Ideal port positioning in different laparoscopic urological procedures
Ideal Port Positioning In Different Laparoscopic Urological Procedures
Submitted To The Global Open University, World Laparoscopy Hospital Centre, Cyber City, Gurgoan, Delhi Ncr, India.
BY:
Dr Bashir Yunusa
Roll No: - Tgou/Pg/2873/M. Mas/2011 J
Being A Partial Fulfilment Of The Requirements For The Award Of Masters Degree In Minimal Access Surgery, (M. MAS)
Contact details: World Laparoscopy Hospital, X-100, cyber city, Gurgaon, NCR Delhi, India-122002.
Ph: +919811416838, +91-0124-2351555
Website: www.laparoscopyhospital.com
Certification :
We have participated and supervised this research done by Dr Bashir Yunusa on “The Ideal Port Positioning in Different Laparoscopic Urological Procedures” conducted in our centre.
Dr J S Chowhan
MBBS, MS, F. MAS, PGDHHM
Coordinator
--------------------------------------------------
Dr (PROF.) R K Mishra
MBBS, MS, MWALS, MRCS, M MAS, F. MAS, D. MAS, FICRS, PhD
Professor and Head, Minimal Access Surgery,
TGO University of Nagaland and Medical Director,
World Laparoscopy Hospital
------------------------------------------------------------
DR BASHIR YUNUSA
C/o World Laparoscopy Hospital
Declaration :
I Dr Bashir Yunusa do hereby declare that this thesis titled “Ideal port positioning in different urologic laparoscopic procedures” has not been submitted in candidature for any other degree.
And I have no objections for this thesis to be copied in part or whole, or used for research purposes.
DR BASHIR YUNUSA
C/o World Laparoscopy Hospital
Acknowledgement :
I would like to sincerely thank my supervisors Dr (prof) R K Mishra and Dr J S Chowhan, and the entire staff crew of the World Laparoscopy Hospital Centre, of The Global Open University of Nagaland, for their tireless support and guide during my research work and thesis writing.
I am grateful to Alhaji Auwalu Abdullahi Rano. (A. A. Rano) for his financial support.
Thanks to my entire family members, friends and colleagues, Department of surgery and the Management of Aminu Kano teaching Hospital, Kano, Nigeria, for their support and assistance.
I thank all who have had a helping hand in making this book a reality.
Dedication :
I have dedicated this thesis to my daughter Fatima
ABBREVIATIONS
HAL = Hand Assisted L aparoscopic
LA = Laparoscopic Adrenalectomy
LESS = Laparo Endoscopic Single-Site
NOTES = Natural Orifice Transluminal Endoscopic Surgery
Submitted To The Global Open University, World Laparoscopy Hospital Centre, Cyber City, Gurgoan, Delhi Ncr, India.
BY:
Dr Bashir Yunusa
Roll No: - Tgou/Pg/2873/M. Mas/2011 J
Being A Partial Fulfilment Of The Requirements For The Award Of Masters Degree In Minimal Access Surgery, (M. MAS)
Contact details: World Laparoscopy Hospital, X-100, cyber city, Gurgaon, NCR Delhi, India-122002.
Ph: +919811416838, +91-0124-2351555
Website: www.laparoscopyhospital.com
Certification :
We have participated and supervised this research done by Dr Bashir Yunusa on “The Ideal Port Positioning in Different Laparoscopic Urological Procedures” conducted in our centre.
Dr J S Chowhan
MBBS, MS, F. MAS, PGDHHM
Coordinator
--------------------------------------------------
Dr (PROF.) R K Mishra
MBBS, MS, MWALS, MRCS, M MAS, F. MAS, D. MAS, FICRS, PhD
Professor and Head, Minimal Access Surgery,
TGO University of Nagaland and Medical Director,
World Laparoscopy Hospital
------------------------------------------------------------
DR BASHIR YUNUSA
C/o World Laparoscopy Hospital
Declaration :
I Dr Bashir Yunusa do hereby declare that this thesis titled “Ideal port positioning in different urologic laparoscopic procedures” has not been submitted in candidature for any other degree.
And I have no objections for this thesis to be copied in part or whole, or used for research purposes.
DR BASHIR YUNUSA
C/o World Laparoscopy Hospital
Acknowledgement :
I would like to sincerely thank my supervisors Dr (prof) R K Mishra and Dr J S Chowhan, and the entire staff crew of the World Laparoscopy Hospital Centre, of The Global Open University of Nagaland, for their tireless support and guide during my research work and thesis writing.
I am grateful to Alhaji Auwalu Abdullahi Rano. (A. A. Rano) for his financial support.
Thanks to my entire family members, friends and colleagues, Department of surgery and the Management of Aminu Kano teaching Hospital, Kano, Nigeria, for their support and assistance.
I thank all who have had a helping hand in making this book a reality.
