Comparison of Learning Curve of Intra corporeal suturing between Robotic Assisted Laparoscopic Surgery and Conventional Laparoscopic Surgery
Comparison of Learning Curve of Intra corporeal suturing between Robotic Assisted Laparoscopic Surgery ( RALS) & Conventional Laparoscopic Surgery (CLS) by Minimal Access Surgery(MAS) Beginners
Dr. A.H.M Azharul Islam
Student – Master in Minimal Access Surgery
Reg. Roll no : M.MAS /001/2011D
Department of Minimal Access Surgery
The Global Open (TGO) University, India
Research Station:
Institute of Minimal Access Surgery
World Laparoscopy Hospital
Gurgaon, NCR, Delhi, India
Declaration of the Resreach work
This primary data base dissertation / research work is submitted as partial fulfilment of the requirements of the degree of Master in Minimal Access Surgery final examination of The Global Open (TGO) University. This Research work was done during Ist May ,2012 to 31st March ,2013 in Institute of Minimal Access Surgery , World Laparoscopy Hospital , Gurgaon, India
No portion of the work referred to in the dissertation has been submitted in support of an application for another degree or qualification of this or any other Institution of learning.
Dr. A.H.M Azharul Islam
M.MAS / 001 / 2011D
Forwarding Letter
Certified that Dr. A.H.M Azharul Islam , M.MAS / 001 / 2011D , carried out this research work titled Comparison of Learning Curve of Intra corporeal suturing between Robotic Assisted Laparoscopic Surgery ( RALS) & Conventional Laparoscopic Surgery (CLS) by Minimal Access Surgery(MAS) Beginners and prepared this dissertation under my direct supervision. I have found the work and the dissertation satisfactory for partial fulfilment of the requirements of the degree of Master in Minimal Access Surgery final examination of The Global Open ( TGO) University , India.
Prof. Dr. R.K Mishra
Professor and Head ,
Department of Minimal Access Surgery
The Global Open (TGO) University , India
Director , World Laparoscopy Hospital , Gurgaon
ACKNOWLEDGEMENT
It is a great pleasure to express my deepest gratitude and indebtedness to my teacher and guide, Prof .Dr. R.K Mishara, MS , MRCS , MMAS , PhD Professor & Head , Department of Minimal Access Surgery, The Global Open (TGO) University , India & Director , World Laparoscopy Hospital , Gurgaon , India for her sincere help, constant supervision and guidance to make this dissertation complete, in the midst of his heavy and busy work schedule.
My great respect and gratitude to Dr. Chowhan, MS, Senior Consultant , World Laparoscopy Hospital , Gurgaon , India for his valuable suggestions and advise during this study. I also thank Dr. Shakil Hossan Rony to help to analyze data and composition of the work.
.
I want to thank all my colleagues and also administrative staff especially Mr. Ranjan, Mr. Motin , all library & Laboratory staff of the institute, for helping me in all possible ways.
Finally, I shall ever remain indebted to all those trainee doctors whose participation made this work find its way.
Dr. A.H.M Azharul Islam
M.MAS / 001 /2011D
Abbreviation
MAS – Minimal Access Surgery
RALS – Robotic Assisted Laparoscopic Surgery
RAL - Robotic Assisted Laparoscopy
CLS- Conventional Laparoscopic Surgery
CL - Conventional Laparoscopy
Abstract
Background :
Robotic assisted laparoscopy (RAL) is used in a wide range of operative interventions, but the advantage of this technique over conventional laparoscopy (CL) remains unclear. Studies comparing RAL and CL are scarce. The present study was performed to test the hypothesis that maiden users master surgical tasks quicker with the robot-assisted laparoscopy technique than with the conventional laparoscopy technique.
Methods:
30 subjects, with little or no prior laparoscopic surgical experience, performed three different surgical tasks in a standardized experimental setting, repeated four times with each of the RAL and CL techniques. Speed and accuracy were measured. A cross-over technique was used to eliminate gender bias and the experience gained by carrying out the first part of the study.
Results:
The task "tie a knot" was performed faster with the RAL technique than with CL. Furthermore, shorter operating times were observed when changing from CL to RAL. There were no time differences for the tasks of grabbing the needle and continuous suturing between the two operating techniques. Gender did not influence the results.
Conclusion:
The more advanced task of tying a knot was performed faster using the RAL technique than with CL. Simpler surgical interventions were performed equally fast with either technique. Technical skills acquired during the use of CL were transferred to the RAL technique. The lack of tactile feedback in RAL seemed to matter. There were no differences between males and female.
Conventional laparoscopic surgery (CL) may offer great advantages to patients but can be demanding for the surgeon because of several technical drawbacks. These limitations include 2-dimensional vision with less than optimal perception of depth, disturbance of the eye-hand-target axis, the fulcrum effect, rigid instruments with limited degrees of freedom and limited tactile feedback. These factors might attribute to the relatively long training period required before reaching a professional level[1,2].
The da Vinci® surgical system from Intuitive Surgical® has been available since 1998 and is still the only robotic surgical system available on the market approved for performing surgical interventions in humans. Several advantages with robotic assisted laparoscopy (RAL) over CL have been identified: 3-dimensional visualization of the operative field with depth perception, additional degrees of freedom and downscaling of instrument movements, restoration of the eye-hand-target axis and enhanced stability, elimination of the fulcrum effect and improved ergonomics for the surgeon.
One stated consequence of these features is that endoscopic surgical skills are more easily mastered and the learning curve is shortened [2-4]. Some authors have succeeded in performing RAL for cases they never tried with CL, possibly indicating that RAL is considered easier [5].
A definition of the learning curve can be the amount of practice, in terms of time or number of repetitions, needed to reach a certain level of proficiency for completing a specific task. Parameters used when analysing learning curves are time to complete the task, the number of errors made and actions required. Learning curves in daily practice are often defined by operating time, blood loss; morbidity and length of hospital stay [3].
There is only very scant literature on the comparison of learning curves for RAL and CL [3,6]. It is also a challenge to interpret the results of earlier studies, one reason being the different levels of previous experience among the participants. However, to know more about the learning curve in minimally invasive surgery and preferably, as a consequence, to be able to shorten the time needed for operative training before reaching a consistent level, is desirable. We therefore decided to test our hypothesis that surgically maiden subjects perform surgical tasks faster with the robot-assisted laparoscopy technique than with the conventional laparoscopy technique
Literature Review:
Suturing is one of the main tasks in advanced laparoscopic surgery, but limited degrees of freedom, 2D vision, fulcrum and pivoting effect make it difficult to perform. Robotic systems provide corresponding solutions as three-dimensional (3D) view, intuitive motion and additional degrees of freedom. This review evaluates these benefits for their impact on suturing in experimental and clinical studies. The Medline database was searched for "robot*, telemanipulator* and laparoscopy*". A total of 1150 references were found and further limited to "suturing" for experimental evaluation, finding 89 references. All references were considered for information on robotic suturing in advanced laparoscopy. Further references were obtained through cross-referencing the bibliography cited in each work. In experimental studies current robotic systems have proven their superior suturing capabilities compared to conventional laparoscopic techniques, mainly attributed to 3D visualization and full seven degrees of freedom. In clinical studies these benefits have not yet been sufficiently reproduced. Robotic systems have to prove the benefits shown in experimental studies for suturing tasks in clinical applications. Robotic devices shorten the learning curve of laparoscopic procedures. Further clinical trials focusing on anastomosis time are needed to assess this question.
"Our findings show that, over a relatively short time, even inexperienced surgeons can perform RALS with efficiency and results comparable to open surgery," said Hiep Nguyen, MD, FAAP, Director of Robotic Surgery and Research, Children's Hospital Boston. "RALS is allowing us to perform suturing more quickly and safely, and we hope that ultimately this will allow for patients to recover faster and with reduced pain."
Place of study- World Laparoscopy Hospital , Gurgaon, India
Duration of study- Ist May ,2012 to 31st March ,2013
Research Question /hypothesis- An experimental study of 30 subjects to compare the learning curve of Intra corporeal suturing by robotic assisted laparoscopic surgery (RALS) & Conventional Laparoscopic surgery(CLS).
Study population-
30 Subjects (Surgeons) with little or no Laparoscopic exposure. From a cohort of approximately 200 Surgeons at World Laparoscopic Hospital, Gurgaon, India, volunteers were invited to participate in this project and from these, 30 subjects (20 men and 10 women), were randomly selected)
a) Inclusion criteria - Minimally exposed in minimal access technique. Age- 30-45 years
b) Exclusion criteria-
It is an experimental study of 30 subjects
Material Used:
30 subjects with performed three different surgical tasks in a standardized experimental setting, repeated four times with each of the RAL and CL techniques. Speed and accuracy were measured. A cross-over technique was used to eliminate gender bias and the experience gained by carrying out the first part of the study. SPSS is used to comparing the data of different subject’s skill.
The workstation was prepared in a standardized way and the participants were allowed to familiarize themselves with the instruments for two minutes before starting the trial. The thread was 20 cm long for both suturing and tying a knot. Each of the 30 students carried out three tasks, grab the needle in a correct way, place three continuous sutures over a rift in the Skin Pad (tissue) and tie a surgical knot. These tasks were done four times with each of RAL and CL. The subjects were divided according to gender and half the males and half the females began with RAL and CL, respectively.
Each subject's results from the RAL and the CL, respectively, were recorded and mean values were calculated for the groups: RAL Green, CL Green, RAL Red and CL Red.
