONCLUSION:
Incidence of Cholelithiasis( Gall Stone) three times higher in the cirrhotic patient than noncirrhotic patients. Cholecystectomy in the cirrhotic patients is a challenging formidable task for surgeons. Laparoscopic Cholecystectomy(L.C.) can be performed safely in selected patients with cirrhosis of Liver Child-Pugh class A and B who have symptoms of Cholelithiasis with acceptable morbidity.
The advantage of L.C. in comparison with Open Cholecystectomy (O.C. ) shorter operative time, reduced hospital stay.
Preoperative MELD Score, INR, Platelet Count predict reasonably intraoperative and postoperative complications, morbidity and mortality than the Child-Pugh classification system.
Patients with cirrhosis and cholelithiasis Laparoscopic Cholecystectomy (L.C.) should be performed. Patient with significant Portal Hypertension and severe Coagulopathy L.C. or O.C. should be Avoided, should be managed Conservatively also in Child-Pugh class C except for emergency situation. The patient should be assessed carefully before surgery. In Child-Pugh class, C in an emergency situation as acute Cholecystitis Percutaneous drainage of gall bladder would be a safer option. Any major procedure of whether O.C.or L.C. carries high mortality and morbidity.
L.C. also Protects surgeons and theatre staff exposure to viral infection Hepatitis B and C which is the major cause of Cirrhosis of Liver in patients. The surgeon with vast experience L.C. is a safer procedure in cirrhotic patient especially Child-Pugh class A and B. Laparoscopic Cholecystectomy (L.C.) should be the mainstay of operative procedure in a cirrhotic patient. The operative risk whether intraoperative and postoperative in cirrhotic patients depends on the degree of Preexistent Hepatic Dysfunction, nature of the procedure and Comorbid Conditions.
KEYWORDS:
Cirrhosis-Cholelithiasis-Laparoscopic Cholecystectomy-MELD Score-Child-Pugh classification-Morbidity-Mortality.
ACKNOWLEDGMENTS:
I am indebted to Professor R.K.Mishra and his team at World Laparoscopic Hospital, Delhi India for their guidance and advice regarding compiling this Review Article.
REFERENCES:
1. E. Cucinotta, S.Lazzara, G.Melita: Laparoscopic Cholecystectomy in Cirrhotic Patients, surgical endoscopy and other interventions. Surgical Endoscopy, December 2003( SAGES)
2. J.SCHIFF, M. Mishra, G.Rendon: Laparoscopic Cholecystectomy in Cirrhotic Patients: Surgical Endoscopy 2005 Sept19(9): 278-81 (SAGES)
3. A.M.Lacey, C.Balaguer, E.Andrade, J.C.Garcia-Valdecasas: Laparoscopic Cholecystectomy in Cirrhotic Patients: Surawis:
surgical Endoscopy (SAGES) 1995
4. C.N.Yeh, M.F.Chen, Y.Y.Jan: Laparoscopic Cholecystectomy in 226 Cirrhotic Patients: Surgical Endoscopy (SAGES)2002
5. Spiros Delis, Andreas Bakoyianis, Juan Madariaga, John Bramis: Laparoscopic Cholecystectomy in Cirrhotic Patients-The value of MELD Score and Child-Pugh classification in predicting outcome: Surgical Endoscopy( SAGES) 2010
6. Ayman El Nakeeb, Waleed Askar, Ramadan El lithy, Mohamed Farid: Clipless Laparoscopic Cholecystectomy using Harmonics Scalpel Vs Conventional Method in cirrhotic patients: J.Gastrointestinal Surgery 2010 Feb 14(2): 323-8
7. Hiroshi Saeki, Daisuke Korenaga, Hirohiko Yamaga, Kyotaro Mawatari: A comparison of Open and Laparoscopic cholecystectomy for patients with cirrhosis: Surgery Today, May 1997, Vol 27, Issue 5, PP 411-413
8. W.S.Cobb, B.T. Heniford, J.M.Burns: Cirrhosis is not a contraindication to a Laparoscopic Surgery: Surgical Endoscopy (SAGES) 2005
9. Petrisor Banu, Vlad D, Florian Popa, Ion Motofee, Christian Balalau: Cholecystectomy in Cirrhotic Patient -How Safe it is?
Review ROJSP2017,Vol 2(Issue1) E-1-10
10. Jerome M Laurence, Peter D Tran, Arthur Richardson, Henry Pleass, Vincent W T Lam: Laparoscopic or Open Cholecystectomy in Cirrhosis- systematic review of outcomes and meta-analysis of randomized trial HPB 2012 March 14(3) 153-16
11. Rafael S. Pinheiro, Daniel R Wonsberg, Quirino Lai, Wellington Andraus: Laparoscopy Cholecystectomy and Cirrhosis, Patient Selection and technical consideration: Indocyanene
Annals of Laparoscopy and Endoscopy Surgery, Vol 2, no 3, March 2017.
12. Luigi Boni, Giulia David, Alberto Mangano, Gianlorenzo Dionigi: Clinical Application of Indocyanine Green (ICG )enhanced Fluorescence in Laparoscopic Surgery: Surgical Endoscopy 2015
13. Teach, Jean-Jacques MD, Passaux : Laparoscopic Cholecystectomy in Cirrhotic Patients: and Surgical Laparoscopy, Endoscopy, and percutaneous Techniques: Surgical Laparoscopy Journal August 2002, Vol 12, Issue 4, P 227-231
14. Khalid Javid Abid, Sadaf Ishaque: Laparoscopic Cholecystectomy in Cirrhotic Patients PJMHS Vol 10 no 4 October-December 2016.