Dedication :
I have dedicated this thesis to my daughter Fatima
ABBREVIATIONS
HAL = Hand Assisted L aparoscopic
LA = Laparoscopic Adrenalectomy
LESS = Laparo Endoscopic Single-Site
NOTES = Natural Orifice Transluminal Endoscopic Surgery
Introduction :
Visualising scope was first introduced by Kelling in the peritoneum of a dog in the year 1901; a landmark in the history of surgery. However, it took decades for a perfected laparoscopic technique to be implemented, not until 1987, when Mouret performed a successful laparoscopic cholecystectomy for the first time.1
In the early years of laparoscopy, patients experienced a lot of inconvenience with greater post-operative pain at port sites and other complications of the procedures. The mistakes leading to these poor outcomes seem to be completely avoidable with use of simple application of principles physics.1
Over the years, there were significant changes in the surgical approaches, with patients and surgeons striving for fewer, smaller incisions with the goals to hasten post-operative recovery and cosmesis. Technology and instrumentation have undergone various modifications to accommodate these changes.1
Laparoscopic surgery provides patients with less painful surgery but is more demanding for the surgeon. The increased technological complexity and sometimes poorly adapted equipments have led to increased complaints of surgeon fatigue and discomfort during laparoscopic surgery. Ergonomic integration and suitable laparoscopic operating room environment are essential to improve efficiency, safety, and comfort for the operating team. Understanding ergonomics can not only make life of surgeon comfortable in the operating room but also reduce physical strains on surgeon.
While advances evolve, there come drawbacks, which are majorly twofold. In the first scenario, the surgeon experiences the ill effects from the surgery, and secondly, the patient is the victim. This statement might seem superficial and poorly reflective in the first glance but it answers a much deeper question. There have been multiple reports of carpal tunnel syndrome, 1 eyestrain and cervical spondylosis, thenar neuropathy due to awkward thumb grips in cases of piston grips among high volume laparoscopic surgeons. However, other unique complications are associated with gaining access to the abdomen for laparoscopic surgery. 2
In 1991, Clayman performed the first successful laparoscopic nephrectomy through multiple key holes incision. Since then the techniques have been developed to permit laparoscopic instrumentation through single incision or laparo-endoscopic single site surgery(LESS). Additionally, natural orifice trans-luminal endoscopic surgery (NOTES) eliminates the need for abdominal incision. 3
Laparoscopic urology has rapidly evolved since the mid-1990s through advances in video technology and instrumentation design and is currently a useful alternative to treat complex surgical diseases encompassing ablative as well as reconstructive urology. 4
With advancement in laparoscopic surgery, procedures are now being performed for coexisting abdominal pathologies simultaneously. There have also been sporadic reports of multiple laparoscopic procedures being combined for urological conditions and few short series demonstrating the feasibility of dual laparoscopic procedures in urology. Thereby reducing psychological stress, single anaesthesia, less medication, shorter hospital stay and considerable cost effectiveness. Prolonged operative time with attendant haemodynamic alterations due to the pneumoperitoneum was considered to be a limiting factor for the performance of concomitant procedures. Nevertheless, once the learning curve and the necessary expertise are achieved this problem can be overcome easily.5
The relative position of the instrument ports is very important in the performance of surgical procedures endoscopically. The angle the instruments make with the operative site and to each other should mimic, as far as possible, the natural relationship of the hands and eyes during conventional surgery, thereby avoiding wrong port position which is the commonest cause of stressful surgery.
Many surgeons (urologist inclusive) use umbilicus as their primary port site due to obvious reasons that, it is a scar, naturally weak area due to absence of all layers and its midpoint location of the abdomen’s greatest diameter make it an attractive trocar site for laparoscopic surgery.6
Improper trocar insertion causes most of the operative complications of laparoscopic surgery, from swording on one side, to injury to the bowel, major vessels, bladder, inferior epigastric vessels, and subcutaneous emphysema, abdominal wall contusions, trocar-site herniation with possible bowel obstruction, and trocar-site tumour implants. Fortunately, the overall incidence of complications is relatively low (about 2%) 6.