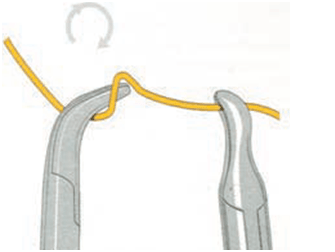
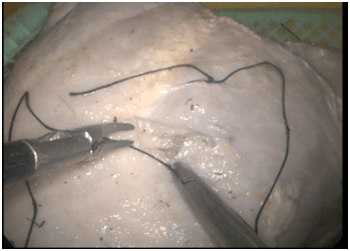
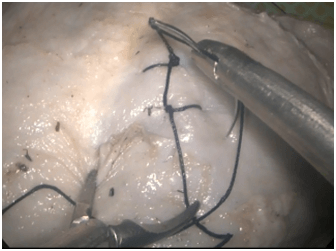
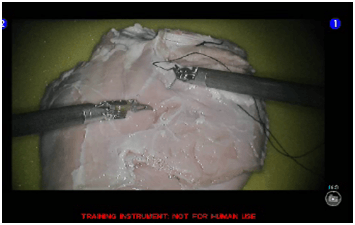
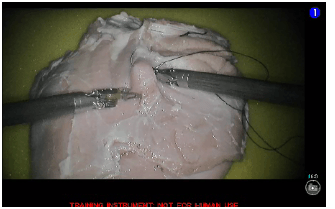
Fig: 1.1 : (Ideal way of doing Intra corporeal surgical knotting).
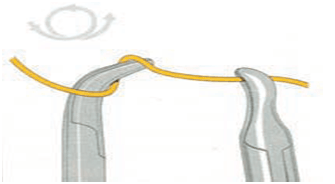
Fig: 1.2 : (Ideal way of doing Intra corporeal surgical knotting).
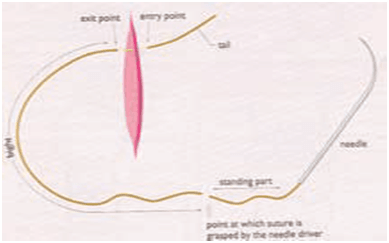
Fig: 1.3 : (Ideal way of doing Intra corporeal surgical knotting).
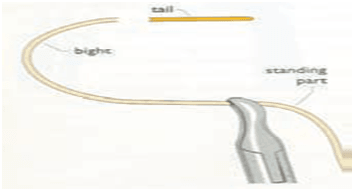
Fig: 1.4 : (Ideal way of doing Intra corporeal surgical knotting)
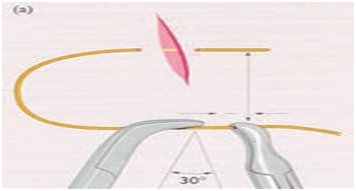
Fig: 1.5 : (Ideal way of doing Intra corporeal surgical knotting)
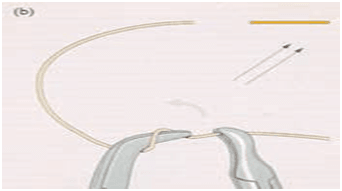
Fig: 1.6 : (Ideal way of doing Intra corporeal surgical knotting)
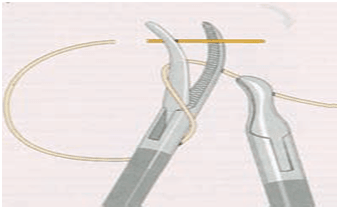
Fig: 1.7 : (Ideal way of doing Intra corporeal surgical knotting)
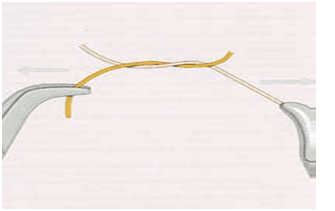
Fig: 1.8 : (Ideal way of doing Intra corporeal surgical knotting)
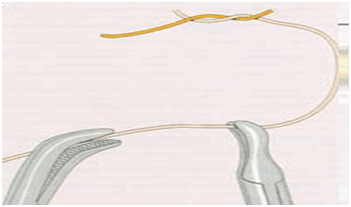
Fig: 1.9 : (Ideal way of doing Intra corporeal surgical knotting )
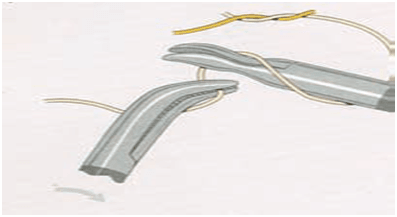
Fig: 1.10 : (Ideal way of doing Intra corporeal surgical knotting)
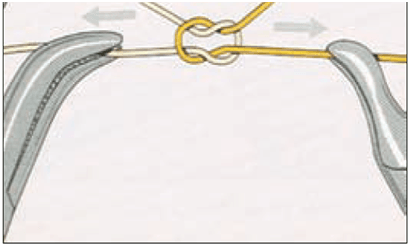
Fig: 1.11: (Ideal way of doing Intra corporeal surgical knotting )
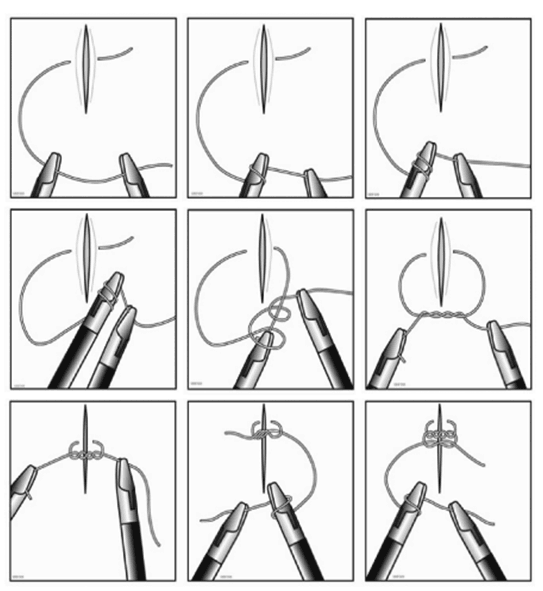
Fig : 1.12 : (Summary- Ideal way of doing Intra corporeal surgical knotting )

Time in sec of each group of participants
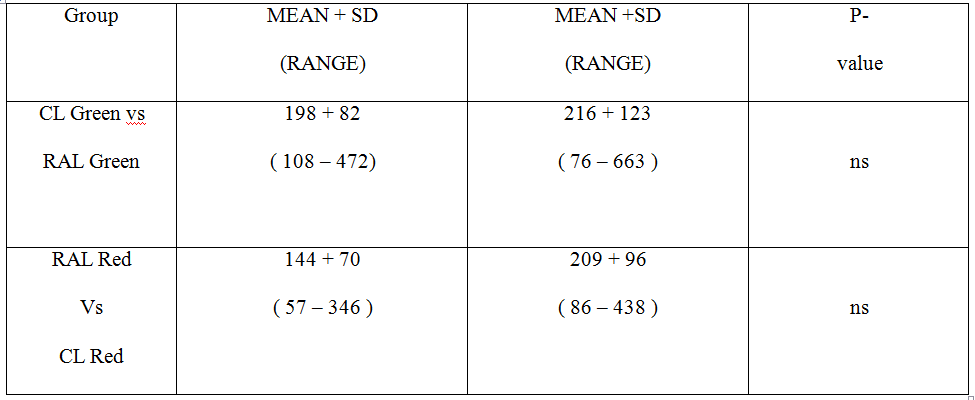
Time in sec of each group of participants
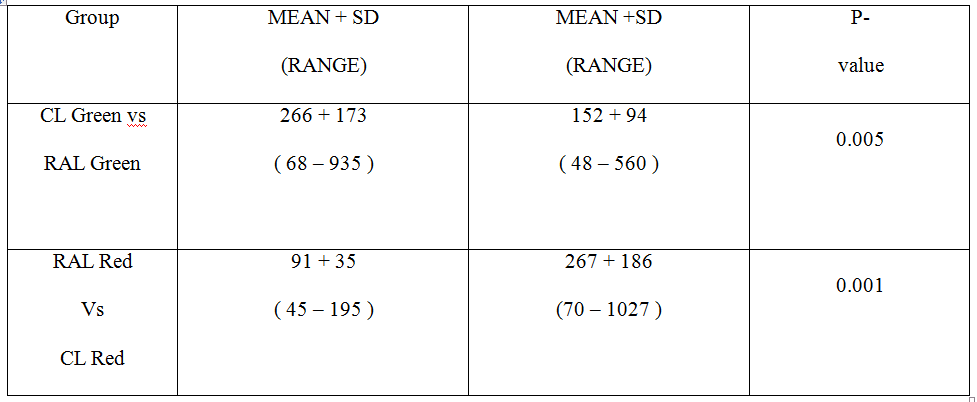
Time in sec of each group of participants
Discussion:
References :
1. Subramonian K, Desylva S, Bishai P, et al: Acquiring surgical skills: a comparative study of open versus laparoscopic surgery. Eur J Urol 2004, 45:346-351.
2. Heemskerk J, van Gemert WG, de Vries J, Greve JW, Bouvy ND: Learning curves of Robot-assisted Laparoscopic Surgery Compared With Conventional Laparoscopic Surgery: An Experimental Study Evaluating Skill Acquisition of Robot-assisted Laparoscopic Tasks Compared With Conventional Laparoscopic Tasks in Inexperienced Users. Surg Laparosc Endosc Percutan Tech 2007, 17:171-174.