15. Puggioni, Wong L L: A meta-analysis of Laparoscopic Cholecystectomy in Patients with Cirrhosis: Journal of American College of Surgeons, 2003 Dec 197(6) 921-6
16. K.T. Nguyen: Cirrhosis is not a contradiction to Laparosco[pic Cholecystectomy NCBI 2011
17. Jorge Mancero, A.M. Gonzalez: Laparoscopic Cholecystectomy in Cirrhotic patients World Journal of Surgery, Page 267-270 in 2008.
18. D.Sleeman, Namias N, Levi D: Laparoscopic Cholecystectomy in Cirrhotic Patients Journal of American College of Surgeons 1998 October, 187(4) :400-3
19. Chinnasamy Palanivelu: Laparoscopic Cholecystectomy in Cirrhotic patients: The Role of subtotal cholecystectomy and its variants. Journal of the American College of Surgeons Vol 203, Issue 2, August 2006 Page 145-151
ABSTRACT:
Any gastrointestinal surgery on Cirrhotic Patient is a challenging, quite formidable task for any surgeon especially Cholecystectomy due to increased risk of severe hemorrhage, higher morbidity, and mortality, post-operative infection, longer hospital stay.
After reviewing various journals on Cholecystectomy in cirrhotic patients, the essence of all the articles suggests it is a challenging task to operate on Cirrhotic patients, Laparoscopic Cholecystectomy or Open Cholecystectomy, mainly due to Intraoperative and Postoperative hemorrhage.
According to authors of various articles published recommend Preoperative INR (International Normalised Ratio) and Platelet Count is more important to anticipate bleeding diathesis preoperative and postoperative, shorter convalescence period than Child-Pugh Classification or MELD Score( Model of End-Stage Liver Disease. Child-Pugh Classification or MELD Score is important for Morbidity and Mortality. Cirrhosis, Hepatocellular failure, Portal hypertension enhances the risk of postoperative complications in gastrointestinal surgery especially Biliary surgery. Reviewing relevant articles it seems Laparoscopic Cholecystectomy ( L.C) is a relatively safer procedure than Open Cholecystectomy ( O.C.) especially Child-Pugh Classification A & B. Gall stones are more common in Cirrhotic Patients, three times higher than non -cirrhotic patients. L.C. has a definitive advantage over O.C.'s shorter convalescence period and hospital stay. Acute Cholecystitis is more common in Cirrhotic patients. Emergency operation carries higher mortality, higher morbidity in comparison to elective surgery for Cholelithiasis.
There is no ambiguity, Laparoscopic Cholecystectomy (L.C) is a relatively safer procedure than Open Cholecystectomy (O.C. ). Laparoscopic Cholecystectomy is a better option due to the magnification of intraabdominal organs, target tissues and applying newer devices like Ultrasonic Shears, the use of Harmonics Scalpel (H.S.). Fibrin Spray will reduce intraoperative and postoperative bleeding, better hemostasis in cirrhotic patients despite Coagulopathy in cirrhotic patients. It is a fact Laparoscopic Cholecystectomy (L.C) has a higher conversion rate to Open Cholecystectomy(O.C.)
INTRODUCTION
The operation of Cholelithiasis in Cirrhotic patients is a high-risk procedure. In the past surgeons were reluctant to operate on cirrhotic patients due to high morbidity and mortality. Intraoperative and postoperative hemorrhage due to coagulopathy was one of the major factors. In the past some of the anesthetic agents were hepatotoxic.
With the advent of Laparoscope, with Ultrasound Shears i.e. Harmonics Slalpel (H.S.) Laparoscopic Cholecystectomy (L.C.) in cirrhotic patients has become a safer option.
.
Preoperative assessment of coagulopathy i.e INR and Platelet Count is paramount important for the successful and safer outcome of Laparoscopic Cholecystectomy(L.C.). MELD Score { Model of End-Stage of Liver Disease ) and Child-Pugh Classification can predict reasonably morbidity and mortality following Laparoscopic Cholecystectomy (L.C.) in the cirrhotic patient. Most of the published data regarding Laparoscopic Cholecystectomy(L.C.) in cirrhotic patients suggest it is safe and effective than open cholecystectomy (O.C.) in the cirrhotic patient which can cause high morbidity, high intraoperative and postoperative bleeding, wound infection and high mortality. Patient selection is vitally important before L.C.in cirrhotic patients. According to published papers MELD Score below 13, Child-Pugh class C carries high mortality and morbidity in any type of operation for Cholelithiasis.
According to published papers, only symptomatic Gall Bladder disease should undergo an operation.
MATERIALS and METHODS:
Review of literature from the year 2006 to 2017 was carried out at least 35 articles from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), Google Search, PubMed, Cross-references, reading the title articles. I have selected 30 articles which are well documented, authentic with comparable data. After going through the articles I have analyzed the demographics, indications of Laparoscopic Cholecystectomy(L.C), the incidence of perioperative and postoperative complications, duration of hospitalization, morbidity, and mortality in L.C. vs Open Cholecystectomy(O.C) in cirrhotic patients.