Although is no uniform consensus about port placements for advanced laparoscopic procedures, the baseball diamond concept should be respected. The placement of ports in most cases is currently dictated by the surgeons′ preference based on experience. Instruments are usually placed in a triangular fashion to ease manipulation along with adequate visualisation during laparoscopy, and the target organ should be 15-20 cm from the centre port used for placing the optical trocar. Generally, the two remaining trocars are placed in the same 15-20 cm arc at 5-7 cm on either side of the optical trocars. This allows the instruments to work at a 60°-90° angle with the target tissue and avoids problems of long handle due to too far or too near placement of ports and the problem of abdominal wall interference. If necessary, two more retracting ports can be placed in the same arc but more laterally so that instruments do not clash.1
Another factor to be considered during trocar placement is the limited length of instrument. If trocar is too far from the desired position, then one has to push abdominal wall towards target organ to gain some length, making movements less precise with attendant strain on the fingers and hand muscles. Equally, if the angle between the target and instrument if too wide or obtuse, manipulation of curved instrument is very difficult.1
Recently, GelPort laparoscopic systems have been introduced which restore spatial awareness and tactile feel while maintaining pneumoperitoneum, making rapid atraumatic manipulation, dissection, palpation and mobilisation of critical vessel by the surgeon′s hand possible. This has been shown to lead to improved procedural times and also has given impetus to the concept of Hand Assisted Laparoscopic Surgery. 1
An ideal manipulation angle (angle made by the two working instrument) is achieved by correct port positioning and this improves task efficiency and quality of performance, and should be between 45° and 60°. Manipulation angle ranging from 45° to 75° with equal azimuth angles is recommended. Manipulation angles below 45° or above 75° are accompanied by increased difficulty and degraded performance, while 90 and above has the greatest muscle work load . Task efficiency was reported to be better with equal azimuth angles than with unequal azimuth angles. Achieving equal azimuth angles may be difficult in many practical situations, but in principle, azimuth inequality should be avoided because it degrades task efficiency.1
There exists a direct correlation between the manipulation and the elevation angles. With a manipulation angle of 60°, the corresponding optimal elevation angle which yields the shortest execution time and optimal quality performance is 60°. Wide manipulation angles necessitate wide elevation angles for optimal performance and task efficiency. When a 30° manipulation angle is imposed by the anatomy or build of the patient, the elevation angle should be also 30° as this combination carries the shortest execution time. The best ergonomic layout for endoscopic surgery consists of a manipulation angle ranging from 45° to 75° with equal azimuth angles.1
Another approach is the Single port laparoscopy, and violets the concept of triangulation used in conventional laparoscopy. Instruments often cross each other, making the procedure "counter-counterintuitive". But steerable endoscopes, bent and articulating instrumentation, magnetic anchorage and guidance systems as well as flexible robotics have been developed to overcome these difficulties
In the early years of laparoscopy, patients experienced a lot of inconvenience with greater post-operative pain at port sites and other complications of the procedures. The mistakes leading to these poor outcomes seem to be completely avoidable with use of simple application of principles physics.1
Over the years, there were significant changes in the surgical approaches, with patients and surgeons striving for fewer, smaller incisions with the goals to hasten post-operative recovery and cosmesis. Technology and instrumentation have undergone various modifications to accommodate these changes.1
Laparoscopic surgery provides patients with less painful surgery but is more demanding for the surgeon. The increased technological complexity and sometimes poorly adapted equipments have led to increased complaints of surgeon fatigue and discomfort during laparoscopic surgery. Ergonomic integration and suitable laparoscopic operating room environment are essential to improve efficiency, safety, and comfort for the operating team. Understanding ergonomics can not only make life of surgeon comfortable in the operating room but also reduce physical strains on surgeon.
While advances evolve, there come drawbacks, which are majorly twofold. In the first scenario, the surgeon experiences the ill effects from the surgery, and secondly, the patient is the victim. This statement might seem superficial and poorly reflective in the first glance but it answers a much deeper question. There have been multiple reports of carpal tunnel syndrome, 1 eyestrain and cervical spondylosis, thenar neuropathy due to awkward thumb grips in cases of piston grips among high volume laparoscopic surgeons. However, other unique complications are associated with gaining access to the abdomen for laparoscopic surgery. 2
In 1991, Clayman performed the first successful laparoscopic nephrectomy through multiple key holes incision. Since then the techniques have been developed to permit laparoscopic instrumentation through single incision or laparo-endoscopic single site surgery(LESS). Additionally, natural orifice trans-luminal endoscopic surgery (NOTES) eliminates the need for abdominal incision. 3
Laparoscopic urology has rapidly evolved since the mid-1990s through advances in video technology and instrumentation design and is currently a useful alternative to treat complex surgical diseases encompassing ablative as well as reconstructive urology. 4
With advancement in laparoscopic surgery, procedures are now being performed for coexisting abdominal pathologies simultaneously. There have also been sporadic reports of multiple laparoscopic procedures being combined for urological conditions and few short series demonstrating the feasibility of dual laparoscopic procedures in urology. Thereby reducing psychological stress, single anaesthesia, less medication, shorter hospital stay and considerable cost effectiveness. Prolonged operative time with attendant haemodynamic alterations due to the pneumoperitoneum was considered to be a limiting factor for the performance of concomitant procedures. Nevertheless, once the learning curve and the necessary expertise are achieved this problem can be overcome easily.5
The relative position of the instrument ports is very important in the performance of surgical procedures endoscopically. The angle the instruments make with the operative site and to each other should mimic, as far as possible, the natural relationship of the hands and eyes during conventional surgery, thereby avoiding wrong port position which is the commonest cause of stressful surgery.
Many surgeons (urologist inclusive) use umbilicus as their primary port site due to obvious reasons that, it is a scar, naturally weak area due to absence of all layers and its midpoint location of the abdomen’s greatest diameter make it an attractive trocar site for laparoscopic surgery.6
Improper trocar insertion causes most of the operative complications of laparoscopic surgery, from swording on one side, to injury to the bowel, major vessels, bladder, inferior epigastric vessels, and subcutaneous emphysema, abdominal wall contusions, trocar-site herniation with possible bowel obstruction, and trocar-site tumour implants. Fortunately, the overall incidence of complications is relatively low (about 2%) 6.