3. Olthof E, Nio D, Bemelman WA: The learning curve of robot-assisted laparoscopic surgery. Medical robotics Vienna: I-Tech Education and PublishingBozovic V 2008, 1-8.
4. Meehan JJ, Meehan TD, Sandler A: Robotic fundoplication in children: resident teaching and a single institutional review of our first 50 patients. J Pediatr Surg 2007, 42:2022-2025.
5. Meehan JJ, Sandler A: Pediatric robotic surgery: A single-institutional review of the first 100 consecutive cases. Surg Endosc 2008, 22:177-182.
6. Yohannes P, Rotariu P, Pinto P: Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 2002, 60:39-45.
7. Blavier A, Gaudissart Q, Cadière GB, Nyssen AS: Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 2007, 194:115-121.
8. Heemskerk J, van Gemert WG, Greve JW, Bouvy ND: Robot-assisted Versus Conventional Laparoscopic Nissen Fundoplication: A Comparative Retrospective Study on Costs and Time Consumption. Surg Laparosc Endosc Percutan Tech 2007, 17:1-4.
9. Anderberg M, Clementson Kockum C, Arnbjörnsson E: Robotic fundoplication in children. Pediatr Surg Int 2007, 23:123-127.
10. Narazaki K, Oleynikov D, Stergiou N, et al: Robotic surgery training and performance. Identifying objective variables for quantifying the extent of proficiency. Surg Endosc 2006, 20:96-103.
11. Hernandez JD, Bann SD, Munz Y, et al: Qualitative and quantitative analysis of the learning curve of a simulated task on the da Vinci system. Surg Endosc 2004, 18:372-378.
12. Ro CY, Toumpoulis IK, Ashton RC, et al: A novel drill set for the enhancement and assessment of robotic surgical performance. Stud Health Technol Inform 2005, 111:418-421.
13. Stefanidis D, et al: Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 2009, 24(2):377-82.
14. Byrn JC, Schluender S, Divino CM, et al: Three dimensional imaging improves surgical performance for both novice and experienced operators using the Da Vinci Robot system. Am J Surg 2007, 193:519-522.
15. Reznick , Richard , Regehr , Glenn , et al: Testing Technical Skills Via an Innovative “Bench Station” Examination. The American Journal of Surgery 1997, 173(3):226-230.
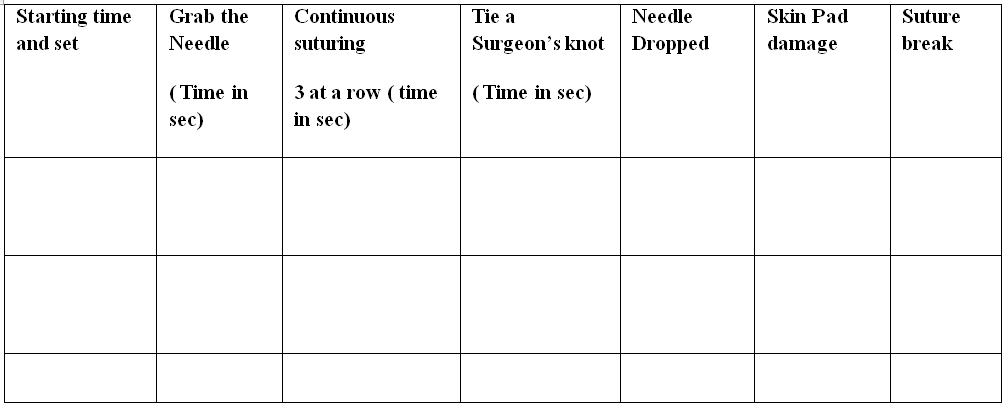
Appendices : Appendix I
Data Collection Sheet
Place of Study : World Laparoscopy Hospital,Gurgaon
Date :
Name of the Participant : …………………………………………………………………….
Gender: Age:
Experiences in MAS :
Task performed group : RAL …………………….. / CL …………………..
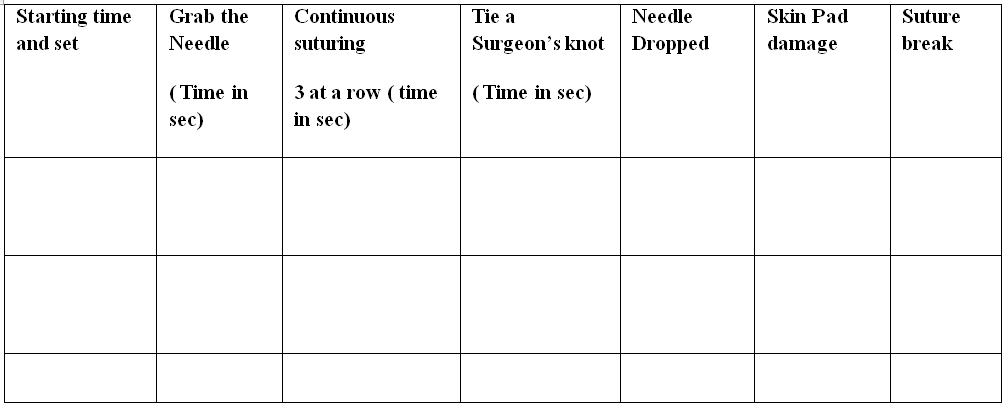
Signature of the Researcher Signature of the supervisor
Appendices : Appendix II
Informed Written Concept
I undersigned Trainee doctor at World Laparoscopy Hospital , Gurgaon , India ,has come to Know that Dr. A.H.M Azharul Islam M.MAS/ 001/2011D, The Global Open (TGO) University performing an experimental (practical based) research on learning curve of intra corporeal suturing between RALS & CLS by MAS beginners . He has explained all the reason & value behind this study. He also assures me that I have every right to withdraw myself from the study at any point of time. His act in this study is only an investigator.
I gladly agree to participate in the study.
Signature and Full name of the participant
Dr. A.H.M Azharul Islam
Student – Master in Minimal Access Surgery
Reg. Roll no : M.MAS /001/2011D
Department of Minimal Access Surgery
The Global Open (TGO) University, India
Research Station:
Institute of Minimal Access Surgery
World Laparoscopy Hospital
Gurgaon, NCR, Delhi, India
Declaration of the Resreach work
This primary data base dissertation / research work is submitted as partial fulfilment of the requirements of the degree of Master in Minimal Access Surgery final examination of The Global Open (TGO) University. This Research work was done during Ist May ,2012 to 31st March ,2013 in Institute of Minimal Access Surgery , World Laparoscopy Hospital , Gurgaon, India
No portion of the work referred to in the dissertation has been submitted in support of an application for another degree or qualification of this or any other Institution of learning.
Dr. A.H.M Azharul Islam
M.MAS / 001 / 2011D
Forwarding Letter
Certified that Dr. A.H.M Azharul Islam , M.MAS / 001 / 2011D , carried out this research work titled Comparison of Learning Curve of Intra corporeal suturing between Robotic Assisted Laparoscopic Surgery ( RALS) & Conventional Laparoscopic Surgery (CLS) by Minimal Access Surgery(MAS) Beginners and prepared this dissertation under my direct supervision. I have found the work and the dissertation satisfactory for partial fulfilment of the requirements of the degree of Master in Minimal Access Surgery final examination of The Global Open ( TGO) University , India.
Prof. Dr. R.K Mishra
Professor and Head ,
Department of Minimal Access Surgery
The Global Open (TGO) University , India
Director , World Laparoscopy Hospital , Gurgaon
ACKNOWLEDGEMENT
It is a great pleasure to express my deepest gratitude and indebtedness to my teacher and guide, Prof .Dr. R.K Mishara, MS , MRCS , MMAS , PhD Professor & Head , Department of Minimal Access Surgery, The Global Open (TGO) University , India & Director , World Laparoscopy Hospital , Gurgaon , India for her sincere help, constant supervision and guidance to make this dissertation complete, in the midst of his heavy and busy work schedule.
My great respect and gratitude to Dr. Chowhan, MS, Senior Consultant , World Laparoscopy Hospital , Gurgaon , India for his valuable suggestions and advise during this study. I also thank Dr. Shakil Hossan Rony to help to analyze data and composition of the work.
.
I want to thank all my colleagues and also administrative staff especially Mr. Ranjan, Mr. Motin , all library & Laboratory staff of the institute, for helping me in all possible ways.
Finally, I shall ever remain indebted to all those trainee doctors whose participation made this work find its way.
Dr. A.H.M Azharul Islam
M.MAS / 001 /2011D
Abbreviation
MAS – Minimal Access Surgery
RALS – Robotic Assisted Laparoscopic Surgery
RAL - Robotic Assisted Laparoscopy
CLS- Conventional Laparoscopic Surgery
CL - Conventional Laparoscopy
Abstract
Background :
Robotic assisted laparoscopy (RAL) is used in a wide range of operative interventions, but the advantage of this technique over conventional laparoscopy (CL) remains unclear. Studies comparing RAL and CL are scarce. The present study was performed to test the hypothesis that maiden users master surgical tasks quicker with the robot-assisted laparoscopy technique than with the conventional laparoscopy technique.
Methods:
30 subjects, with little or no prior laparoscopic surgical experience, performed three different surgical tasks in a standardized experimental setting, repeated four times with each of the RAL and CL techniques. Speed and accuracy were measured. A cross-over technique was used to eliminate gender bias and the experience gained by carrying out the first part of the study.
Results:
The task "tie a knot" was performed faster with the RAL technique than with CL. Furthermore, shorter operating times were observed when changing from CL to RAL. There were no time differences for the tasks of grabbing the needle and continuous suturing between the two operating techniques. Gender did not influence the results.
