A Review of Laparoscopic Vesico-Vaginal Fistula Repair
REVIEW ARTICLE
MINIMAL ACCESS, OPTIMAL DRYNESS: A review of laparoscopic repair of vesicovaginal fistula.
Click here to download complete articleMichael S Archibong1*, Oluwole E Ayegbusi1
1Department of Obstetrics and Gynaecology, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Osun state, South west, Nigeria.
ABSTRACT
Background: Vesicovaginal fistula (VVF) is an embarrassing condition to women . Various routes of surgical intervention exists with regards to the management of VVF. Laparoscopic repair has been shown to be safe and effective.
Objective: To review the success rate of laparoscopic repair of VVF and to highlight the benefits/advantages of the laparoscopic approach.
Methods: Using various databases, previous studies of patients who underwent laparoscopic VVF repair between 2008 and 2018 were reviewed. Outcome measures from these studies were success rate, mean blood loss, mean operating time, length of hospital stay, major intraoperative complications and conversion to open surgery.
Results: 14 retrospective studies (full-text articles) were retrieved and reviewed. 269 patients had laparoscopic repair. The pooled success rate was 96.7 %. Mean Blood loss ranged from 30-400mls, length of hospital stay ranged from 1.1 to 7.8 days while the mean operating time ranged from 54 to 229 minutes. There was only one major intraoperative complication. Only 4 patients had to be converted to open surgery.
Conclusion: Laparoscopic repair of VVF has a high success rate and is a safe, patient-friendly and cost-effective route for surgical management of VVF.
Keywords: Vesicovaginal fistula, laparoscopic route, abdominal repair.
How to cite: Archibong M.S, Ayegbusi O.E. MINIMAL ACCESS, OPTIMAL DRYNESS: A review of laparoscopic repair of vesicovaginal fistula. World J Lap Surg 2019
Corresponding author: Michael S Archibong. Senior Registrar, Department of Obstetrics and Gynaecology, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Southwest Nigeria. Phone: +2348063553021, Email: beracah4@yahoo.com
Introduction
Vesicovaginal fistula (VVF) is an abnormal communication between the epithelium of the bladder and that of the vagina which leads to continuous/total involuntary leakage of urine. It is a condition that not only affects the health of the woman but also imposes a great deal of social embarrassment and psychological trauma on the patient. It is considered as one of the most dehumanizing conditions that affect and reduces the quality of life of women 1
The etiology of VVF is largely influenced by socioeconomic development /standard of health care delivery system. In underdeveloped/developing countries, Prolonged labor accounts for over 90% of VVF; however, in developed countries, it is usually from iatrogenic causes particularly from hysterectomies for benign gynecological conditions, radiation therapy, and advanced reproductive tract malignancies2.
It has been estimated that there are about 3 million women with unrepaired fistula globally, with about 150,000 new cases every year 3. Ever since the first successful VVF repair pioneered by James Marion Sim, various methods and techniques have subsequently been discovered and employed to surgically treat VVF. With respect to the route of repair, there is no consensus regarding the best route, as this is influenced by a variety of factors like the site, size, etiology, surgeons choice and level of expertise/competence 4.
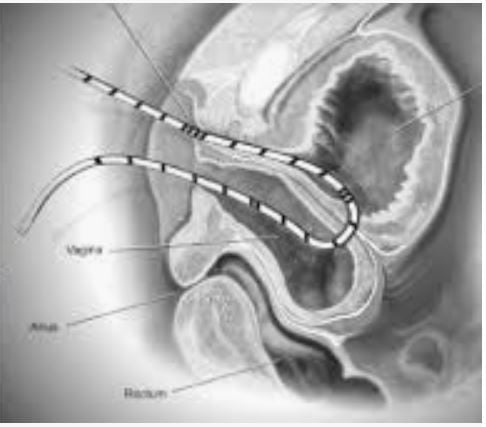
VVF can be repaired by two routes: vaginal and abdominal. The abdominal route repair has been performed predominantly by open surgery (laparotomy) and has been found to be associated with more morbidities; these morbidities can be minimized/ avoided via minimal access surgery5.
Minimal access surgery has reformed the field of gynaecology; becoming established in everyday practice and is gradually becoming the norm and gold standard in gynecological practice and in diagnosis and treatment of various gynecological conditions including repair of VVF. Laparoscopic repair of VVF has been conducted with remarkable success6.
The purpose of this article is to review the success rates of the laparoscopic repair of VVF and also highlight some of the benefits/advantages of the laparoscopic repair.