Laparoscopic Cholecystectomy (L.C) started in the 1980s. Previously Cholecystectomy in cirrhotic patients deemed risky and fatal. Since the introduction of Laparoscopic procedure, modern instruments and devices for L.C. seem relatively safer than open cholecystectomy (O.C) in cirrhotic patient especially Child-Pugh classification A and B.
The number of patients who had undergone L.C. for cholelithiasis in cirrhotic patients varies from center to center as per publication in surgical endoscopic journals. It ranges from 2005 patients to 21 patients as per published articles. Rafael Pinheiro in 2017 published paper where he and his associates did Laparoscopic Cholecystectomy (L.C) in 2005 patients with cirrhosis over the years. According to SAGES publication113 patients had L.C. who had cirrhosis between 1995-2006. Spiros Delis in June 2009 published data with 220 patients with cirrhosis who had undergone L.C. Masayuki Akita et all performed L.C. in 21 patients with cirrhosis. Abdul Shaikh et all performed L.C. in 250 patients with cirrhosis, published a paper in the year 2009. Some centers did a statistical analysis of L.C. in cirrhotic patients using CHI Square, WILCOXON rank-sum.
There are centers where Harmonics Scalpel (H.S.)was used than the traditional method for L.C. ie clips for cystic duct and artery, diathermy for gall bladder bed dissection. Ayman El Nakeeb et all published paper in the year 2009 where H.S. was used in 60 patients for L.C. in cirrhotic patients. Abid Khalid et all performed 350 laparoscopic cholecystectomies in cirrhotic patients, published the data in the year 2016. Chinasammy et all feel safer L.C. in 265 cirrhotic patients using traditional method i.e. clips and diathermy. Luigi Boni et all in 2015 published an article using Indocyanine Green (ICG ) enhanced Fluorescence in Laparoscopy Cholecystectomy(L.C) in 52 patients with cirrhosis.
Overall data shows the majority of cirrhotic patients with symptomatic gall bladder disease who had undergone Laparoscopic Cholecystectomy (L.C) were Child-Pugh Classification Aand B. Very few with C type who had L.C. showed higher morbidity and mortality.
RESULTS:
Cirrhosis of the Liver is a serious nature of pathological disorder the Laparoscopic Cholecystectomy (L.C) in symptomatic Cholelithiasis is a safer procedure especially Child-Pugh Aand B, provided INR and Platelet count is within the normal range.
Laparoscopic Cholecystectomy (L.C) in cirrhotic patients causes less intraoperative and postoperative bleeding, less morbidity less mortality, less incidence of postoperative infection, reduced period of hospital stay and early feeding in the postoperative period.
According to the published paper, HarmonicsScalpel (H.S) has more advantages than standard use of Clips and Diathermy in L.C.(El Nakeeb et all 2010). Using H.S. causes less intraoperative bleeding, less gall bladder perforation, less incidence of conversion to Open Cholecystectomy (O.C) and reduced postoperative pain. Jorge M Mancero published a paper in the World Journal of Surgery (in 2008) 23 patients had cirrhosis with Child-Pugh A class 76.7%, B class 23.3%, all these patients had Laparoscopic Cholecystectomy (L.C). All of them undergone L.C. 6 of them with class B developed postoperative Ascites none in A-class, no conversion to Open Cholecystectomy (O.C) in either A or B class.
Another study published by Spiros Delis in June 2009, L.C. was performed in 220 patients who had cirrhosis with symptomatic Cholelithiasis between the year 1995-2008, Child-Pugh A and B both classes had symptomatic gall bladder disease, no death was reported. Intraoperative, Postoperative morbidity occurred in 19% of patients mainly bleeding, wound complications and intraabdominal collection.
Intraoperative bleeding in 19 cases(8.6%), O.C. conversion 12 cases out of 220 patients (5.4%), 22 patients needed postoperative blood transfusion F F P (Fresh Frozen Plasma). In essence MELD Score above 13 showed a higher complication rate postoperatively. Child-Pugh class did not predict morbidity or mortality effectively. It seems MELD Score predicts morbidity more accurately than the Child-Pugh classification system.
According to a published paper in 2009 by Spiros Delis surgeons should pay more attention to MELD Square regarding the predictability of intraoperative and postoperative complications, morbidity and mortality than Child-Pugh classification. Meld score recently introduced and used for the following :
1. To predict survival in cirrhotic patients receiving Trans Jugular Intrahepatic portosystemic shunt (TIPS)
2. To determine priority on the waiting list for a liver transplant
3. To predict the postoperative outcome of cirrhotic patients undergoing surgical procedures.
The MELD score was calculated by using the preoperative values of three laboratory tests: INR, Serum Creatinine and Total Bilirubin.
There was no significant result in MELD Score distribution with gender male or female or Liver cirrhosis etiology alcoholic or nonalcoholic. The article published by W.S.Cobb in the year 2005, 50 patients with cirrhosis ( 27 men and 23 women ) undergone L.C. for symptomatic cholelithiasis. 39 patients were Child-Pugh A, 10 patients were B, one patient class C. The rate of wound infection and wound bleeding were markedly low in those patients who undergone L.C. Evaluating 50 patients by WS Cobb et all who had cirrhosis, the average MELD score was 8.9. According to W.S.Cobb publication although he found L.C. technically challenging because of portal hypertension varies and Thrombocytopenia frequently coexists despite the challenges, advancement in Laparoscopic surgery can safely be performed in patients with mild to moderate cirrhosis of Liver (Child-Pugh A and B Classification). With thorough and proper management of coagulopathy low perioperative and postoperative morbidity, rapid convalescence is achievable for the high-risk groups of patients.