Conclusion:
The more advanced task of tying a knot was performed faster using the RAL technique than with CL. Simpler surgical interventions were performed equally fast with either technique. Technical skills acquired during the use of CL were transferred to the RAL technique. The lack of tactile feedback in RAL seemed to matter. There were no differences between males and female.
Conventional laparoscopic surgery (CL) may offer great advantages to patients but can be demanding for the surgeon because of several technical drawbacks. These limitations include 2-dimensional vision with less than optimal perception of depth, disturbance of the eye-hand-target axis, the fulcrum effect, rigid instruments with limited degrees of freedom and limited tactile feedback. These factors might attribute to the relatively long training period required before reaching a professional level[1,2].
The da Vinci® surgical system from Intuitive Surgical® has been available since 1998 and is still the only robotic surgical system available on the market approved for performing surgical interventions in humans. Several advantages with robotic assisted laparoscopy (RAL) over CL have been identified: 3-dimensional visualization of the operative field with depth perception, additional degrees of freedom and downscaling of instrument movements, restoration of the eye-hand-target axis and enhanced stability, elimination of the fulcrum effect and improved ergonomics for the surgeon.
One stated consequence of these features is that endoscopic surgical skills are more easily mastered and the learning curve is shortened [2-4]. Some authors have succeeded in performing RAL for cases they never tried with CL, possibly indicating that RAL is considered easier [5].
A definition of the learning curve can be the amount of practice, in terms of time or number of repetitions, needed to reach a certain level of proficiency for completing a specific task. Parameters used when analysing learning curves are time to complete the task, the number of errors made and actions required. Learning curves in daily practice are often defined by operating time, blood loss; morbidity and length of hospital stay [3].
There is only very scant literature on the comparison of learning curves for RAL and CL [3,6]. It is also a challenge to interpret the results of earlier studies, one reason being the different levels of previous experience among the participants. However, to know more about the learning curve in minimally invasive surgery and preferably, as a consequence, to be able to shorten the time needed for operative training before reaching a consistent level, is desirable. We therefore decided to test our hypothesis that surgically maiden subjects perform surgical tasks faster with the robot-assisted laparoscopy technique than with the conventional laparoscopy technique
Literature Review:
Suturing is one of the main tasks in advanced laparoscopic surgery, but limited degrees of freedom, 2D vision, fulcrum and pivoting effect make it difficult to perform. Robotic systems provide corresponding solutions as three-dimensional (3D) view, intuitive motion and additional degrees of freedom. This review evaluates these benefits for their impact on suturing in experimental and clinical studies. The Medline database was searched for "robot*, telemanipulator* and laparoscopy*". A total of 1150 references were found and further limited to "suturing" for experimental evaluation, finding 89 references. All references were considered for information on robotic suturing in advanced laparoscopy. Further references were obtained through cross-referencing the bibliography cited in each work. In experimental studies current robotic systems have proven their superior suturing capabilities compared to conventional laparoscopic techniques, mainly attributed to 3D visualization and full seven degrees of freedom. In clinical studies these benefits have not yet been sufficiently reproduced. Robotic systems have to prove the benefits shown in experimental studies for suturing tasks in clinical applications. Robotic devices shorten the learning curve of laparoscopic procedures. Further clinical trials focusing on anastomosis time are needed to assess this question.
"Our findings show that, over a relatively short time, even inexperienced surgeons can perform RALS with efficiency and results comparable to open surgery," said Hiep Nguyen, MD, FAAP, Director of Robotic Surgery and Research, Children's Hospital Boston. "RALS is allowing us to perform suturing more quickly and safely, and we hope that ultimately this will allow for patients to recover faster and with reduced pain."