Although is no uniform consensus about port placements for advanced laparoscopic procedures, the baseball diamond concept should be respected. The placement of ports in most cases is currently dictated by the surgeons′ preference based on experience. Instruments are usually placed in a triangular fashion to ease manipulation along with adequate visualisation during laparoscopy, and the target organ should be 15-20 cm from the centre port used for placing the optical trocar. Generally, the two remaining trocars are placed in the same 15-20 cm arc at 5-7 cm on either side of the optical trocars. This allows the instruments to work at a 60°-90° angle with the target tissue and avoids problems of long handle due to too far or too near placement of ports and the problem of abdominal wall interference. If necessary, two more retracting ports can be placed in the same arc but more laterally so that instruments do not clash.1
Another factor to be considered during trocar placement is the limited length of instrument. If trocar is too far from the desired position, then one has to push abdominal wall towards target organ to gain some length, making movements less precise with attendant strain on the fingers and hand muscles. Equally, if the angle between the target and instrument if too wide or obtuse, manipulation of curved instrument is very difficult.1
Recently, GelPort laparoscopic systems have been introduced which restore spatial awareness and tactile feel while maintaining pneumoperitoneum, making rapid atraumatic manipulation, dissection, palpation and mobilisation of critical vessel by the surgeon′s hand possible. This has been shown to lead to improved procedural times and also has given impetus to the concept of Hand Assisted Laparoscopic Surgery. 1
An ideal manipulation angle (angle made by the two working instrument) is achieved by correct port positioning and this improves task efficiency and quality of performance, and should be between 45° and 60°. Manipulation angle ranging from 45° to 75° with equal azimuth angles is recommended. Manipulation angles below 45° or above 75° are accompanied by increased difficulty and degraded performance, while 90 and above has the greatest muscle work load . Task efficiency was reported to be better with equal azimuth angles than with unequal azimuth angles. Achieving equal azimuth angles may be difficult in many practical situations, but in principle, azimuth inequality should be avoided because it degrades task efficiency.1
There exists a direct correlation between the manipulation and the elevation angles. With a manipulation angle of 60°, the corresponding optimal elevation angle which yields the shortest execution time and optimal quality performance is 60°. Wide manipulation angles necessitate wide elevation angles for optimal performance and task efficiency. When a 30° manipulation angle is imposed by the anatomy or build of the patient, the elevation angle should be also 30° as this combination carries the shortest execution time. The best ergonomic layout for endoscopic surgery consists of a manipulation angle ranging from 45° to 75° with equal azimuth angles.1
Another approach is the Single port laparoscopy, and violets the concept of triangulation used in conventional laparoscopy. Instruments often cross each other, making the procedure "counter-counterintuitive". But steerable endoscopes, bent and articulating instrumentation, magnetic anchorage and guidance systems as well as flexible robotics have been developed to overcome these difficulties
Objective Of The Study :
To determine Ideal Port positioning in different Laparoscopic procedures by finding the shortest time for each procedure at a given port positions and respective manipulation angles.
2.1 Literature Review
2.2 Laparoscopic Nephrectomy And Port Positioning :
There are various approaches to nephrectomy and the placement of ports depends on the approach and the side, and weither or not a single site laparoendoscopic approach is intended.
2.3 Transperitoneal Approach :
In this approach usually a 12–mm port is placed at umbilicus by open Hasson technique, which is often primarily used as a camera port. Another 12–mm laparoscopic port is placed between umbilical port and anterior superior iliac spine (spinoumbilical port) and a 5–mm port is placed in line with the camera port at about 3 cm below the costal margin and 3 cm lateral to the midline. The fourth usually for retraction if needed, is a 5 mm port placed 4 cm below the costal margin in anterior axillary line.7 Both kidneys have similar approach on either side.