Another published data by Quillin RC et all in 2013 L.C. in 94 patients was carried out in cirrhotic patients with symptomatic gall bladder disease. The median Child-Turcotte-Pugh (CTP) score was 6 and the average MELD score was 11. The average length of stay in the hospital was 2.6 +4-3 days. The conversion rate was 11%. The conversion risk factors were: decreased albumin, increased MELD Score and blood loss. Morbidity occurred in 32 patients.
Predictor of morbidity increases in high INR, high CTP score and number of intraoperative RBC transfusion. Mortality occurred in 4 patients (4.2%). Masayuki Akita et all published paper in the year 2017. 21 patients with cirrhosis of Liver with symptomatic gall bladder disease had undergone L.C. and 74 patients had L.C. without cirrhosis. Despite the Child-Pugh Score being higher in cirrhotic patients, the MELD score was similar in the two groups. There was no difference in operative time or amount of blood transfused. Postoperative hospital stay and postoperative morbidity rates were marked by greater in the cirrhotic group. According to the author,s (Masayuki) opinion safety of Laparoscopic Cholecystectomy in cirrhotic patients are proven and confirmed. Due to the pathological process, the gall bladder is usually completely covered in cirrhotic liver, the French Style approach which allows surgeons more easy access to the gall bladder pocket is supposed to be one of the operative options which are a safer and pragmatic option.
Another study published by Chinnasammy Palanivelee et all in 2006, 265 patients with cirrhosis (Child A and B) with symptomatic gall bladder disease had undergone L.C. between the year 1991 and 2005. The mean operative time in the subtotal cholecystectomy group was 72 minutes, in the standard group was 41 minutes, no mortality reported. 15% of patients postoperative deterioration of Liver function occurred worsening Ascites, port site infection, port site bleeding, intraoperative bleeding and increased bile drainage.
According to Chinnasammy, the author L.C. is a safe and effective treatment for calculous cholecystitis in cirrhotic patients. appropriate modification of subtotal cholecystectomy should be practiced, depending on the risk factors present it is advisable to avoid complications.
Data published by Sleeman et all in 1998 in the Journal of the American college of surgeons. 25 patients with L.C. procedures were carried out in cirrhotic patients from May 1992 till July 1996. There was no mortality in their group. All procedures were successfully performed by L.C., mean length of hospital stay was 1.7 days. Morbidity is consistent with wound hematoma, pneumonia and Ascites(32%) of cases postoperatively. According to Sleeman et all L.C. can be safely be performed in cirrhotic patients with all well-compensated Liver function.
DISCUSSION:
Any abdominal surgery in cirrhotic patients is technically difficult, risky undertaking especially Child-Pugh C, MELD Score over 13, high INR, low Platelet count, coagulopathy which is invariable findings in cirrhotic patients. Open cholecystectomy (O.C. ) in cirrhotic patient carry higher morbidity and mortality, higher incidence of post-operative infection, longer hospital stay. Intraoperative bleeding, postoperative bleeding is a major concern. Cholelithiasis in cirrhotic patients occurs more frequently 3 times more than the general population.
A review of 4895 autopsy records in the literature showed gall stones 29.4% of patients with cirrhosis than 12.8% in noncirrhotic patients. The possible cause of high incidence of gall stone in cirrhotic patients due to intravascular hemolysis, with slowing down of gall bladder emptying and mobility. Reviewing various literature 7-20% mortality and 5-25 % morbidity associated with gall bladder removal in cirrhotic patients are noted. Due to high mortality and morbidity surgeons should carefully think and assess the patient's condition before embarking on cholecystectomy. Cholecystectomy in cirrhotic patients considered as formidable operation. Patients with significant coagulopathy and portal hypertension cholecystectomy should be avoided except in a dire emergency.
Several studies show Laparoscopic Cholecystectomy (L.C. ) in a cirrhotic patient can be safely performed. Preoperative management, patient selection is essential. Child-Pugh A & B, compensated Liver function, normal INR, normal Platelet count, MELD Score below 10 is a good predictor of successful operation, less mortality, and less morbidity. With the advent of new technology ultrasound scan (u/scan ) CAT Scan, preoperative endoscopy can assess the state of Liver failure and cirrhosis of Liver, portal hypertension. Laparoscope also magnifies the operative field, anatomy of biliary and structure, gall bladder bed in case of hemorrhage and portal hypertension.
Using harmonics or ultrasound shears helps to reduce intraoperative bleeding. Pneumoperitoneum during laparoscopy reduces the venous pressure less risk of severe bleeding using harmonics scalpel has definite advantages over clips and it should be Bipolar than Monopolar due to local tissue damage, burn to bowel, remote injury. Using laparoscopy any collection of blood can be easily visualized and any arterial bleeding can be controlled. Laparoscopic cholecystectomy should be performed in symptomatic cholelithiasis patients.
In Child-Pugh C class it is riskier to do either L.C. or O.C. The subcostal incision for O.C. has high risk in cirrhotic patients. Possibility of severe hemorrhage wound infection and delayed wound healing .O.C. has a higher risk of bleeding due to coagulopathy, sepsis, increased morbidity and mortality in Child-Pugh class A and B. Reviewing various literature about L.C. in cirrhotic patients. It seems L.C. is effective, low incidence of intraoperative and postoperative complications, less mortality and less morbidity. first and foremost important is patient selection. There are few parameters that are paramount importance to remember INR, Platelet count, Child-pugh classification, MELD Score, state of Liver failure, portal hypertension. Some centers published data in cirrhotic patients who had undergone L.C. mortality was 10%. in Child-Pugh A class, 30% in B, 82% in C class.