Aim & Objectives:
- Aim :The aim of this study is to compare the different stages of suturing technique performing in Robotic assisted laparoscopic surgery and conventional laparoscopic surgery.
- Specific Objectives:
- Grab the needle – Time in seconds
- Continuous suturing ( 3 stiches )- Time in second
- Tie a knot ( square knot) – Time in second
- Dropped needle ? – Number of time / set
- Damage of the skin pad ( tissue)? – Yes / No
- Tearing of the thread – Number of time /set
Materials and methods :
Study Design- Prospective study.Place of study- World Laparoscopy Hospital , Gurgaon, India
Duration of study- Ist May ,2012 to 31st March ,2013
Research Question /hypothesis- An experimental study of 30 subjects to compare the learning curve of Intra corporeal suturing by robotic assisted laparoscopic surgery (RALS) & Conventional Laparoscopic surgery(CLS).
Study population-
30 Subjects (Surgeons) with little or no Laparoscopic exposure. From a cohort of approximately 200 Surgeons at World Laparoscopic Hospital, Gurgaon, India, volunteers were invited to participate in this project and from these, 30 subjects (20 men and 10 women), were randomly selected)
a) Inclusion criteria - Minimally exposed in minimal access technique. Age- 30-45 years
b) Exclusion criteria-
- Experts Surgeon
- Maiden Surgeon
- Age more than 45 years or less than 30 years
- Surgeon having Co morbidity
It is an experimental study of 30 subjects
Material Used:
- Da Vinci Surgical system of World Laparoscopy hospital
- A robotic needle holder and a grasper
- A laparoscopic needle holder and a grasper
- Laparoscopic optics
- Skin pad ( tissue)
- Suture material ( 3/0 Silk)
30 subjects with performed three different surgical tasks in a standardized experimental setting, repeated four times with each of the RAL and CL techniques. Speed and accuracy were measured. A cross-over technique was used to eliminate gender bias and the experience gained by carrying out the first part of the study. SPSS is used to comparing the data of different subject’s skill.
The workstation was prepared in a standardized way and the participants were allowed to familiarize themselves with the instruments for two minutes before starting the trial. The thread was 20 cm long for both suturing and tying a knot. Each of the 30 students carried out three tasks, grab the needle in a correct way, place three continuous sutures over a rift in the Skin Pad (tissue) and tie a surgical knot. These tasks were done four times with each of RAL and CL. The subjects were divided according to gender and half the males and half the females began with RAL and CL, respectively.
Each subject's results from the RAL and the CL, respectively, were recorded and mean values were calculated for the groups: RAL Green, CL Green, RAL Red and CL Red.
Results:
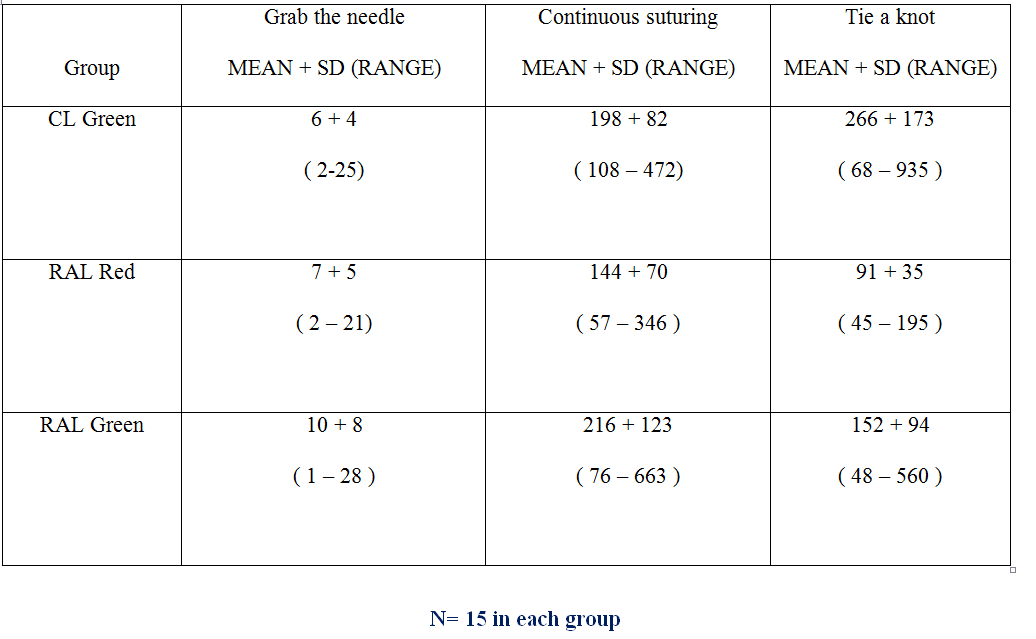
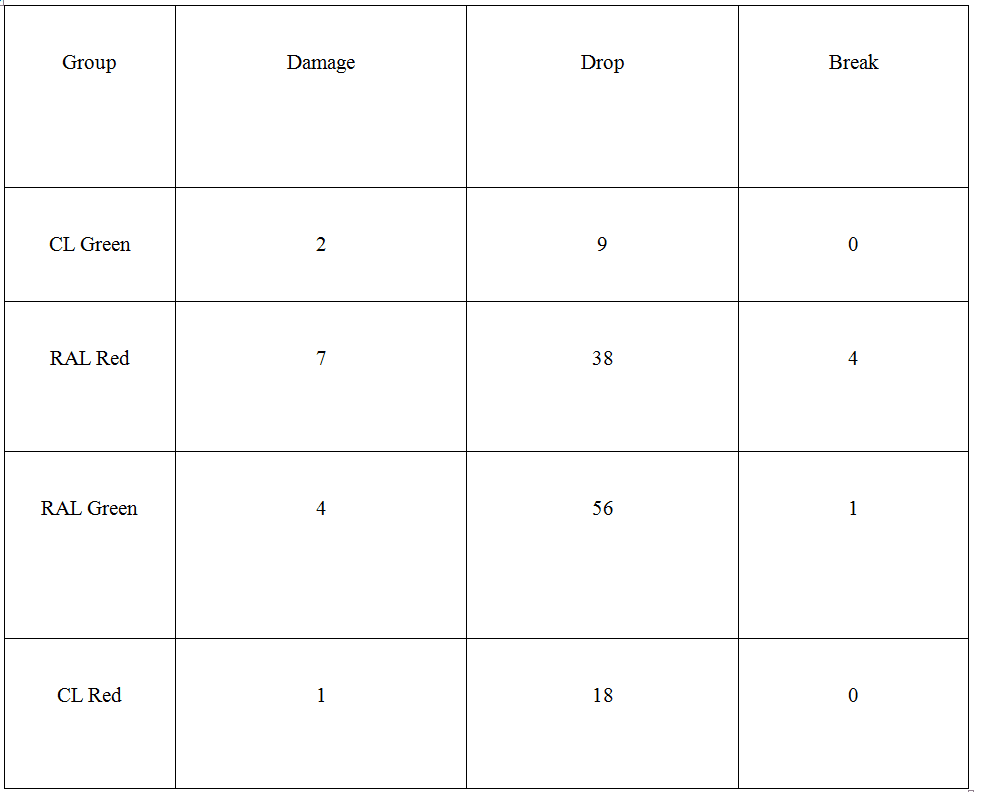
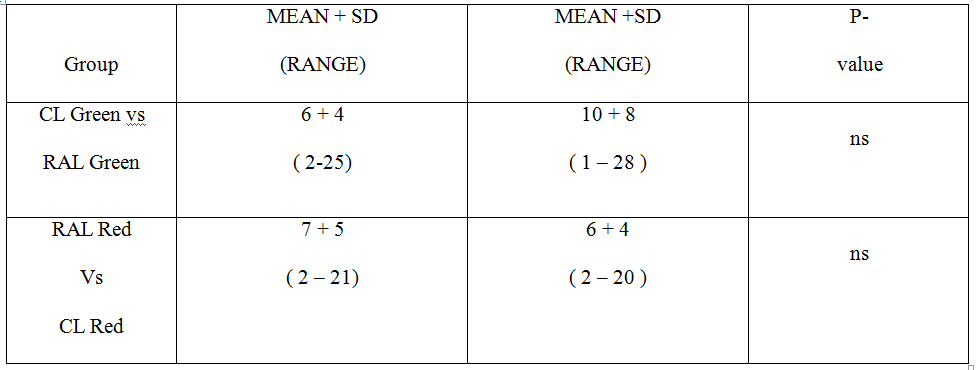
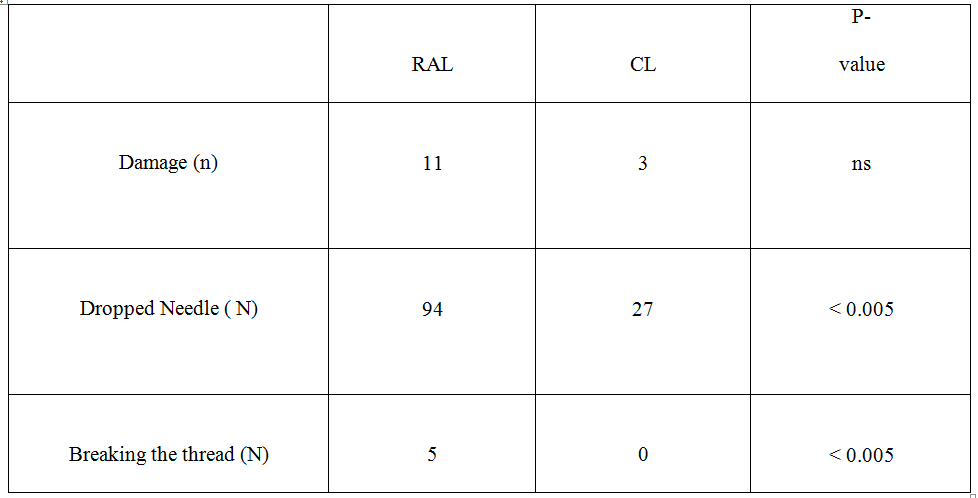
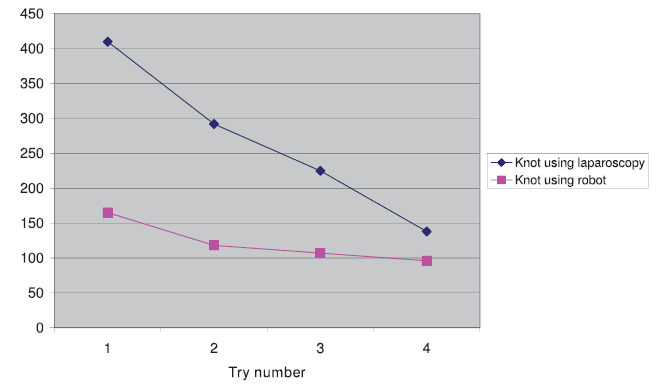
The values are summarized in Tables 1 and 2. "Grabbing the needle" and "suturing continuously" were carried out at equal speeds with RAL and CL. The transfer effect was seen when performing the continuous suturing for RAL but not for CL (Tables 3, 4). The same transfer effect was seen for RAL in tying a knot but not for CL. The task of tying a knot was performed faster with RAL than with CL regardless of whether RAL was performed first or second. A difference was observed in tying the knot when changing to the other operating technique, regardless of which technique the subjects started with. The difference favoured RAL and was negative for CL (Table 5). Dropping the needle happened more often during the RAL part of the study and tearing the thread only occurred with the RAL technique. Damage to the Skin Pad (tissue) was equally common though more in RAL(Table 6). There are learning curves seen for tying a knot (Figure 4) and continuous suturing (Figure 5) for both RAL and CL when comparing trials 1 and 4. There was no difference between the male and female subjects' performances regarding any of the three tasks or the three quality indicators included in the study.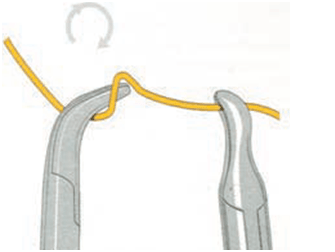
Fig: 1.1 : (Ideal way of doing Intra corporeal surgical knotting).
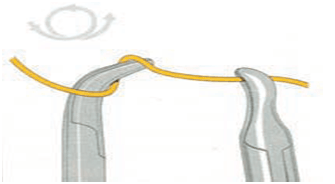
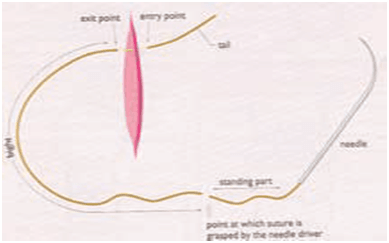
Fig: 1.3 : (Ideal way of doing Intra corporeal surgical knotting).