Another approach is to place the laparoscopic port on the mid-clavicular line just at or above the upper border of the umbilicus. A working port usually 10/12mm is positioned a finger-breadth below the costal margin on the anterior axillary line. A second working port, is placed on the anterior axillary line just above the superior iliac crest. An additional working port may be placed on the mid-axillary line mid-way between the costal margin and the superior iliac crest to provide access for a retracting instrument and to mobilize the kidney laterally. For the extremely thin patient the port sites are all moved medially with the laparoscope at the umbilicus, the working ports on the mid-clavicular line and an additional port on the anterior axillary line.8
One other approach for the left kidney is to place the camera port at the paraumblical space at the lateral border of the rectus muscle at the level of the umbilicus while the patient is placed in the right lumbotomy position; through the open introduction technique according to Hasson. One additional 10-mm, and one 5-mm trocar are then inserted under laparoscopic vision in the epigastric and mid-clavicular positions.9
The left kidney can also be approached with the camera port placed just to the left of the umbilicus. The left hand 12-mm port placed along the lateral border of the rectus abdominis muscle lateral to the umbilicus. The right hand port placed on the lateral border of the rectus near the dome of the bladder. A fourth port to be placed laterally to retract the sigmoid colon medially.10
2.4 The Retroperitoneal Approach :
In the retroperitoneal laparoscopic approach, incision is made at tip of 12th rib and then blunt dissection or balloon used to create space and the working port is placed between the midaxillary line and the anterior axillary line (5cm above the iliac crest). A 5mm port is then inserted at the junction of the 12th rib and paraspinal muscles (renal angle).11
Another approach through the retroperitoneal space is obtained through a 15-20mm incision just below the tip of the 12th rib and the secondary ports are then placed along the inferior border of the costal margin using digital palpation through the balloon dilated incision site. After digital placement of all the secondary ports, the primary balloon-tip port is inserted. The posterior secondary 12mm port is placed at the lateral border of the paraspinal muscle along the inferior border of the 12th rib. An anterior port is placed near the anterior axillary line, just below the inferior tip of the 11th rib. An additional 5mm port may be placed, on the mid-axillary line at or above the level of the superior iliac crest, and used for retraction and suction. Often a 12 mm port is placed at Petit’s triangle just above the midportion of the iliac crest and a fingerbreadth superior to the iliac crest. 8
2.5 Hand-Assissted Laparoscopic (Hal) Nephrectomy:
The hand-assisted device for right renal surgery could be located at and just below the umbilicus on the midline. Alternatively, on the right side the hand port may be placed as a Gibson incision in the right lower quadrant. A port is placed on the mid-clavicular line just above the superior iliac crest; the laparoscope is positioned at this port site. A 12mm port is placed two finger breadths below the costal margin on the mid-clavicular line, to accommodate the EndoGIA stapling device. A 5mm port is placed on the mid-line in the epigastric region for placement of an instrument to retract the liver superiorly and medially.8
Conversely, on the left the incision for the HAL device is located on the midline, at and above the umbilicus on the mid- clavicular line just above the superior iliac crest, a 10mm port placed for positioning of the 10mm, 30 degree laparoscope. The laparoscope may then be used for visualization of the HAL device incision. An additional 12mm working port is placed on the mid-clavicular line 2 finger breadths below the costal margin. Retraction of the kidney laterally may be facilitated by an instrument placed through a 5mm port in the mid-axillary line, mid-way between the costal margin and superior iliac crest.8
2.6 Laparoendoscopic Single Site (Less) Nephrectomy) :
Since the advent of laparoscopy, urologist have tried to minimize scars and improve cosmesis, leading to the progression to laparoendoscopic single site urological procedure. Access is usually gain through the umbilicus, but others include trans abdominal or retroperitoneal flank approach, a suprapubic or mini pfannesteil approach or Gibson incisions.12
Either a specialised port or cluster conventional port can be used to obtain access. Conventional laparoscopic techniques are generally followed, although modifications in techniques and manoeuvres unique to single site surgeries are employed.12
During LESS nephrectomy, a peri- umbilical incision is made to the rectus fascia. The peritoneum is entered with an extra-long trocar. After pneumoperitoneum, another trocar, is placed 1-1.5 cm caudal and at the 4 o'clock position to the extra-long trocar, eventually functioning as the camera port. A 12 mm port is inserted 1.5 cm caudal to the second trocar, resulting in triangular configuration. A fourth 12 mm standard length trocar is placed 1 cm cephalad to the umbilical protuberance, through which liver or splenic retraction and control of the renal upper pole and adrenal gland is achieved.13
2.7 Natural Orifice Transluminal Endoscopic Nephrectomy :
Natural orifice trans luminal endoscopic surgery (NOTES), with the objective of incision free abdominal surgery through natural orifices, (mouth, vagina and rectum) has been described. Although there were reports on successful completion of six laparoscopic transvaginal nephrectomies using conventional instruments in a porcine model, there were note of limitations of the laparoscopic instruments making the procedure cumbersome and time consuming. Clayman and colleagues reported their experience with single port NOTES transvaginal nephrectomy and encountered similar difficulty until a purpose built multi lumen operating instruments were made available.14
Hybrid NOTES in which two natural orifices are used for approaches has also been described and tried for nephrectomies. Transvaginal NOTES hybrid combined with either trans gastric or trans vesical nephrectomy, transvesical –trans gastric have all been described.15
2.8 Laparoscopic Pyeloplasty :
Standard port placement described as ports placed in the upper and lower quadrant midclavicular lines and the camera port placed near the umbilicus. An assistant port is placed in the suprapubic midline.16
Another approach with a primary port at 2.5 cm to the right of umbilicus, a 5 mm port midway between the primary port and right costal margin, and on right mid-clavicular line, and another 5 mm port midway between the antero-superior iliac spine and the umbilicus was used while the patient was placed in the 45 left lateral position. Fourth flank port is placed for retraction.17
2.9 Less Pyeloplasty :
The patient is positioned in a modified flank fashion, and a 2.5-cm incision is made within the umbilical dimple to conceal the scar. After insufflation of the abdomen, three 5-mm trocars are placed through the anterior abdominal fascia in a triangular configuration. A 5-mm 45-degree laparoscope is used along with articulating laparoscopic instruments. The laparoscope is placed through the most medial trocar and positioned anteriorly in the abdomen so that the camera looks down onto the surgical field. The working instruments are placed through the 2 lateral trocar.18
2.10 Laparoscopic Adrenalectomy :
Laparoscopic adrenalectomy (LA) has become a gold standard in the management of most of the adrenal disorders, after it was decribed by Schuessler et al in 1993 and matched it success with open.19 Apart from advantages like early recovery, reduced hospital stay and cosmesis, the main benefits of LA over open adrenalectomy are decreased incidence of intra-operative and post-operative hemorrhage, decreased morbidity and mortality.