Regarding the operative technique in L.C. place of Port insertion is important. It is advisable to avoid unilateral port in cirrhotic patients due to porta-vena cava shunt using harmonics scalpel reduces the chances of bleeding especially severe adhesions around Callot's Triangle, subtotal cholecystectomy or aspiration of the gall bladder is a safer procedure in case of dense adhesions around Callot's Triangle.
Using Fibrin glue or spray reduces the oozing from the gall bladder bed. Besides Fibrin glue and harmonics scalpel there is a wide variety of bleeding control devices are sold in the market i.e, Tissue -Link, Enseal offers reasonable control of bleeding during dissection of structure and detachment of gall bladder from Liver bed. L.C. provides lower morbidity, reduced operative time, earlier feeding postoperative period, less need for blood transfusion, reduced hospital stay in comparison with O.C. In comparison with the noncirrhotic patient has a higher conversion rate, increased operating time, higher bleeding complications and higher overall morbidity compared with the patient without cirrhosis who had undergone Laparoscopic Cholecystectomy(L.C.)
In 2003 Puggioni and Wong conducted a meta-analysis that included studies of cirrhotic patients submitted Puggioni and Wong about Laparoscopic Cholecystectomy(L.C.), six of patients were cirrhotic and six of them were non-cirrhotic. Puggioni and Wong concluded that although L.C. is a safe procedure for cirrhotic patients, they had a higher rate of conversion to O.C. longer surgery time, more severe bleeding and higher morbidity than noncirrhotic patients. The potential complications of L.C. are damage to the umbilical vein. Trocar should be placed to the right or left of the median line under direct vision to avoid complications. Traction of the gall bladder should be exercised with caution as well as dissection of the Liver, where vessels may be relatively large.
Preoperative imaging with CAT Scan or MRI is important to identify abdominal varices on the abdominal wall. Insertion of the first trocar should be infraumbilical . An experienced surgeon and anesthetist are paramount importance for the proper safe management of cirrhotic patients.
The " Hepatic Arterial buffer response" is impaired in cirrhosis of the Liver. The pressure generated by pneumoperitoneum slows down the hepatic flow in the Liver, which can cause further damage to hepatic cells in cirrhotic patients. To minimize Liver damage using the lowest possible intraabdominal pressure(IAP) that provides good visualization. To minimize Liver damage especially longer operative time, a short period of insufflation every 2 to 3 hours it will reduce the adverse effects on hepatic perfusion may be safer and wise pragmatic steps to take. Bleeding complications are a major cause of adverse outcomes after surgery for patients with Liver cirrhosis and Liver damage. Prothrombin is produced only by the parenchymal cells of the Liver. In reality, its half-life is only 2 days it is a good pointer of hepatocellular decompensation. Several studies have shown Prothrobmin time (P.T)and Partial Thromboplastin time to be a more reliable prognostic indicator. Correcting Coagulopathy and Thrombocytopenia preoperatively is vitally important.
Portal hypertension can be a major concern in L.C.Vascular staples (2mm)to control vascular hilum if indicated, it will reduce blood loss, shorter hospital stay, and fewer wound complications. The laparoscopic procedure reduces the exposure of bloodborne pathogens as compared to open technique(O.C. ) Half of the cirrhotic patients may carry Hepatitis B and C. Many of these patients need Liver Transplant in the future. L.C. surgery may benefit in reducing the severity of postoperative adhesion formation in those patients.
The major difficulties surgeons face during L.C. surgery are the following :
1.Adhesion with new blood vessel formation( Neovascularization)
2. Difficult retraction of the Liver.
3.Inadequate exposure of Callot's Triangle
4. Risky gall bladder bed
5.High-risk Hilum.
The experienced surgeons who have performed numerous L.C. in cirrhotic patients have advised the following safety tips :
Due to the umbilical vein, the recanalization umbilical port should be created away from Falciform ligament. The Liver parenchyma is hard and fibrotic difficult to retract. The retractor should be applied to the body of the gall bladder, just above infundibulum to expose the Callot's Triangle. Rotating Trocars positions to the right If Callot's Triangle not exposed properly then the fundus first method should be used. Bipolar electrosurgery is safe, pragmatic, more useful in cirrhotic patients. Bipolar works more efficiently than the Monopolar instrument to coagulate bleeding area in gall bladder bed and hepatic parenchyma. Harmonics Scalpel (H.S.) or advanced Bipolar devices are helpful especially dissecting peritoneal adhesions. Argon Beam coagulation and Thrombin Spray may also be useful for hemostatic dissection. Minimal blunt dissection is recommended Before completing L.C. all necessary ports should be thoroughly checked for bleeding. All the accessory ports should be closed meticulously even small port 5mm or 3mm.
The separation of the gall bladder from the Liver bed may be difficult and the source of massive bleeding when tortuous, dilated vessels occur in the gall bladder bed. In such cases, the posterior wall may be left intact with the Liver and the remnant either by mucosectomy or by electromigration i.e. Laparoscopic subtotal Cholecystectomy (LSC). LSC type I, II, III can be performed assessing the situation. The use of Harmonics Scalpel (H.S.) markedly reduces bleeding complications in L.C.