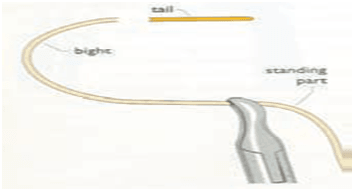
Fig: 1.4 : (Ideal way of doing Intra corporeal surgical knotting)
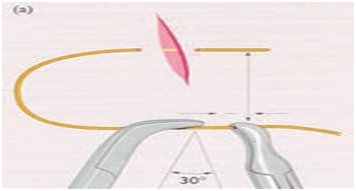
Fig: 1.5 : (Ideal way of doing Intra corporeal surgical knotting)
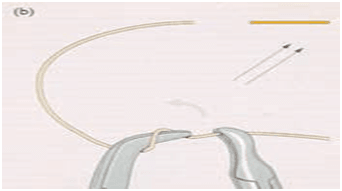
Fig: 1.6 : (Ideal way of doing Intra corporeal surgical knotting)
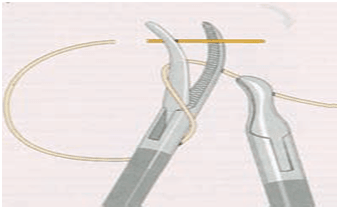
Fig: 1.7 : (Ideal way of doing Intra corporeal surgical knotting)
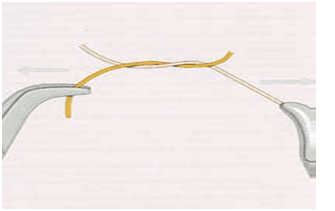
Fig: 1.8 : (Ideal way of doing Intra corporeal surgical knotting)
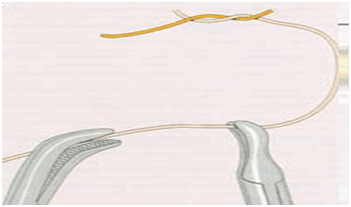
Fig: 1.9 : (Ideal way of doing Intra corporeal surgical knotting )
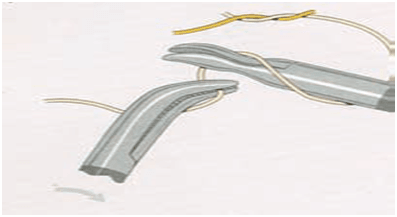
Fig: 1.10 : (Ideal way of doing Intra corporeal surgical knotting)
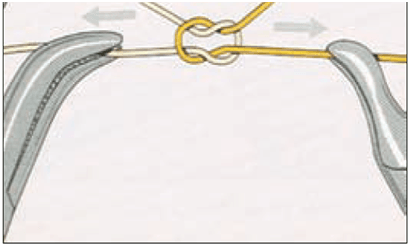
Fig: 1.11: (Ideal way of doing Intra corporeal surgical knotting )
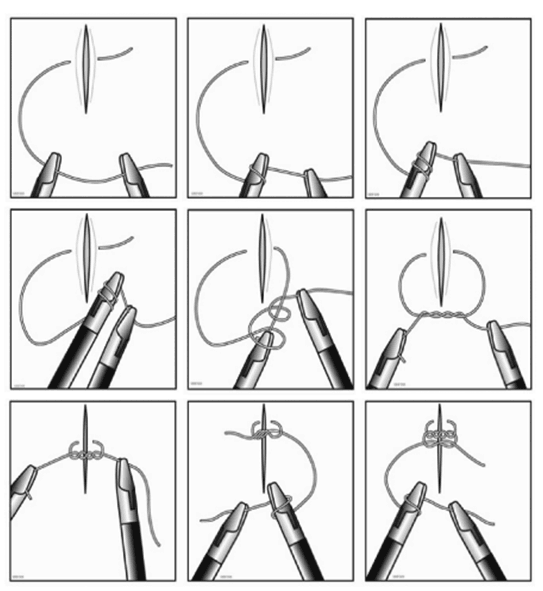
Fig : 1.12 : (Summary- Ideal way of doing Intra corporeal surgical knotting )
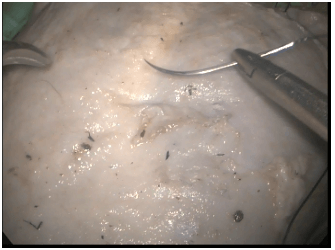
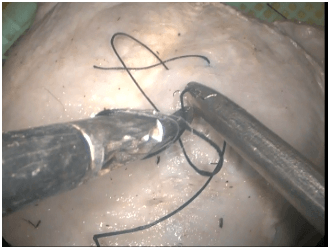
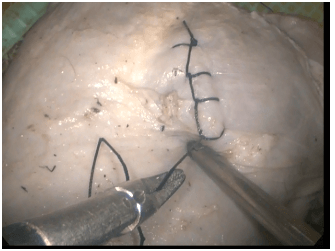
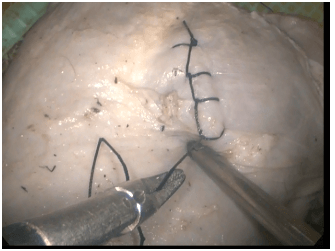
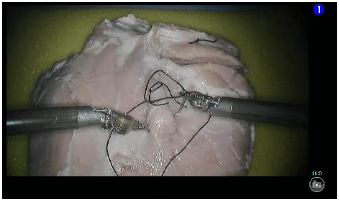
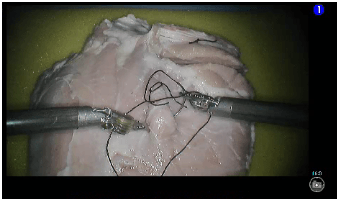
CL intracorporeal suturing & knotting by the participants :
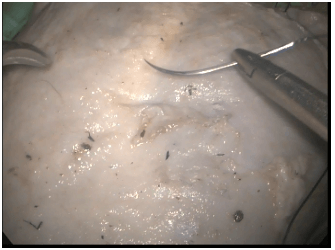
Fig: 2.1 :
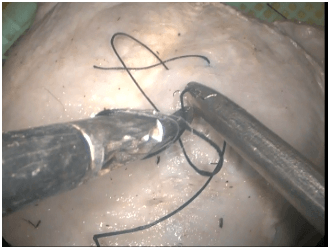
Fig: 2.2 :
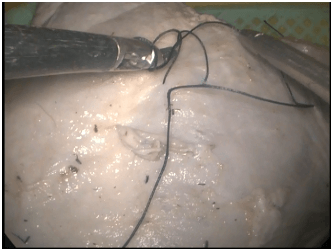
Fig: 2.3 :
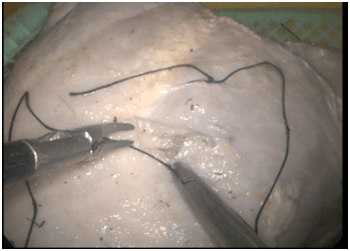
Fig: 2.4 :

Fig: 2.5 :