2.11 Transperitoneal Laparoscopic Adrenalectomy :
This involves putting 12mm port in the umbilicus or at the lateral border of rectus abdominis muscle just above the level of umbilicus. Two subcostal 5mm ports at midclavicular line and in the lateral border of the rectus and another 3.5mm subcostal trocar - anterior axillary line, for the left adrenals. The Right is approached through a mirror image and an additional epigastric port to the left of the liver for its retraction.20
Right adrenalectomy can also be performed with four ports. The primary Camera port 10 mm to be placed at about 3 cm lateral and cephalad to the umbilicus. Two working ports, 5 mm and 10 mm are placed in the midclavicular position, the upper one (5 mm) below the costal margin, and the lower one (10 mm), 10-12 cm below the upper one. Another 5 mm port is to be placed in the sub-xiphisternal position for liver retraction. A fifth 5 mm port, if required, is placed in the right anterior axillary line, to facilitate retraction or suction.20, 21
And another approach is to put the telescope’s trocar at the umbilicus while maintaining the positions of the other trocars.20 In the case of the left usually the first three ports are placed in a mirror image of the right. A fourth 5 mm port, if required, is placed in the left mid-axillary line to facilitate retraction 20, 21, 22
2.12 Retroperitoneal Lateral Laparoscopic Adrenalectomy :
Retroperitoneal lateral approach to the left adrenal gland is through an incision at the inferior edge of the 12th rib in which the camera port is placed, the second port 5mm at anterior axillary line midway between the iliac crest and costal margin, third port is placed posteriorly between the 12th rib and iliac crest along the lateral border of sacrospinatus muscles and the fourth port for retraction is placed cephalad to the first port at anterior axillary line. The right side is a mirrow image of the left but the liver lobe is retracted percutaneously reducing the ports number to three.23
Retroperitoneal posterior approach described by Walz et al, and thoracoscopic transdiaphragmatic approach described by Gill et al are not commonly used.20
2.13 Less- Adrenalectomy :
The approach is usually through trans umblical incision and placement of multichannel single Gelport and 3.5mm ports for flexible laparoscope, SILS dissector and tissue sealing device; and the adrenal gland approached anteriorly in cases of right side with no mobilization of the right lobe of the liver, and the left is approached laterally.23 Retroperitoneal LESS adrenalectomy has also been described.
2.14 Laparoscopic Approaches To The Ureter :
A three port approach with primary port at the umbilicus, one 5 mm port midway between the umbilicus and the medial costal margin and a 5 mm port midway between the anterosuperior iliac spine and the umbilicus, was described.24
