Comparative study of veress needle and visiport in creating pneumoperitoneum in laparoscopic surgery
Comparative study of veress needle and visiport in creating pneumoperitoneum in laparoscopic surgery
Thesis submitted by:Dr. Sheela Prince
Roll No.: TGOU (N) 009/M.MAS/2014D
To the Global Open University
Department of Minimal Access Surgery
World Laparoscopy Hospital Center
Global Open University of Nagaland
In partial fulfillment for the Award of
Masters Degree in Minimal Access Surgery
January 2018
INTRODUCTION
In minimal surgery the technique of first entry in human body with the telescope and instruments is called access technique. It is important to know that 20% of laparoscopic complications are caused at the time of initial access. Developing access skill is one of the important achievements for the surgeons practicing minimal access surgery. First entry access in laparoscopy is of two types: Closed and open access.
In closed technique, veness needle is commonly used by minimal access surgeons worldwide but it is a blind technique. Nowadays, entry technique with optical trocars are used for visual guided access in to the abdomen. Here we are analyzing the merits and demerits of two entry techniques and the incidence of complications in both techniques. Comparison is between the blind technique by using veress needle and undervision technique by using visiport.
AIM OF STUDY
REVIEW OF LITERATURE
The word “Laparoscopy” originated from the greek word laparo which means abdomen and scopion – to examine. [2]
Laparoscopy is an art of examining the abdominal cavity and it’s contents. This is achieved by sufficiently distending the abdominal cavity (pneumoperitoneum) and visualizing the abdominal contents using illuminated telescope. [2]
The first laparoscopy in humans was performed by Jacobeus of Sweden in 1910 [7]. Since then, the laparoscopic techniques have been in constant evolution. Over the last two-three decades, it has become the preferred options for multitude of operative procedures [7].
Initially, laparoscopic surgery was termed minimally invasive surgery. But this term was changed to minimal access surgery as laparoscopic surgery is an invasive procedure associated with similar risks of major complications as compared with conventional open surgery [2].
Pneumoperitoneum is the first step in laparoscopic surgery [3]. Laparoscopic surgery was made possible later in the 20th century due to successful abdominal distention by introducing pneumoperitoneum initially nitrous oxide was used later on. It was replaced by a carbon dioxide. Carbon dioxide is colorless, non-toxic and non-inflammable, thus allowing the used of diathermy and laser. It also has the greatest margin of safety in case of venous embolism, as it is highly soluble. Diagnostic and therapeutic procedures have been carried out in the space created in the abdomen by the pneumoperitoneum and the initial penetration of the abdominal cavity to produce pneumoperitoneum [4].
In the last three decades, rapid advances in laparoscopic surgery have made it as an invaluable part of general surgery but there remains no clear consensus as an optional method of entry in to peritoneal cavity [12].
METHODS OF CREATING PNEUMOPERITONEUM [1, 9]
CLOSED METHOD:
In closed access technique, pneumoperitoneum is created by veress needle. This is a blind technique and most commonly practice method of access by surgeons worldwide [1]. The used of veress needle to create the pneumoperitoneum has inherent risks. It may cause vascular and visceral injuries [10]. Also, visually guided entry by optical trocars is a closed method. This permits smaller skin incision and better visualization of tissues as they are penetrated and have been shown in large series to be safe and fast ways to access the peritoneal space.
OPEN METHOD:
In this there is direct entry by open technique without creating pneumoperitoneum and insufflator is connected once blunt trocar is inside the abdominal cavity under direct vision. There are various ways of open access like Hasson’s techniques, Scandinavian techniques and fielding techniques.
ANATOMY OF THE ANTERIOR ABDOMINAL WALL
There are three large flat muscles (external oblique, internal oblique, transverses abdominis) and one long vertically oriented segmental muscle (rectus abdominis) on it’s side. And four major arteries are present in the anterior abdominal wall which form an anastomotic arcade that supplies the abdominal wall on either side. They are superior and inferior epigastric arteries, musculophrenic artery, deep circumflex iliac artery.
Umbilicus is the site of choice for access. It is the scar remaining after the umbilical cord obliteration. At the level of umbilicus, skin peritoneum and fascia are fused together with minimum fat. The midline is free of muscle fibers, nerves and vessels except at its inferior edges where pyramidalis muscle is sometimes found. Trocar side in this locations rarely cause much bleeding. The colon is attached to the lateral abdominal wall along both gutters and puncture laterally should be under video control to avoid visceral injury.