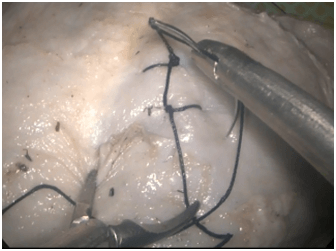
Fig: 2.6 :
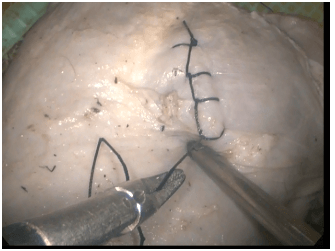
Fig: 2.7 :
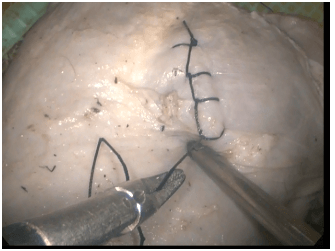
Fig: 2.8 :
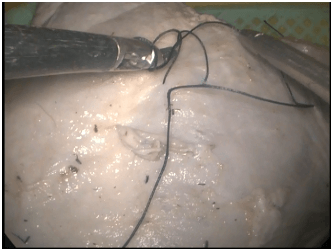
RAL intracorporeal suturing & knotting by the Participants :
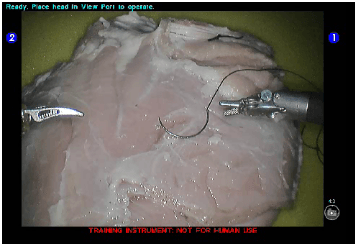
Fig: 3.1
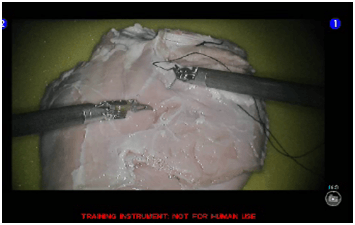
Fig: 3.2 :
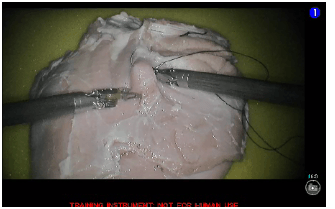
Fig: 3.3 :
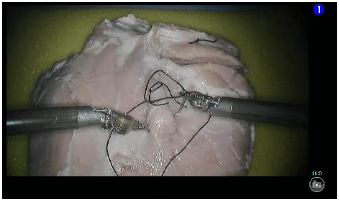
Fig: 3.4:
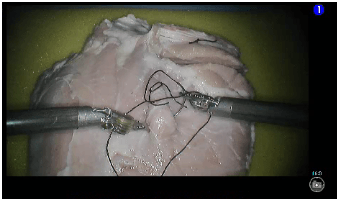
Fig: 3.5 :
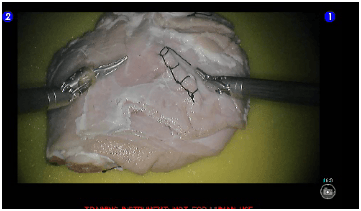
Fig: 3.6 :
Table 1 : Time in sec for each group of participants
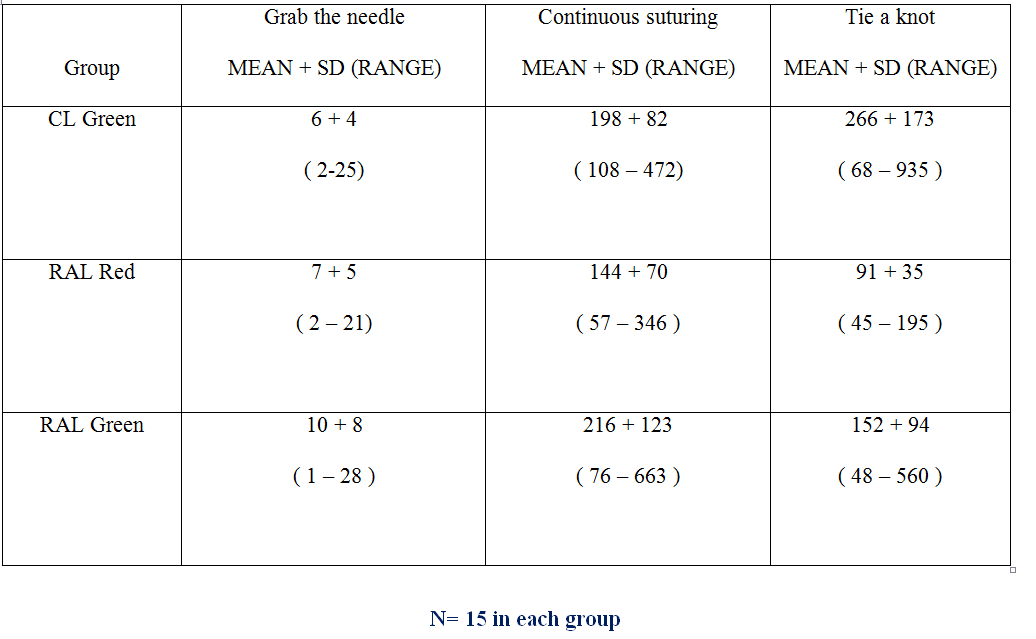
Table 2 : Qualitative parameters for each group of participants
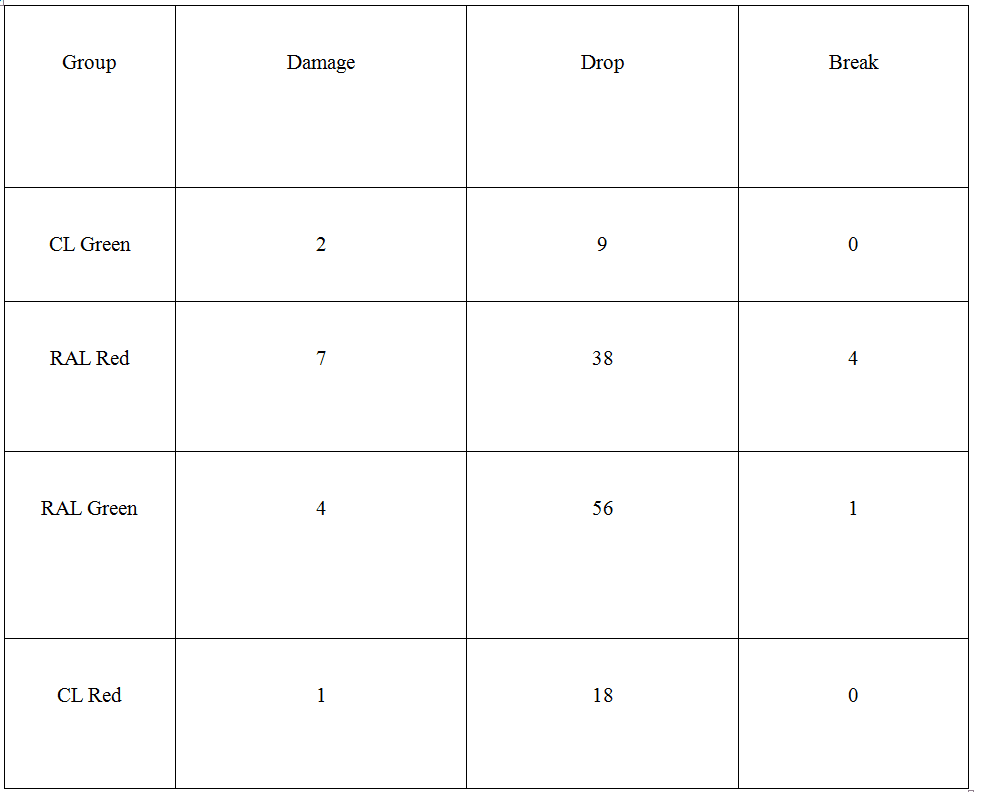
Number of times damage the tissue pad , dropping the needle or breaking the thread
Table 3 : Grabbing the needle
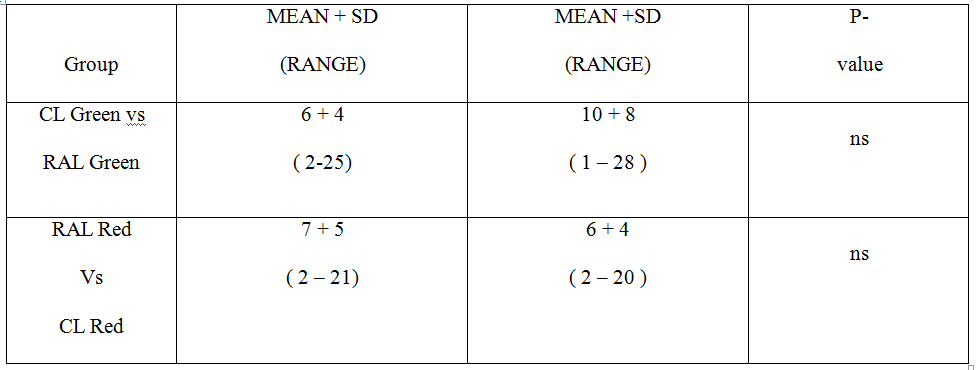
Time in sec of each group of participants
Table 4 : Continuous suturing
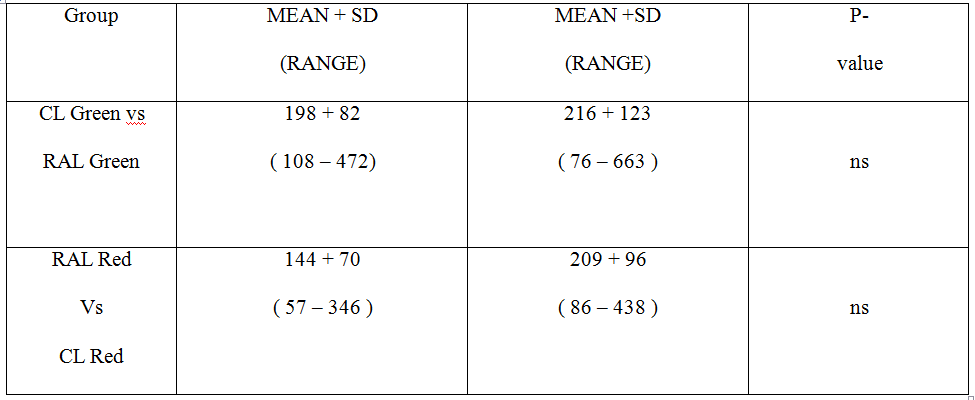
Time in sec of each group of participants
Table 5 : Tying a knot
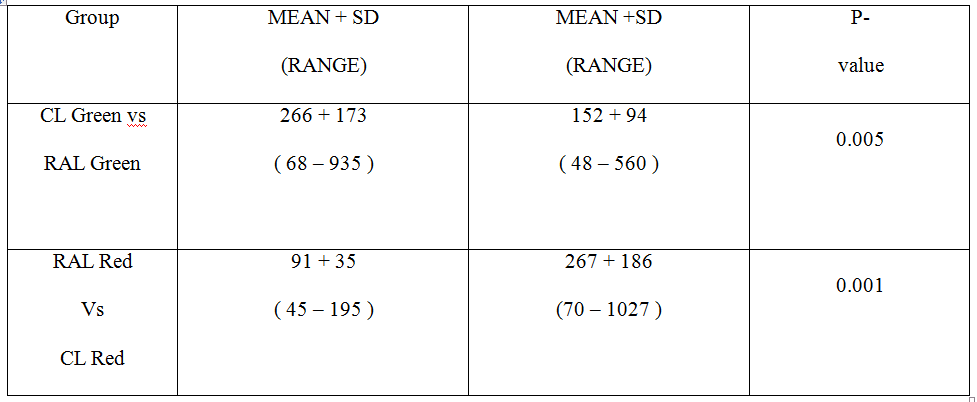
Time in sec of each group of participants
Table 6 : Qualitative parameters for all 30 participants after four repeats with RAL & CL expressed as number of time they occurred (n)
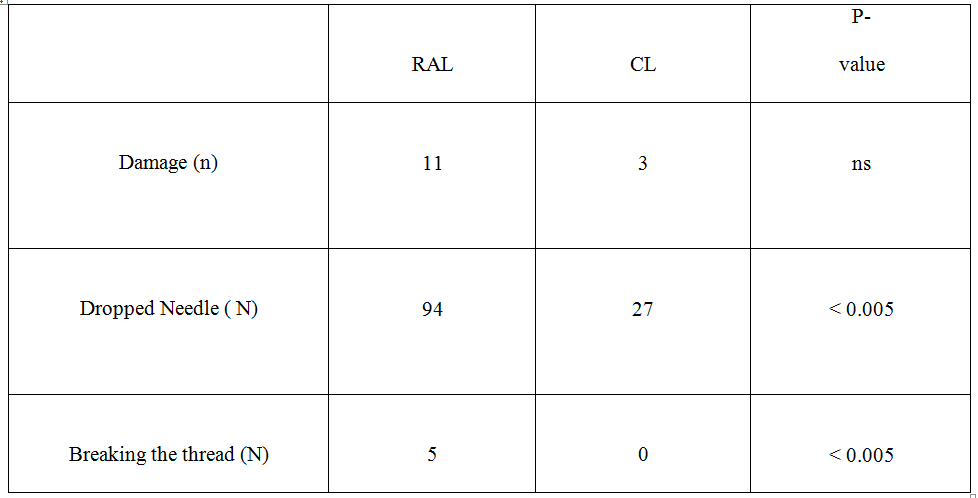
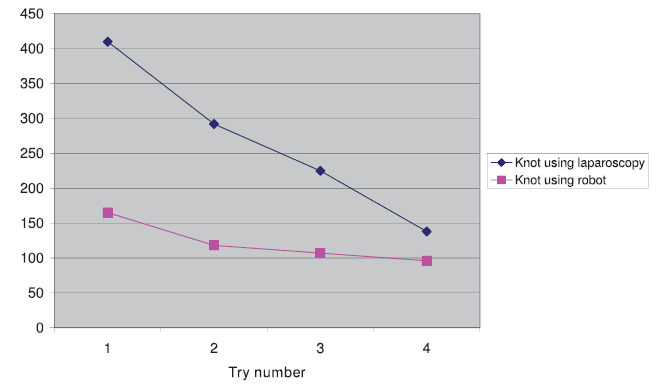
Fig 4 : The mean time for each try to tie a knot for the 30 subjects with CL & RAL in Seconds .