Umblical port with, ipsilateral hypochondrium and iliac fossa as working ports have been described for approaches to upper and mid ureter while ipsilateral paraumblical and suprapubic ports for lower ureter while maintaining the umblical port.25
In cases of retrocaval ureter. A three port approach with a primary port at 2.5 cm to the right of umbilicus, a 5 mm port midway between the primary port and right costal margin, and on right mid-clavicular line, and another 5 mm port midway between the antero-superior iliac spine and the umbilicus was used while the patient is placed in the left lateral position. Mobilization of the ureter in the interaortocaval region require additional 5 mm port to be inserted at the flank.17
LESS approach to lower ureter through suprapubic transvesical port has been described. 26
2.15 Laparoscopic Prostatectomy :
Laparoscopic simple or radical prostatectomy has been performed through almost the same approach. The commonly described conventional laparoscopy is through a primary port placed upper side of the umbilicus. Then secondary ports at upper margin of the pubic bone and levels of the anterior superior iliac spines bilaterally and the fifth port at a point midline at about 15cm from the pubic bone. 27, 28 while others described both iliac fossae for the last two ports, most especially when it is to be robotic assisted, 29 others described the distance of the second and third ports to be 8-10cm from the camera port. 30
Transumblical LESS radical prostatectomy was first described in 2008 by Kaouk and colleagues, through the umbilicus using a single three-channel port, and two years later Desai et al published the initial series of single-port transvesical simple prostatectomy where a single-port device inserted percutaneously into the bladder through a 2-3 cm incision in the suprapubic skin crease was used.5
2.16 Laparoscopic Cystectomy :
Laparoscopic cystectomy has been described by many authors, but remains to be evaluated and is far from being a standard procedure. While some described a similar approach to prostatectomy with peri-umblical port, two others 8-10 cms away from the primary port and then bilateral iliac fossae,31 others described only four ports approach with 3-4cm supra-umblical camera port and two iliac fossae ports and suprapubic port32 and the sixth port is only needed during urinary diversion in radical surgeries.33
In the hand assisted approach a 7cm peri umblical incision is made as the hand port, Camera is placed at the left of the hand port in the midclavicular line at the level of the umbilicus, a second port is placed 5cm below the level of the umbilicus at right midclavicular line. A 10mm port is placed in the left anterior axillary line and a 5mm at midline about 5cm above the pubic symphisis.34
Kaouk et al described the laparoscopic radical cystectomy and pelvic node dissection through a single umbilical port and an extracorporeal urinary diversion by way of extension of the umbilical port site.5
2.17 Laparoscopic Varicocelectomies :
