Laparoscopic Cholecystectomy with Real-time Near-Infrared Fluorescent Cholangiography
Laparoscopic Cholecystectomy with Real-time Near-Infrared Fluorescent Cholangiography
Dr R K Mishra
Introduction
Sometimes, there are certain mistakes that can happen during laparoscopic cholecystectomy procedure. The most common mistake is usually the misidentification of the extrahepatic bile duct anatomy which can lead to bile duct injury. At World Laparoscopy Hospital now we have atarted using ICG during laparoscopic cholecystectomy. However, there is something that can be down about the mistake, or basically, the mistake can be avoided. In order to avoid the mistake, it requires the doctor to use a technique or tools that will enhance or promote the easier recognition of the biliary anatomy in the intraoperative procedure by use of near-infrared fluorescence cholangiography or imaging.
According to various studies on the use of the near-infrared cholangiography in laparoscopic cholecystectomy, the report showed that there was positive and successful intraoperative identification of the extrahepatic bile ducts. This reduced the likelihood of causing an injury to the bile ducts. This is however unlike the conventional imaging, whose results are usually not very successful.
Understanding laparoscopic cholecystectomy (LC)
Laparoscopic cholecystectomy is one of the most commonly performed procedures in various countries. The procedure itself is usually associated with bile duct injury due to a poor intraoperative identification of the extrahepatic bile ducts. However, that complication is usually rare and actually, it is associated with an incidence of 0.3 to 0.7%. However, it should be noted that when the mistake happens and there happens to be a bile duct injury, it can lead to various complications such as lower quality of life, morbidity and mortality that are clinically relevant, and extra costs.

Often an injury to the bile duct leads to leakage of bile and abdominal sepsis which can lead to the obstruction or blockage of bile duct with obstructive jaundice. This will eventually lead to orthotopic liver transplantation.
This complication should be detected as early as possible, however, if it is detected when it is late or has really advanced it can be difficult to manage the bile ducts injuries since they will have caused severe damage which progresses to biliary peritonitis, multiorgan failure, sepsis and eventually death. Therefore, you need to understand that this is a condition that can be fatal if not detected and managed early enough. As earlier mentioned, the intraoperative misidentification of the bile ducts anatomy is usually the main cause of bile ducts injury.
Fluorescence cholangiography can help to reduce the risk of the bile duct, by helping improve the orientation of the anatomy during laparoscopic cholecystectomy. When the doctor is able to identify the relevant anatomical structure, he is able to perform the operation easily without making any mistakes that can be costly and fatal to the patient. However, given this advantage, the procedure is yet to be adopted across the globe due to several reasons. One of the reason is that the procedure takes times, involves exposure to radiation and requires additional practitioners. Additional, the ability to clearly identify the relevant anatomical structure or interpret an intraoperative cholangiogram clearly to some extent depends on the expertise of the surgeon.
Understanding Real-Time Infrared cholangiography
On the other hand, real-time infrared fluorescent cholangiography requires is often performed after the intravenous injection of indocyanine green (ICG) is viewed as a better and new technique for easier recognition of the biliary anatomy. One is not exposed to radiation and the procedure does not require any additional manpower. This makes it easy and actually a real-time and a flexible technique to use during laparoscopic cholecystectomy. Since the procedure is able to provide real-time visual or identification of the bile duct relevant anatomy, the outcome of the surgery can be improved leading to almost 100% success rates in various patients.
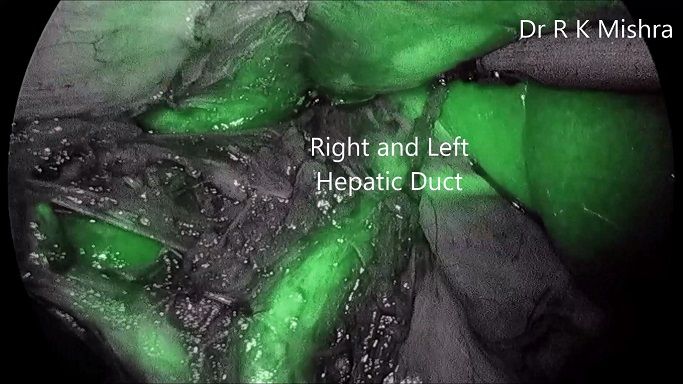
According to a clinical study, results showed that infrared cholangiography provided an improved and real-time identification of the extrahepatic bile ducts during the phase of CVS dissection. The identification was faster, in fact, up to 10 minutes of earlier identification of the cystic duct and the common bile duct was recorded. One of the best things about this procedure is that the liver is able to quickly and exclusively clear indocyanine green (ICG) that is often intravenously administered before the technique is put into action. Still, according to the clinical study, it was established that the real-time identification of the hepatic and cystic arteries was obtained after a repeated dose of intravenous injection of ICG.