Indocyanine Green (ICG )enhanced Fluorescence has possible clinical application in L.C. to improve the view and provide detailed anatomical information during surgery especially where anatomy in Callot's Triangle is blurred, ICG will help for safe L.C.
ICG makes blood vessel and bile duct more prominent looking, delineate the cystic duct, CBD, the cystic artery and hepatic artery. ICG should be injected 45 minutes before the L.C. procedure.
Patients with cirrhosis undergoing nonhepatic surgery have reported mortality in the literature that may be as high as 45%. Over the years surgeons were often reluctant to operate on cirrhotic patients due to the possibility of developing acute or chronic Liver failure especially of anesthetic agents used which could be hepatotoxic also of surgical trauma. The use of less hepatotoxic agents has reduced the risk. The usual risk indicators are Child-Pugh class C, presence of portal hypertension, ascites, encephalopathy, infection, anemia, malnutrition, jaundice, hypoalbuminemia, hypoxemia and Prothrombin Time(P.T.) not resolved by VitaminK or Fresh Frozen Plasma (F FP). The mortality rate of Cholecystectomy is related to the severity of underlying Liver Disease.
The gastrointestinal surgery in cirrhotic patients known to be associated with immense technical difficulty and increased morbidity and mortality. Cirrhosis is a major key intraoperative finding that magnifies the surgical difficulties in L.C. Meta-Analysis of six studies comparing L.C. in cirrhotics and non-cirrhotics patients reported higher conversion rate to open procedure(O.C. )7.06% Vs 3.64 P=0.0237, Odds ratio:1.085-3718, longer operative time 98.2 minutes Vs 70 minutes P=0.00467, Confidence interval(CI): 1.085-3718, increased intraoperative bleeding complications 26.4% Vseve 3.1% P=0.001. The blood loss ( 105.6Vs 35.2ml). Increased overall morbidity 20.86% Vs 7.99% P=0.001.
No statistical difference found regarding wound infection incidence and death. The length of hospital stay was 5.4 Vs 3.5 days. More cirrhotic patients went through emergency procedures for acute cholecystitis. The acute Cholecystitis was evident 47% of patients with cirrhosis Vs 14.7% without cirrhosis.
The Emergency Procedures in cirrhotic patients are associated with higher morbidity, longer postoperative hospitalization and sevenfold higher mortality comparison to elective surgery. According to a systematic review published, identified 2005 patients with cirrhosis undergone Laparoscopic Cholecystectomy(n=1756) and Open Cholecystectomy (n==249). General raw data showed that Laparoscopic Cholecystectomy (L.C. ) procedures compared to O.C. was associated with fewer post op[erative complications 17.6x47.7%, the fewer infection rate of 0.8%x2%. The conversion rate of L.C. was 5.8%. The prevalence of Child-Pugh class A, B, C of patients was similar between L.C. and O.C. L.C. group was A 76.6%, B 21.77%, C 1.59%and O.C. group A 67.2%, B 28.73% and C 4.02% respectively.
The most complications of L.C. found in large case series include postoperative worsening of Ascites 10.6%, Intraoperative bleeding 5.2%, Intraoperative collection 3.5%, pulmonary infection 1.75%, blood transfusion 1.1% and minimal incidence of wound infection. The overall conversion for L.C. in cirrhotic patients ranges from 4.75% to 5.8%. The reason for conversion includes difficulty in identifying anatomy, uncontrolled bleeding, massive intracavitary adherence, the need for common bile duct (CBD) exploration and suspected bile duct injury. It seems MELD Score assessment preoperatively is a more rational approach while considering Conversion from L.C. especially when MELD Score is higher than 14. Population base study Chmilac et all analysis of 2857 L.C. to 38.3 O.C. in cirrhotic patients in the U.S.A. showed uncontrolled bleeding may be a major problem during L.C.It may be caused by abdominal varices and coagulopathy secondary to a reduction of clotting factor synthesis and Thrombocytopenia. Therefore Fresh Frozen Plasma (FFP)and Platelets may be given preoperatively as well as activated recombinant factor VII (rFVII a).
Cholecystectomy in cirrhotic patients used to be an intervention operation procedure with major complications some were fatal. Series from 1980 report mortality rate was 25%, morbidity was 35%. Patient with cirrhosis undergoing Cholecystectomy mortality rate has gone down considerably last two decades due to Laparoscopic procedures(L.C.) Laparoscopic Cholecystectomy offers lower mortality, lower morbidity, shorter operative time, earlier feeding resumption, less need for blood transfusion and reduced hospital stay compared with open cholecystectomy.
Better results are achieved by the following :
1. Magnification of the surgical field gives a clear vision to achieve hemostasis.
2.Suffered venous bleeding control with pneumoperitoneum.
3. Use of Harmonics Scalpel (H.S.) and Laparoscopic ultrasound.
A meta-analysis conducted in 2003 showed that L.C. in cirrhotic patients had less blood loss during operation shorter hospital stay compared with open Cholecystectomy (O.C. ). L.C. performed in cirrhotic patients was associated with a high conversion rate, increased operating time. higher bleeding complications and higher overall morbidity compared with the patient without cirrhosis who received Laparoscopic Cholecystectomy (L.C). Irrespective of better results regarding mortality, reported morbidity remains high. Preoperative prediction of expected post-operative morbidity would be of significant value for preoperative decision making.MELD Score has been used not only for portosystemic shunt and transplanted procedures but also for cardiac and general surgical procedures as well, focussing mainly on the ability of MELD Score to predict mortality.