OPERATING ROOM SET UP
An organized well equipped operation theatre is essential for successful laparoscopy. The entire surgical team should be familiar with instruments and their functions. The entire instruments should be placed according to the convenience of surgeon so that it should be ergonomically perfect for that surgery. The co-axial alignment should be maintained. The eye of the surgeon, target of the dissection and monitor should be placed in the same axis.
PATIENT POSITION
Initially at the time of pneumoperitoneum by veress needle, patient should be placed supine with 10-20 degree head down. The benefit of this steep Trendelenburg position is that bowel will be pull up and there will be more room in the pelvic cavity for safe entry of veress needle. If the surgeon is planning to insert the veress needle pointing towards pelvic cavity. If the surgeon is planning to insert the veress needle perpendicular to the abdominal wall as in case of very obese patient or diagnostic laparoscopy under local anesthesia, the patent should be placed in supine position otherwise all bowel will come just below the umbilicus and there is increase risk of bowel injury.
POSITION OF THE SURGICAL TEAM
Laparoscopic surgeon is very much dependent and helpless with eye fixed on monitor. In laparoscopic upper abdominal surgery, French surgeons like to stand between legs of the patient popularly known as French position. The American surgeons like to operate from left side in cases of upper abdominal surgery like fundoplication in hiatus hernia and cholecystectomy called American position. In most of the cases, at the time of access, surgeons should stand on the left side of the patient if the surgeon is right handed. If the surgeon is left handed, he should stand right to the patient at the time of access. This helps in inserting veress needle and trocar towards pelvis by dominant hand. Once all the ports are in position, the surgeon should come to the opposite side to target the organ to start surgery.
In most of the upper abdominal surgery, camera assistant should stand left to the surgeon and in lower abdominal surgery he/she should stand right to the surgeon. The surgeon should work in the most comfortable and less tiring position possible with shoulder relaxed, arms along side of body, elbow 90 degree and forearms horizontal.
PREPARATION FOR ACCESS
Before starting access the abdomen should be examined for any palpable lump. It is wise to tell the patient to void urine before coming to operating room but if the bladder is found full at the time of palpation, Foley’s catheter should be inserted. Full bladder maybe injured very easily by veress needle or trocar.
CHOICE OF GAS FOR PNEUMOPERITONEUM
Initially in the beginning period of laparoscopy, pneumoperitoneum was created by filtered room air. Carbon dioxide and nitrous oxide are now preferred gas because of increased risk of air embolism with room air. Carbon dioxide is used for insufflation as it is 200 times more diffusible than oxygen.
SITE OF VERESS NEEDLE ENTRY
There are many sites of veress needle insertion but central location of the umbilicus and the ability of the umbilicus to hide scar makes it more attractive site for primary port. Umbilicus is good site for access because:
PALMER’S POINT [16]
In patients with previous laparotomy, palmer advocated insertion of the veress needle 3 cm below the left subcostal border [9].
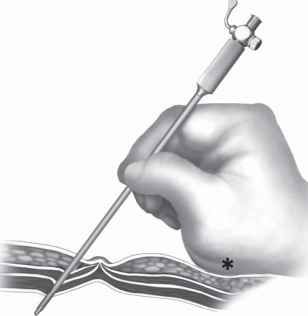
INTRODUCTION OF VERESS NEEDLE
Veress needle should be held like a dart at the time of insertion there should be 45 degrees of elevation angle. Elevation angle is the angle between the instrument and the body of the patient. Distal end of the veress needle should be pointed towards rectum [1]. Commercially available veress needles vary from 12 to 15 cm with the external diameter of 2 mm [12].
A bezel shape tip enables the needle to pierce the tissue of the abdominal wall upon entering the peritoneal cavity the resistance generated from the abdominal wall is overcome which permits the interior needle with its blunt atraumatic mandril. This system affords a degree of safety and efficacy making the puncture of peritoneal cavity with a veress needle an easy, fast and effective technique. Once the peritoneal cavity is inflated by this technique, the first trocar can be inserted without problem minimizing intraoperative gas leakage and saving surgical time [12].