Indocyanine Green (ICG)
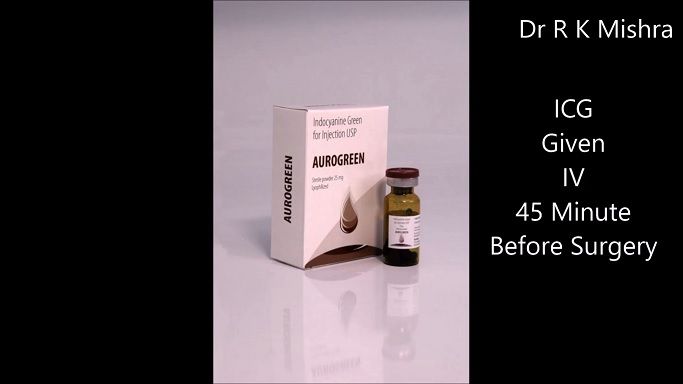
Indocyanine Green (ICG) is also known as the fluorescent dye. As earlier mentioned, the liquid is usually injected intravenously, it is actually the one that helps light the path for better and real-time identification of the biliary anatomy during the laparoscopic cholecystectomy.
The Near-Infrared Fluorescent Cholangiography is usually performed using, as its name goes, a fluorescent imaging system that is usually used together with a laparoscope. The system must have a lighting system that provides light for both infrared and xenon rays. To perform this cholangiography technique, the ICG must be administered at least 45 minutes before the procedure. This dye has been used for quite some time now, in fact, since 1956. Today, it is widely being used in almost every hospital for surgical and various clinical purposes.
ICG is able to provide better visualization of the biliary anatomy when it is illuminated by the infrared light, which makes it manifest fluorescence. When this happens the practitioner is able to clearly and in real time identify all the relevant biliary anatomy, thus enabling one to perform laparoscopic cholecystectomy better without causing injury to the bile ducts.
Therefore ICG acts as an imaging agent, which is sterile, water-soluble and has a peak spectral absorption averaging at 805 nm in blood plasma or simply the blood. Since it is exclusively eliminated by the liver, it does not undergo enterohepatic recirculation. It only stays in the bile for about 8 minutes after injection. The removal of ICG depends on several factors, including the blood flow of the liver, biliary excretion and parenchymal cellular function.
Sometimes, fluorescence may not be detected 45 minutes after the injection of ICG. Therefore, when this happens, the second dose of 2.5 mg of ICG can be administered intravenously also. A second injection of ICG can also be given if there is anything regarding perfusion that cannot be clearly understood during the surgery.
Exploration of the Biliary Anatomy
Practitioners always report their experience with Real-time near Infrared cholangiography using ICG. Most of the times when it comes to laparoscopic cholecystectomy, feasibility and safety of the technique are usually well reported.
The reports are quite interesting when it comes to RSSC where the ICG is still administered before the surgery and the biliary anatomy can be analysed before any dissection is made. This is quite different for cholangiography requiring extensive dissection of the cystic duct. Therefore using ICG during RSSC can help to analyse the extrahepatic biliary anatomy better and this could help reduce the bile duct injury due to the misinterpretation of the biliary anatomy. However, there are no data to prove this statement.
Other advantages of Real-time near Infrared Fluorescent Cholangiography
Near-Infrared Fluorescent Cholangiography improves the ability to analyze and identify the relevant biliary anatomic structure in a quick manner, therefore it can help reduce the time used in performing the procedure. Quicker assessment of the extrahepatic biliary anatomy is what is needed during laparoscopic cholecystectomy. The technique is usually able to shorten the operative time due to the fact there is no need to bring on board additional equipment and manpower, especially the radiology personnel for an x-ray.
The technique also serves as a good teaching tool for practitioners who are able to identify the relevant extrahepatic structures in almost every patient. This helps them become more experienced with the procedure which makes it easier for them to perform future procedures.
The technique does not require any X-ray, therefore, the no one is exposed to radiation. The ICG that is used is usually safe and does not cause any adverse reactions in patients. It is exclusively removed by the liver even before it undergoes enterohepatic recirculation. It is also a cost-effective technique that can help patients save some of their money that would otherwise have been used if the technique was not used.
However, near Infrared Fluorescent technique comes with some limitations. The common one is that it lacks the standardization of the fluorescence imaging systems. This is quite a drawback for this technique because standardization is needed for the determination of the objective assessments during any fluorescence-guided surgery like the laparoscopic cholecystectomy. The differences in fluorescence cholangiography make it difficult for the comparisons between fluorescence cholangiography studies.
Conclusion
The Real-time Near-Infrared Fluorescence Cholangiography is new and better technology that can help with the identification of the vital biliary anatomy. Several studies have been done on the technique and have been proven to be good for laparoscopic cholecystectomy. It helps to reduce the risk of the bile duct injury by proving clear vision of the vital extrahepatic structures. The reduced risk helps to avoid various complications that can arise from the injury of the bile duct which sometimes can be fatal to a patient.