Cirrhotic patients are operated late in course of their gall bladder disease, present late with severe chronic cholecystitis. Therefore the gall bladder tissue is often woody and friable, hence more extensive surgical dissection is one of the primary steps to surgical success in these patients. Perfect hemostasis is time-consuming in the coagulopathy group. Preoperatively when appropriate correction of coagulopathy was attempted with Fresh Frozen Plasma (FFP) and Vitamin K preinduction and platelets were given post induction as needed. Additional types of modalities can be applied including hemostatic agents such as oxidized cellulose (Gelfoam), Surgical, a topical hemostatic agent like FLoseal, application of ultrasound energy via Harmonics Scalpel (H.S.) All these applications in conjunction with mechanical compression from introduced surgical sponges. Surgical sponges are important for safer and successful surgery in these patients. Finally, a tremendous amount of patience is necessary because of conversion (O.C.)unable to control coagulopathy.
Patients with cirrhosis have a higher risk of postoperative complications. There is a greater risk of patients needing a postoperative blood transfusion, suggestive of increased bleeding tendency. Increased risk of bleeding in cirrhotic patients is due to various factors. In addition, portal hypertension generates Thrombocytopenia due to Hypersplenism and stimulates angiogenesis. The neovascularization in the abdominal wall and around the Liver hilum constitutes a major technical challenge when performing Cholecystectomy in cirrhotic patients. In some cases, percutaneous Cholecystectomy has been suggested for cholecystitis in patients with severe portal hypertension or with Liver cirrhosis grade Child-Pugh C class. Gall stone disease in cirrhotic patients three times higher than noncirrhotic patients. In terms of epidemiology, gall stone disease is a leading cause of hospital admission. The incidence of higher in cirrhotic patients due to changes both to the gall bladder and composition to bile. In most cases a patient with cirrhosis develops black pigmented stones due to increased concentration of unconjugated bilirubin, ionized Ca 2+ in the bile causing supersaturation in calcium bilirubin. Increasing Ca 2+ is due to mucin hypersecretion leading to defective acidification of bile and precipitation of Calcium. The disorder of vascular kinetics consists of hypomobility induced by wall edema and hormonal changes in the context of cirrhosis. Relaxing peptides such as VIP, Somatostatin and Glucagon.
Embarking surgery on the cirrhotic patients faced with certain restraint due to their fragile background and risk of decompensation that can be precipitated by surgery. As Cirrhosis of Liver progresses synthetic dysfunction ensues and cirrhosis becomes " Systemic Disease". Cirrhotic patients have a dynamic circulatory syndrome leading to increased cardiac output and decreased peripheral resistance. It is actually the state of heart failure hidden by decreasing afterload which compensates ventricular filling shortfall but it becomes apparent in conditions of physical or pharmacological stress so-called " Cirrhotic Cardiomyopathy".
Regarding the respiratory function, patients with liver cirrhosis have a degree of hypoxemia caused by ascending diaphragm due to increased abdominal pressure in presence of Ascites. The risk of pulmonary atelectasis is correlated with the presence of ascites and hydrothorax. Hepatopulmonary syndrome as severe functional decompensation of the two organs is characterized by the Triad: Liver failure, severe hypoxemia (PaO2 less than 70 mm Hg) and pulmonary shunts opening carry a very high mortality. Hepatorenal syndrome is a severe renal impairment due to an important reduction in rate given by vasoconstrictors which can be triggered by numerous factors including bacterial infection.
In addition coagulation disorder in cirrhosis deficiency in protein synthesis immune dysfunctions and the fact, these deficiencies increase with the progression of cirrhosis. It becomes obvious why practicing surgery in these patients requires a thorough preoperative evaluation and optimization of patients are blood loss, postoperative Liver failure, and sepsis that may cause a high rate of mortality and morbidity.
Laparoscopic Cholecystectomy (L.C.) has become Gold Standard in the treatment of benign disease of the gall bladder and expanded its indication inpatient with Liver cirrhosis, the major benefit is less traumatic and has lower mortality and morbidity associated with. The main reason the Laparoscopy Cholecystectomy (L.C.) does not require a large opening of the peritoneum and there is less risk of Ascitic fluid leak and sepsis.
CONCLUSION:
Incidence of Cholelithiasis( Gall Stone) three times higher in the cirrhotic patient than noncirrhotic patients. Cholecystectomy in the cirrhotic patients is a challenging formidable task for surgeons. Laparoscopic Cholecystectomy(L.C.) can be performed safely in selected patients with cirrhosis of Liver Child-Pugh class A and B who have symptoms of Cholelithiasis with acceptable morbidity.
The advantage of L.C. in comparison with Open Cholecystectomy (O.C. ) shorter operative time, reduced hospital stay.
Preoperative MELD Score, INR, Platelet Count predict reasonably intraoperative and postoperative complications, morbidity and mortality than the Child-Pugh classification system.
Patients with cirrhosis and cholelithiasis Laparoscopic Cholecystectomy (L.C.) should be performed. Patient with significant Portal Hypertension and severe Coagulopathy L.C. or O.C. should be Avoided, should be managed Conservatively also in Child-Pugh class C except for emergency situation. The patient should be assessed carefully before surgery. In Child-Pugh class, C in an emergency situation as acute Cholecystitis Percutaneous drainage of gall bladder would be a safer option. Any major procedure of whether O.C.or L.C. carries high mortality and morbidity.