INDICATORS OF VERESS NEEDLE INSERTION [1]
It is important to keep nice hold on the veress needle throughout while gas is flowing otherwise veress needle can slip out and make create pre peritoneal insufflation.
QUADROMANOMETRIC INDICATORS OF INSUFFLATION
PRIMARY TROCAR INSERTION AFER VERESS NEEDLE INSUFFLATION
Patient position is important, patient should be placed supine with 10-20 degree head down.
Site: Same site of veress needle entry should be used for primary trocar insertion.
INTRODUCTION OF PRIMARY TROCAR
Hold the trocar in such a way that head of trocar should rest on the thenar eminence middle finger should encircle air inlet and index finger should point towards sharp end.
Angle of insertion: Initially angle of insertion of primary trocar should be perpendicular to the abdominal wall but once surgeon feels giving way sensation the trocar should be tilted to 60-70 degrees angle.
Confirmation of entry of primary trocar:
USE OF VERESS NEEDLE IN OBESE PATIENT
In obese patient, the incision should be trans umbilical (base of umbilicus) for veress needle insertion as this is the thinnest part of the abdominal wall and less fatty area. The direction of the veress needle entry in the obese patient should be perpendicular. And pneumoperitoneum created up to 18 mm of Hg [1].
ENTRY IN CASE OF MORBID OBESITY
Morbidly obese patient it is virtually impossible to lift the abdominal wall and the veress needle need to be introduce perpendicular to the abdominal wall trans-umbilically without lifting [1, 12]
VISUAL GUIDED ENTRY
Optical trocars are used for visual guided entry, this permits smaller skin incision and better visualization of tissues as they are punctured and have been shown in long series to be safe and fast way to access peritoneal space. Injuries can be recognized immediately thereby reducing their potential morbidity. Disadvantage includes the inability to remove the trocar during its initial advancement which may change the original tract and confuse orientation. In addition making it difficult to recognize the peritoneal layer.
Optical trocar has been the bariatric surgery gold standard for minimally invasive peritoneal access [38]. Now these trocars are also being used after insufflation with veress needle. In visport, a single use optical obturator that includes a blunt clear window at the distal end along with the crescent shaped knife blade and a pistol grip handle with trigger at the proximal end. And an opening to accommodate a 10 mm laparoscope. When the trigger is pulled, the blade extends approximately 1 mm and immediately retracts. This action permit controlled sharp dissection of the tissue layers. The laparoscope permits visualization as the obturator passed through the abdominal wall. It is essential to assure that the image is in clear focus prior to use with midline deployment. The subcutaneous fat, the linea alba, the peritoneal fat and peritoneum can be clearly and reliably visualized layer by layer. The combination of flow steady gently pressure with the firing of blade only through these recognizable abdominal wall layers are essential components of safe entry.
COMPLICATIONS OF ACCESS TECHNIQUE [4, 12, 38]
Improper veress needle insertion and trocar insertion causes most of the operative complications of laparoscopic surgery [14]. Injuries to the bowel, major vessels, bladder, inferior epigastric vessels and subcutaneous emphysema.
VISCERAL INJURY
In minimal surgery the technique of first entry in human body with the telescope and instruments is called access technique. It is important to know that 20% of laparoscopic complications are caused at the time of initial access. Developing access skill is one of the important achievements for the surgeons practicing minimal access surgery. First entry access in laparoscopy is of two types: Closed and open access.
In closed technique, veness needle is commonly used by minimal access surgeons worldwide but it is a blind technique. Nowadays, entry technique with optical trocars are used for visual guided access in to the abdomen. Here we are analyzing the merits and demerits of two entry techniques and the incidence of complications in both techniques. Comparison is between the blind technique by using veress needle and undervision technique by using visiport.
AIM OF STUDY
- To study and compare the merits of closed (blind) technique of creating pneumoperitoneum and clear view (undervision) technique of visiport in creating pneumoperitoneum in Laparoscopic surgery.
- To assess evaluate and compare the incidence of complications in blind and clear view access techniques in laparoscopic surgery.
REVIEW OF LITERATURE
The word “Laparoscopy” originated from the greek word laparo which means abdomen and scopion – to examine. [2]
Laparoscopy is an art of examining the abdominal cavity and it’s contents. This is achieved by sufficiently distending the abdominal cavity (pneumoperitoneum) and visualizing the abdominal contents using illuminated telescope. [2]
The first laparoscopy in humans was performed by Jacobeus of Sweden in 1910 [7]. Since then, the laparoscopic techniques have been in constant evolution. Over the last two-three decades, it has become the preferred options for multitude of operative procedures [7].