MATERIALS AND METHODS
Search strategy: Relevant studies /publications were searched for using Pubmed, Google scholar, Cochrane library, ScienceDirect, Embase, Medline. The databases were searched using the relevant medical subject headings(MeSH) terms. Search words included: vesicovaginal fistula, laparoscopic repair, abdominal route. No restriction was placed on the language of publication.
Study selection: Studies selected were original research articles published in the last 10 years with more than 7 patients. Studies greater than 10 years from the date of publication and/or studies with less than 8 patients were excluded.
Data extraction: The data assessed from the studies included: success rate, mean blood loss, mean operating time, length of hospital stay, major intraoperative complications and conversion to open surgery.
RESULTS:
Within the limits of literature search, 14 full-text articles met the aforementioned criteria. All articles were retrospective, there were no prospective studies or randomized controlled trials. From this review, a total of 269 patients underwent laparoscopic repair of VVF. 231 (85.9%) cases were primary repairs while 38(14.1%) cases had previous failed repairs. Nine out of the fourteen series reviewed reported a success rate of 100%, the other series reported success rates of 98, 95.5, 91.6, 87.5 and 86% respectively. Laparoscopic repair failed in only 9 out of the 269 patients (2 out of these 9 patients were those with previously failed repair). The pooled/overall success rate was 96.7%., while the success rates for those undergoing primary and previously failed repair were 96.9% and 94.7% respectively. Mean Blood loss ranged from 30-400mls, length of hospital stay ranged from 1.1 to 7.8 days while the mean operating time ranged from 54 to 229 minutes. There was only one major intraoperative complication (bleeding), giving a complication rate of 0.37%. 265 (98.5%) cases were completed laparoscopically; only 4 patients had to be converted to open surgery due to severe adhesions, the overall/ pooled conversion rate was 1.5%. ( Table 1).
Discussion
The first laparoscopic VVF repair was reported by Nezhat et al in 199416. Like any advancement in medical practice, it was initially greeted with a lot of skepticism and criticism. However, over the years this approach has come to be embraced and has gained more acceptance among fistula repair surgeons because of the available evidence which has proved it to be very effective. Meta-analysis and comparative studies have found the success rates between laparoscopic and open laparotomy to be comparable with a statistically significant shorter hospital stay and reduced blood loss 6,12,20.
Previously it was thought that the laparoscopic route may be associated with a lot of conversions to open surgery, this review has disproved that, as only 4 out of 256 repairs were converted to open surgery. Interestingly, conversions were not due to a complication of laparoscopy per se but rather from dense intra-abdominal adhesions/fibrosis (due to previous surgeries) which in itself is a relative contraindication to laparoscopy.
It was also thought that laparoscopic repair may not be suitable for patients with previously failed repair, however, this review has revealed that the success rate for primary repair and those with previously failed repairs are comparable. With a complication rate of less than 1% from this review, credence has been lent to the safety of the laparoscopic approach to VVF repair. The safety and minimal blood loss in laparoscopic repair may be attributed to the enhanced /magnified vision during surgery which affords the surgeon the benefit of dissecting tissues with a high degree of precision and accuracy without iatrogenic injury to adjacent structures. The pneumoperitoneum also functions as a hemostatic tamponade to help minimize blood loss.
The quick recovery period, reduced hospital stay and better cosmesis associated with laparoscopic repair have shown that this approach confers on the patient some cost-benefit or cost-utility.
Laparoscopic repair of VVF is a highly technical and advanced laparoscopic procedure which involves a lot of intracorporeal suturing and knot tying, this underscores the need for proper training and skill acquisition in order to attain expertise and competence before it should be embarked upon. However, the advent of barbed sutures which eliminates the need for knot tying can enhance surgical efficiency and significantly shorten the operating time 21.
Conclusion
The laparoscopic approach to the surgical management of VVF is effective, safe and associated with minimal complications.
Fistula repair surgeons (particularly) in developing countries should acquire the necessary skills and acquaint themselves with this route of repair in other for patients to benefit from the advantages which this approach confers.
Studies done so far on the laparoscopic repair of VVF have been retrospective studies. There is a need for prospective and randomized controlled trials to further substantiate and strengthen the already existing body of evidence.
Acknowledgment
The author wishes to acknowledge the entire training staff of world laparoscopy Hospital, Gurgaon India, led by Prof R.K Mishra and Dr. Chowhan.
REFERENCES
1. Ijaiya MA, Rahman AG, Aboyeji AP, Olatinwo AW, Esuga SA, Ogah OK, et al. Vesicovaginal fistula: a review of the nigerian experience. West Afr J Med. 2010; 29(5):293-298.