L.C. also Protects surgeons and theatre staff exposure to viral infection Hepatitis B and C which is the major cause of Cirrhosis of Liver in patients. The surgeon with vast experience L.C. is a safer procedure in cirrhotic patient especially Child-Pugh class A and B. Laparoscopic Cholecystectomy (L.C.) should be the mainstay of operative procedure in a cirrhotic patient. The operative risk whether intraoperative and postoperative in cirrhotic patients depends on the degree of Preexistent Hepatic Dysfunction, nature of the procedure and Comorbid Conditions.
KEYWORDS:
Cirrhosis-Cholelithiasis-Laparoscopic Cholecystectomy-MELD Score-Child-Pugh classification-Morbidity-Mortality.
ACKNOWLEDGMENTS:
I am indebted to Professor R.K.Mishra and his team at World Laparoscopic Hospital, Delhi India for their guidance and advice regarding compiling this Review Article.
REFERENCES:
1. E. Cucinotta, S.Lazzara, G.Melita: Laparoscopic Cholecystectomy in Cirrhotic Patients, surgical endoscopy and other interventions. Surgical Endoscopy, December 2003( SAGES)
2. J.SCHIFF, M. Mishra, G.Rendon: Laparoscopic Cholecystectomy in Cirrhotic Patients: Surgical Endoscopy 2005 Sept19(9): 278-81 (SAGES)
3. A.M.Lacey, C.Balaguer, E.Andrade, J.C.Garcia-Valdecasas: Laparoscopic Cholecystectomy in Cirrhotic Patients: Surawis:
surgical Endoscopy (SAGES) 1995
4. C.N.Yeh, M.F.Chen, Y.Y.Jan: Laparoscopic Cholecystectomy in 226 Cirrhotic Patients: Surgical Endoscopy (SAGES)2002
5. Spiros Delis, Andreas Bakoyianis, Juan Madariaga, John Bramis: Laparoscopic Cholecystectomy in Cirrhotic Patients-The value of MELD Score and Child-Pugh classification in predicting outcome: Surgical Endoscopy( SAGES) 2010
6. Ayman El Nakeeb, Waleed Askar, Ramadan El lithy, Mohamed Farid: Clipless Laparoscopic Cholecystectomy using Harmonics Scalpel Vs Conventional Method in cirrhotic patients: J.Gastrointestinal Surgery 2010 Feb 14(2): 323-8
7. Hiroshi Saeki, Daisuke Korenaga, Hirohiko Yamaga, Kyotaro Mawatari: A comparison of Open and Laparoscopic cholecystectomy for patients with cirrhosis: Surgery Today, May 1997, Vol 27, Issue 5, PP 411-413
8. W.S.Cobb, B.T. Heniford, J.M.Burns: Cirrhosis is not a contraindication to a Laparoscopic Surgery: Surgical Endoscopy (SAGES) 2005
9. Petrisor Banu, Vlad D, Florian Popa, Ion Motofee, Christian Balalau: Cholecystectomy in Cirrhotic Patient -How Safe it is?
Review ROJSP2017,Vol 2(Issue1) E-1-10
10. Jerome M Laurence, Peter D Tran, Arthur Richardson, Henry Pleass, Vincent W T Lam: Laparoscopic or Open Cholecystectomy in Cirrhosis- systematic review of outcomes and meta-analysis of randomized trial HPB 2012 March 14(3) 153-16
11. Rafael S. Pinheiro, Daniel R Wonsberg, Quirino Lai, Wellington Andraus: Laparoscopy Cholecystectomy and Cirrhosis, Patient Selection and technical consideration: Indocyanene
Annals of Laparoscopy and Endoscopy Surgery, Vol 2, no 3, March 2017.
12. Luigi Boni, Giulia David, Alberto Mangano, Gianlorenzo Dionigi: Clinical Application of Indocyanine Green (ICG )enhanced Fluorescence in Laparoscopic Surgery: Surgical Endoscopy 2015
13. Teach, Jean-Jacques MD, Passaux : Laparoscopic Cholecystectomy in Cirrhotic Patients: and Surgical Laparoscopy, Endoscopy, and percutaneous Techniques: Surgical Laparoscopy Journal August 2002, Vol 12, Issue 4, P 227-231
14. Khalid Javid Abid, Sadaf Ishaque: Laparoscopic Cholecystectomy in Cirrhotic Patients PJMHS Vol 10 no 4 October-December 2016.
15. Puggioni, Wong L L: A meta-analysis of Laparoscopic Cholecystectomy in Patients with Cirrhosis: Journal of American College of Surgeons, 2003 Dec 197(6) 921-6
16. K.T. Nguyen: Cirrhosis is not a contradiction to Laparosco[pic Cholecystectomy NCBI 2011
17. Jorge Mancero, A.M. Gonzalez: Laparoscopic Cholecystectomy in Cirrhotic patients World Journal of Surgery, Page 267-270 in 2008.
18. D.Sleeman, Namias N, Levi D: Laparoscopic Cholecystectomy in Cirrhotic Patients Journal of American College of Surgeons 1998 October, 187(4) :400-3
19. Chinnasamy Palanivelu: Laparoscopic Cholecystectomy in Cirrhotic patients: The Role of subtotal cholecystectomy and its variants. Journal of the American College of Surgeons Vol 203, Issue 2, August 2006 Page 145-151