Initially, laparoscopic surgery was termed minimally invasive surgery. But this term was changed to minimal access surgery as laparoscopic surgery is an invasive procedure associated with similar risks of major complications as compared with conventional open surgery [2].
Pneumoperitoneum is the first step in laparoscopic surgery [3]. Laparoscopic surgery was made possible later in the 20th century due to successful abdominal distention by introducing pneumoperitoneum initially nitrous oxide was used later on. It was replaced by a carbon dioxide. Carbon dioxide is colorless, non-toxic and non-inflammable, thus allowing the used of diathermy and laser. It also has the greatest margin of safety in case of venous embolism, as it is highly soluble. Diagnostic and therapeutic procedures have been carried out in the space created in the abdomen by the pneumoperitoneum and the initial penetration of the abdominal cavity to produce pneumoperitoneum [4].
In the last three decades, rapid advances in laparoscopic surgery have made it as an invaluable part of general surgery but there remains no clear consensus as an optional method of entry in to peritoneal cavity [12].
METHODS OF CREATING PNEUMOPERITONEUM [1, 9]
- Closed Method:
- Blind method
- Veress needle
- Direct Trocar entry method
- Undervision
- Clear view (optiview) trocar
- Veress needle with optiview technique
- Open Method
- Hasson’s technique
- Scandinavian technique
- Fielding technique.
CLOSED METHOD:
In closed access technique, pneumoperitoneum is created by veress needle. This is a blind technique and most commonly practice method of access by surgeons worldwide [1]. The used of veress needle to create the pneumoperitoneum has inherent risks. It may cause vascular and visceral injuries [10]. Also, visually guided entry by optical trocars is a closed method. This permits smaller skin incision and better visualization of tissues as they are penetrated and have been shown in large series to be safe and fast ways to access the peritoneal space.
OPEN METHOD:
In this there is direct entry by open technique without creating pneumoperitoneum and insufflator is connected once blunt trocar is inside the abdominal cavity under direct vision. There are various ways of open access like Hasson’s techniques, Scandinavian techniques and fielding techniques.
ANATOMY OF THE ANTERIOR ABDOMINAL WALL
There are three large flat muscles (external oblique, internal oblique, transverses abdominis) and one long vertically oriented segmental muscle (rectus abdominis) on it’s side. And four major arteries are present in the anterior abdominal wall which form an anastomotic arcade that supplies the abdominal wall on either side. They are superior and inferior epigastric arteries, musculophrenic artery, deep circumflex iliac artery.
Umbilicus is the site of choice for access. It is the scar remaining after the umbilical cord obliteration. At the level of umbilicus, skin peritoneum and fascia are fused together with minimum fat. The midline is free of muscle fibers, nerves and vessels except at its inferior edges where pyramidalis muscle is sometimes found. Trocar side in this locations rarely cause much bleeding. The colon is attached to the lateral abdominal wall along both gutters and puncture laterally should be under video control to avoid visceral injury.
OPERATING ROOM SET UP
An organized well equipped operation theatre is essential for successful laparoscopy. The entire surgical team should be familiar with instruments and their functions. The entire instruments should be placed according to the convenience of surgeon so that it should be ergonomically perfect for that surgery. The co-axial alignment should be maintained. The eye of the surgeon, target of the dissection and monitor should be placed in the same axis.
PATIENT POSITION
Initially at the time of pneumoperitoneum by veress needle, patient should be placed supine with 10-20 degree head down. The benefit of this steep Trendelenburg position is that bowel will be pull up and there will be more room in the pelvic cavity for safe entry of veress needle. If the surgeon is planning to insert the veress needle pointing towards pelvic cavity. If the surgeon is planning to insert the veress needle perpendicular to the abdominal wall as in case of very obese patient or diagnostic laparoscopy under local anesthesia, the patent should be placed in supine position otherwise all bowel will come just below the umbilicus and there is increase risk of bowel injury.