2. Moselle LT, Kohi TW, Mvungi A, Evjen-Olsen B, Moland KM. Waiting for attention and care birthing accounts of women in rural Tanzania who developed obstetric fistula as an outcome of labor. BMC Pregnancy Childbirth. 2011;11:75.
3. Adegoke AI. Prevalence of anemia in obstetric fistula patients in Abakaliki. Int J Res Med Sci 2018;6:2611-4.
4. Abdel-Karim AM, Mahfouz W. Laparoscopic VVF Repair: Current Trends. Current Women’s Health Reviews, 2013, 9,:93-98
5. Nwogu-Ikojo E, Chigbu C, Iloabachie G. Bladder-only Repair Of Vesicovaginal Fistula: Twelve Years Experience In South-eastern Nigeria. Webmed Cen Obstet Gynecol. 2010; 1(10): 1-4.
6. Bodner-Adler B, Hanzal E, Pablik E, Koelbl H, Bodner K. Management of vesicovaginal fistulas (VVFs) in women following benign gynecologic surgery: A systematic review and meta-analysis. PLoS ONE 2017; 12(2): e0171554.
7. Utrera NM, Foneron A, Castillo OA. Laparoscopic vesicovaginal fistula repair. Arch Esp Urol. 2012 ;65(10):887-90.
8. Abdel-Karim AM, Mousa A, Hasouna M, Elsalmy S Laparoscopic transperitoneal extravesical repair of vesicovaginal fistula. Int Urogynecol J, 2011;22:693–697
9. Miklos JR, Moore RD. Laparoscopic extravesical vesicovaginal fistula repair: our technique and 15-years experience. Int Urogynecol J, 2015. 26:441–446
10. Sharma S, Rizvi SJ, Bethur SS, Bansal J, Qadri S, Modi P. Laparoscopic repair of urogenital fistulae: A single centre experience. J Min Access Surg 2014;10:180-4.
11. Shuah SJ. Laparoscopic transabdominal transvesical vesicovaginal fistula repair. J Endourol. 2009 ; 23(7):1135-7.
12. Transperitoneal laparoscopic repair of vesicovaginal fistula for patients with supratrigonal fistula: comparison with open transperitoneal technique. Int Urogynecol J, 2016 ;27(9):1415-22
13. Chu Lei, Wang Jian-Jun, Xiao-Wen Tong, Bo-Zhen Fan, Yi Guo, Huai-Fang Li Laparoscopic repair of iatrogenic vesicovaginal and rectovaginal fistula. Int J Clin Exp Med
2015;8(2):2364-2370
14. Abreu AD, Tanaka M. Laparoscopic Management of Iatrogenic Lesions. J Endourol. 2008;22(6):1279-83
15. Javali TD, Katti A, Nagaraj HK. A . A simplified laparoscopic approach to repair of vesicovaginal fistula: the MS Ramaiah technique. Urology, 2015;85(3):544-6
16. Mallikarjuna C, Maryak P, Reddy S. The AINU Technique for LaparoscopicVesico-Vaginal Fistula Repair: A Preliminary Report Urol Int 2015;95:357–360
17. Rizvi SJ, Gupta R, Patel S, Trivedi A, Trivedi P, Modi P. Modified laparoscopic abdominal vesico-vaginal fistula repair-"Mini-O'Connor" vesicostomy. J Laparoendosc Adv Surg Tech A. 2010; 20(1): 13-15.
18. Zhang Q, Ye Z, Liu F, Qi X, Shao C, He Xet al. Laparoscopic transabdominal transvesical repair of supratrigonal vesicovaginal fistula. Int Urogynecol J. 2013; 24: 337-342
19. González L, Rodríguez R, , Javier A. . Laparoscopic Transperitoneal Vesicovaginal Fistula Repair. Journal of Gynecologic Surgery. 2017; 33(5):1-5
20. Ghosh B, Wats V, Pal DK. Comparative analysis of outcome between laparoscopic versus open surgical repair for vesicovaginal fistula. Obstet Gynecol Sci 2016;59(6):525-529
21 Shah HN, Nayyar R, Rajamahanty S, Hemal AK Prospective evaluation of unidirectional barbed suture for various indications in surgeon-controlled robotic reconstructive urologic surgery: Wake Forest University experience. Int Urol Nephrol,2012; 44(3):775–785. How to cite: Archibong M.S, Ayegbusi O.E. MINIMAL ACCESS, OPTIMAL DRYNESS: A review of the success of laparoscopic repair of vesicovaginal fistula. World J Lap Surg 2019
Corresponding author:
Michael S Archibong. Senior Registrar, Department of Obstetrics and Gynaecology, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, South West Nigeria. Phone: +2348063553021, Email: beracah4@yahoo.com
Click here to download complete article