Discussion:
Very few studies comparing the learning curves of RAL and CL have been published. In the experimental setting a diversity of parameters, not always well-defined, has been used for analysis of learning curves and only the very beginning of the learning curve is studied. In the clinical setting, an experience bias has been expected due to prior laparoscopic experience of the participating surgeons [2,6-12]. Both experimental and clinical studies show diverging learning curves for robotic surgery. The results of previous studies are not conclusive and to objectively evaluate the learning curve of robotic surgery is difficult.
Our experimental study included participants without any prior experience of open surgery, RAL or CL, making the group homogeneous. The performed tasks, well-defined and described, closely mimicked some of the proper surgical procedures used every day in the operating theatre. We used the only robotic surgical system currently on the market and standard CL instruments. The size of our group of participants and the number of repetitions studied was decided after power calculation.
The task of tying a surgical knot was always faster with RAL than with CL, even when the participant had gained no experience by carrying out the first part of the study with CL. There are learning curves seen for tying a knot for both RAL and CL when comparing trials 1 and 4. The learning curve is steeper for CL but the curves never cross (Figure 4). These findings differ from most previous studies where the initial performance with RAL is often inferior to the performance with CL [3]. In a recent publication by Stefanidis et al. the authors reported that robotic assistance significantly improved intracorporeal suturing performance and shortened the learning curve. They also reported that performance of laparoscopic knot tying without robotic assistance did not improve after three repeats [13]. The first statement is supported by our study but the latter is not since we also saw a significant learning curve for CL. Performing more advanced tasks like tying a knot might be faster for maiden users due to the fact that RL is more "intuitive" with instrument movements mimicking normal hand movements. This is supported by some authors [4]. The fact that RAL is performed with 3-dimensional vision instead of the 2-dimensional vision in CL might also improve the performance, as has been suggested by others [7,14].
The transfer effect, with a faster performance if the specific method was used as the second part of the study when the tasks had already been tried by the first method, was seen for continuous suturing and tying a knot with RL, but not for CL. This might be interpreted as the RAL method being easier to adapt to once acquaintance had been made with the tasks themselves, at least for maiden users. The study by Blavier et al. showed worse performance when shifting from one method to the other in both directions. The shorter learning curve for RAL noted by the same authors is supported by our study [7].
The learning curve consists of an initial steep phase in which performance improves rapidly. When the change in improvement slows down, the learning curve reaches a plateau phase in which variability in performance is small. The number of repetitions reported here are too low to reach consistency, which characterizes the end of the learning curve. The learning curve for CL was steeper, but the number of repetitions too few to disclose a complete learning curve. This was not the aim of the study. We concentrated on the first phase of the learning curve in order to detect even small changes or differences between the two techniques used. From our data, we can therefore only conclude that it is initially easier for novice subjects to use robotic assistance for the specific tasks using the set performance parameters. Whether or not the curves for RAL and CL eventually cross after more repetitions, or when the plateau phase of the learning curve for each technique is reached, remains unclear. This could be the aim of another study in the future.
The objective structured assessment of technical skill (OSATS) described by Reznick et al. is a validated tool widely used in the education literature. The OSATS is feasible, reliable and can be used for testing technical competence with high clinical relevance [15]. Since we focused on comparing the different repeats and the transfer effect in all three tasks we did not calculate a total score for the time and accuracy parameters.
Dropping the needle was more common in the RAL group. Half of the subjects dropped the needle while performing CL and all but two while performing RAL. Furthermore, the thread was only torn when using RAL. Tactile feedback is not yet possible in RAL, which is the most probable explanation for our findings.
In spite of these differences, albeit significant, the performance when using RAL was not slower in the task "continuous suturing" compared with CL. Without the dropping of the needle in the task "continuous suturing", RAL might have been faster. Learning curves are also seen for a continuous suture for both RAL and CL when comparing trials 1 and 4 (Figure 5). The two figures 4 and 5 express the mean time for each try for the specific task but do not consider in what order the task is performed. As already stated, no difference was noted between RAL and CL for "continuous suturing". Clinical reports have indicated that the improved vision in RAL seems to make up for the lack of tactile feedback for more experienced surgeons [5]. The tearing of threads and dropping of needles is probably a greater challenge to the beginner.
The end points of our study, time and accuracy, may not be the best end points to measure. Length of pathway and economy of movement might be better predictors of learning curve and safe performance of laparoscopic surgery. A further possible limitation of our study is that error reduction, an important goal of training, was not measured. The study of Narazaki et al. suggests that both task completion time and distance travelled is shortened with training in novice users[10].
The suggested advantage of faster laparoscopy in the RAL group might not be relevant in clinical surgery since inexperienced users are not supposed to perform advanced laparoscopic surgery. Robotic surgeons today are often senior surgeons and already expert laparoscopists. However, the training to become an expert takes a lot of time and is costly, so learning curves are important also for the future education of young surgeons. If RAL is proven easier to master with equal or better results than CL, robotic surgery could be an option for efficient surgical training. The many steps of a surgical intervention each have a learning curve and if learning curves are shorter for RAL it may have some clinical relevance even at later stages of training.
RAL is still in its infancy but offers great opportunities for the future. Major improvements in the availability of tactile feedback and specifically designed instruments are necessary and expected soon. More research needs to be done to define the exact indications for RAL to justify the increased costs and the increased time consumption involved, compared with CL.
Whether or not these features with improved accuracy, dexterity and visualization enhance surgical performance remains unclear.
Conclusion:
In conclusion, we found support for our hypothesis that a surgical task, such as tying a knot, was performed faster using RAL than with CL, while easier surgical tasks could be performed equally fast with either technique. The lack of tactile feedback in RAL is a factor to consider at least for maiden users. Experience from one technique was transferred to the other. Our data do not support the suggestion that considerable CL experience is important for those starting to use RAL. On the other hand, previous experience did matter in our study. No difference between the performances of male and female subjects was noted.
References :1. Subramonian K, Desylva S, Bishai P, et al: Acquiring surgical skills: a comparative study of open versus laparoscopic surgery. Eur J Urol 2004, 45:346-351.
2. Heemskerk J, van Gemert WG, de Vries J, Greve JW, Bouvy ND: Learning curves of Robot-assisted Laparoscopic Surgery Compared With Conventional Laparoscopic Surgery: An Experimental Study Evaluating Skill Acquisition of Robot-assisted Laparoscopic Tasks Compared With Conventional Laparoscopic Tasks in Inexperienced Users. Surg Laparosc Endosc Percutan Tech 2007, 17:171-174.
3. Olthof E, Nio D, Bemelman WA: The learning curve of robot-assisted laparoscopic surgery. Medical robotics Vienna: I-Tech Education and PublishingBozovic V 2008, 1-8.
4. Meehan JJ, Meehan TD, Sandler A: Robotic fundoplication in children: resident teaching and a single institutional review of our first 50 patients. J Pediatr Surg 2007, 42:2022-2025.
5. Meehan JJ, Sandler A: Pediatric robotic surgery: A single-institutional review of the first 100 consecutive cases. Surg Endosc 2008, 22:177-182.
6. Yohannes P, Rotariu P, Pinto P: Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 2002, 60:39-45.
7. Blavier A, Gaudissart Q, Cadière GB, Nyssen AS: Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 2007, 194:115-121.
8. Heemskerk J, van Gemert WG, Greve JW, Bouvy ND: Robot-assisted Versus Conventional Laparoscopic Nissen Fundoplication: A Comparative Retrospective Study on Costs and Time Consumption. Surg Laparosc Endosc Percutan Tech 2007, 17:1-4.
9. Anderberg M, Clementson Kockum C, Arnbjörnsson E: Robotic fundoplication in children. Pediatr Surg Int 2007, 23:123-127.
10. Narazaki K, Oleynikov D, Stergiou N, et al: Robotic surgery training and performance. Identifying objective variables for quantifying the extent of proficiency. Surg Endosc 2006, 20:96-103.
11. Hernandez JD, Bann SD, Munz Y, et al: Qualitative and quantitative analysis of the learning curve of a simulated task on the da Vinci system. Surg Endosc 2004, 18:372-378.
12. Ro CY, Toumpoulis IK, Ashton RC, et al: A novel drill set for the enhancement and assessment of robotic surgical performance. Stud Health Technol Inform 2005, 111:418-421.
13. Stefanidis D, et al: Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 2009, 24(2):377-82.
14. Byrn JC, Schluender S, Divino CM, et al: Three dimensional imaging improves surgical performance for both novice and experienced operators using the Da Vinci Robot system. Am J Surg 2007, 193:519-522.
15. Reznick , Richard , Regehr , Glenn , et al: Testing Technical Skills Via an Innovative “Bench Station” Examination. The American Journal of Surgery 1997, 173(3):226-230.
Appendices : Appendix I
Data Collection Sheet
Place of Study : World Laparoscopy Hospital,Gurgaon
Date :
Name of the Participant : …………………………………………………………………….
Gender: Age:
Experiences in MAS :
Task performed group : RAL …………………….. / CL …………………..
Signature of the Researcher Signature of the supervisor
Appendices : Appendix II
Informed Written Concept
I undersigned Trainee doctor at World Laparoscopy Hospital , Gurgaon , India ,has come to Know that Dr. A.H.M Azharul Islam M.MAS/ 001/2011D, The Global Open (TGO) University performing an experimental (practical based) research on learning curve of intra corporeal suturing between RALS & CLS by MAS beginners . He has explained all the reason & value behind this study. He also assures me that I have every right to withdraw myself from the study at any point of time. His act in this study is only an investigator.
I gladly agree to participate in the study.
Signature and Full name of the participant