POSITION OF THE SURGICAL TEAM
Laparoscopic surgeon is very much dependent and helpless with eye fixed on monitor. In laparoscopic upper abdominal surgery, French surgeons like to stand between legs of the patient popularly known as French position. The American surgeons like to operate from left side in cases of upper abdominal surgery like fundoplication in hiatus hernia and cholecystectomy called American position. In most of the cases, at the time of access, surgeons should stand on the left side of the patient if the surgeon is right handed. If the surgeon is left handed, he should stand right to the patient at the time of access. This helps in inserting veress needle and trocar towards pelvis by dominant hand. Once all the ports are in position, the surgeon should come to the opposite side to target the organ to start surgery.
In most of the upper abdominal surgery, camera assistant should stand left to the surgeon and in lower abdominal surgery he/she should stand right to the surgeon. The surgeon should work in the most comfortable and less tiring position possible with shoulder relaxed, arms along side of body, elbow 90 degree and forearms horizontal.
PREPARATION FOR ACCESS
Before starting access the abdomen should be examined for any palpable lump. It is wise to tell the patient to void urine before coming to operating room but if the bladder is found full at the time of palpation, Foley’s catheter should be inserted. Full bladder maybe injured very easily by veress needle or trocar.
CHOICE OF GAS FOR PNEUMOPERITONEUM
Initially in the beginning period of laparoscopy, pneumoperitoneum was created by filtered room air. Carbon dioxide and nitrous oxide are now preferred gas because of increased risk of air embolism with room air. Carbon dioxide is used for insufflation as it is 200 times more diffusible than oxygen.
SITE OF VERESS NEEDLE ENTRY
There are many sites of veress needle insertion but central location of the umbilicus and the ability of the umbilicus to hide scar makes it more attractive site for primary port. Umbilicus is good site for access because:
- It is the thinnest abdominal wall.
- Cosmetically better.
- No significant blood vessels.
- Ergonomically better (center point of abdomen).
PALMER’S POINT [16]
In patients with previous laparotomy, palmer advocated insertion of the veress needle 3 cm below the left subcostal border [9].
INTRODUCTION OF VERESS NEEDLE
Veress needle should be held like a dart at the time of insertion there should be 45 degrees of elevation angle. Elevation angle is the angle between the instrument and the body of the patient. Distal end of the veress needle should be pointed towards rectum [1]. Commercially available veress needles vary from 12 to 15 cm with the external diameter of 2 mm [12].
A bezel shape tip enables the needle to pierce the tissue of the abdominal wall upon entering the peritoneal cavity the resistance generated from the abdominal wall is overcome which permits the interior needle with its blunt atraumatic mandril. This system affords a degree of safety and efficacy making the puncture of peritoneal cavity with a veress needle an easy, fast and effective technique. Once the peritoneal cavity is inflated by this technique, the first trocar can be inserted without problem minimizing intraoperative gas leakage and saving surgical time [12].
INDICATORS OF VERESS NEEDLE INSERTION [1]
- Needle movement test
- Once the veress needle is inside the abdominal cavity, the tip of the veress needle should be free and if the surgeon moves the tip of the needle gently then should not be any feel of resistance. It is very important that veress needle should not be moved inside the abdominal cavity much because there is risk of laceration of bowel to be punctured.
- Irrigation Test
- With 10 ml syringe, try to inject 5 ml of saline through veress needle. If the tip of the veress needle is inside, the abdominal cavity there will be free flow of saline, otherwise some resistance is felt on injecting saline.
- Aspiration Test
- After injecting saline, surgeon should try to aspirate that saline back through veress needle. If the tip of the veress needle is inside the abdominal cavity, irrigated water cannot be sucked out. But if it is in the preperitoneal space or in the muscle fiber or above the injected water can be aspirated back.
- Hanging drop test [12]
- Few drops of saline should be poured over the veress needle and the abdominal wall should be lifted slightly. If the tip of the veress needle is inside the abdominal cavity, the hanging drop should be sucked inside because inside the abdomen there is negative pressure. If the tip of the veress needle is anywhere else, hanging drop test will be negative [1].
It is important to keep nice hold on the veress needle throughout while gas is flowing otherwise veress needle can slip out and make create pre peritoneal insufflation.
- Insufflation of gas test (Quadromanometric test)
- For safe access, surgeon should always see carefully all the four indicators of insufflator at the time of creation pneumoperitoneum. Ig the gas is flowing inside the abdominal cavity, there should be proportionate rise in actual pressure with the total gas used.
QUADROMANOMETRIC INDICATORS OF INSUFFLATION
- Preset insufflation pressure
- Actual pressure
- Gas flow rate
- Volume of gas consumed
PRIMARY TROCAR INSERTION AFER VERESS NEEDLE INSUFFLATION
Patient position is important, patient should be placed supine with 10-20 degree head down.
Site: Same site of veress needle entry should be used for primary trocar insertion.
INTRODUCTION OF PRIMARY TROCAR
Hold the trocar in such a way that head of trocar should rest on the thenar eminence middle finger should encircle air inlet and index finger should point towards sharp end.
Angle of insertion: Initially angle of insertion of primary trocar should be perpendicular to the abdominal wall but once surgeon feels giving way sensation the trocar should be tilted to 60-70 degrees angle.
Confirmation of entry of primary trocar:
- Audible click if disposable trocar or safety trocar is used.
- Whooshing sound if reusable trocar is used.
- Loss of resistance felt both in disposable as well as reusable trocar.
USE OF VERESS NEEDLE IN OBESE PATIENT
In obese patient, the incision should be trans umbilical (base of umbilicus) for veress needle insertion as this is the thinnest part of the abdominal wall and less fatty area. The direction of the veress needle entry in the obese patient should be perpendicular. And pneumoperitoneum created up to 18 mm of Hg [1].
ENTRY IN CASE OF MORBID OBESITY
Morbidly obese patient it is virtually impossible to lift the abdominal wall and the veress needle need to be introduce perpendicular to the abdominal wall trans-umbilically without lifting [1, 12]
VISUAL GUIDED ENTRY
Optical trocars are used for visual guided entry, this permits smaller skin incision and better visualization of tissues as they are punctured and have been shown in long series to be safe and fast way to access peritoneal space. Injuries can be recognized immediately thereby reducing their potential morbidity. Disadvantage includes the inability to remove the trocar during its initial advancement which may change the original tract and confuse orientation. In addition making it difficult to recognize the peritoneal layer.
Optical trocar has been the bariatric surgery gold standard for minimally invasive peritoneal access [38]. Now these trocars are also being used after insufflation with veress needle. In visport, a single use optical obturator that includes a blunt clear window at the distal end along with the crescent shaped knife blade and a pistol grip handle with trigger at the proximal end. And an opening to accommodate a 10 mm laparoscope. When the trigger is pulled, the blade extends approximately 1 mm and immediately retracts. This action permit controlled sharp dissection of the tissue layers. The laparoscope permits visualization as the obturator passed through the abdominal wall. It is essential to assure that the image is in clear focus prior to use with midline deployment. The subcutaneous fat, the linea alba, the peritoneal fat and peritoneum can be clearly and reliably visualized layer by layer. The combination of flow steady gently pressure with the firing of blade only through these recognizable abdominal wall layers are essential components of safe entry.
COMPLICATIONS OF ACCESS TECHNIQUE [4, 12, 38]
Improper veress needle insertion and trocar insertion causes most of the operative complications of laparoscopic surgery [14]. Injuries to the bowel, major vessels, bladder, inferior epigastric vessels and subcutaneous emphysema.
VISCERAL INJURY
- Small bowel
- Large bowel
- Bladder
- Stomach
Solid Organs:
VASCULAR INJURY
- Liver
- Spleen
VASCULAR INJURY
- Inferior epigastric
- Omental vessel injury
- Mesenteric vessels
- Aorta
- Inferior vena cava
OTHER COMPLICATIONS [12]
- Gas embolism
- Pneumo omentum
- Surgical emphysema
- Port site hematoma [38]
NEWER DEVELOPMENTS IN ACCESS TECHNIQUE
- Veress needle with inbuilt fiber optic telescope – It is also used for direct visualization at the time of its introduction but quality of picture is not safe for introduction.
- Pneumoperitoneum using versa step system – The versa step system is an integrated system combining a nylon stretchable sheath over a disposable veress needle. Once inserted, the sheath is dilated by inserting the trocar (with dilator in place). The real advantage of the system is that it has no cutting entry blade thus, dramatically decreasing trocar site bleed and potential for an intraabdominal injury. In addition, it creates a small fascial defect, which does not need to be closed.