Laparoscopic varicocelectomy is generally performed transperitoneally, but extra or retroperitoneal has also been described. And two trocars or single trocar approaches described, but generally three trocars are required especially in bilateral cases.35
Varicocelectomy is performed in a trans peritoneal laparoscopic fashion with two ports placed at supraumblical and caudal and lateral to the umbilicus on the contralateral side of the varicocele.36
For the three ports approach, some described the sub-umblical camera port with secondary trocars at midline half way between umbilicus and pubic symphisis, and the other at midclavicular line 1-2cm below horizontal line to the umbilicus while maintaining subumblical camera port, 37 while others described umblical primary port and both lower abdominal quadrants ports. 38, 39
2.18 Mitrofanoff :
A four port transperitoneal approach is described, with camera at umbilicus, two 5mm at left lower quadrant and right midaxillary line at the level of the umbilicus. Fourth port at left midaxillary also at umblical level. 40
2.19 Other Less Procedures :
Single-site laparoscopic surgery has been reported in small numbers for a variety of other urological conditions. A mesh sling has been successfully removed from the bladder via a transvesical approach. Sacrocolpopexies, orchidopexy and orchidectomy have been successfully performed through a single-incision without complication.5
Methodology
Justification For The Study :
This study was justified by the difficulties, prolonged operative time, and unnecessary additional ports and other complications of wrong port positioning challenging laparoscopic urologist during various procedures. This result will minimize if not completely eliminate the above mentioned problems.
Materials And Methods :
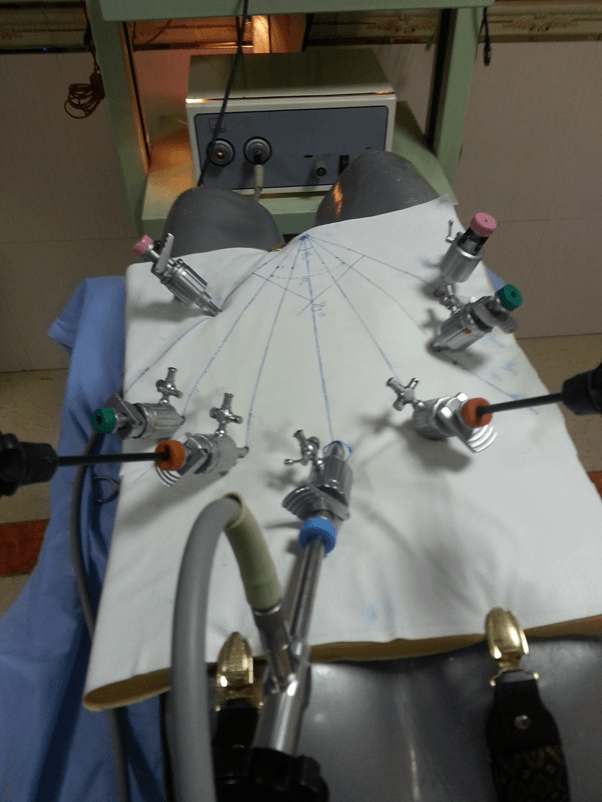
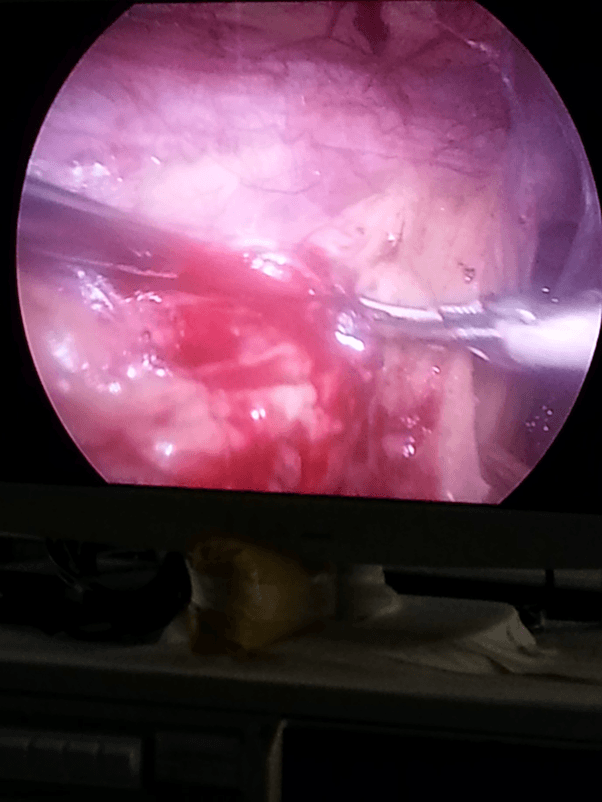
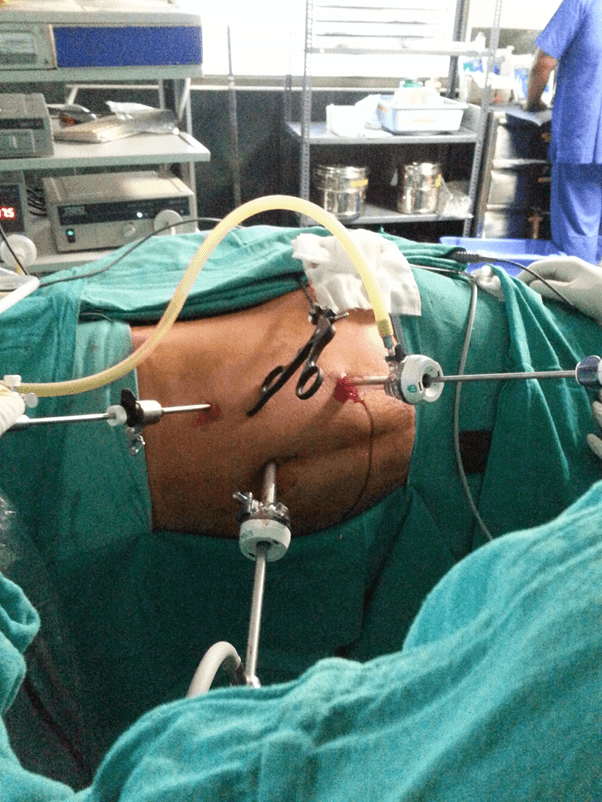
This study (descriptive cross sectional study) was conducted on both dry and wet laboratories; and also some data were recorded from living donour nephrectomies. Different ports were inserted at different positions and provided manipulation angles of 30, 60 and 90 degrees and were used to perform surgeon’s knots on the dummies, renal vessels ligation and uretero-ureteric anastomosis on the swine to represent common laparoscopic tasks performed in the region of the upper urinary tracts. Timing for the procedures performed by Diploma students who had similar exposure to laparoscopic training were recorded for the respective angles.
Pelvic ring transfer and surgeons knot were also performed on the dummies to represent the common procedures performed on the region of lower urinary tracts and timing and manipulation angles were kept as above. The recorded timings were validated using χ2, presented on tables and graphs. The timings of laparoscopic donor nephrectomy was taken, manipulation angles estimated, validated and presented on charts.
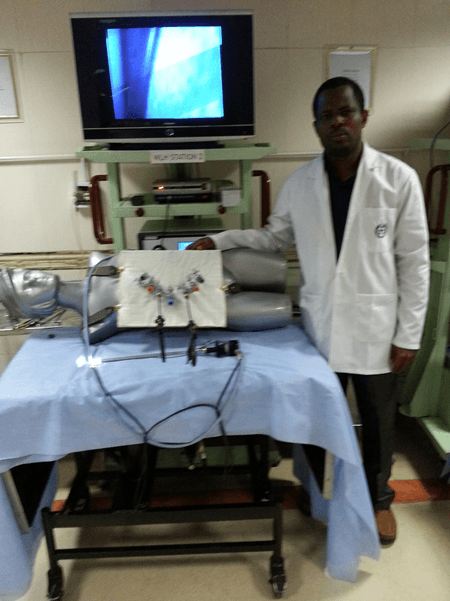
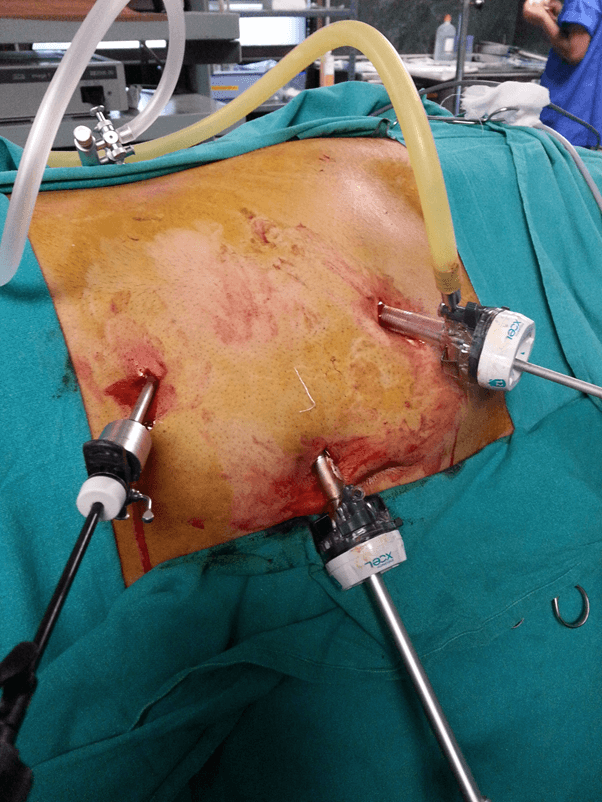
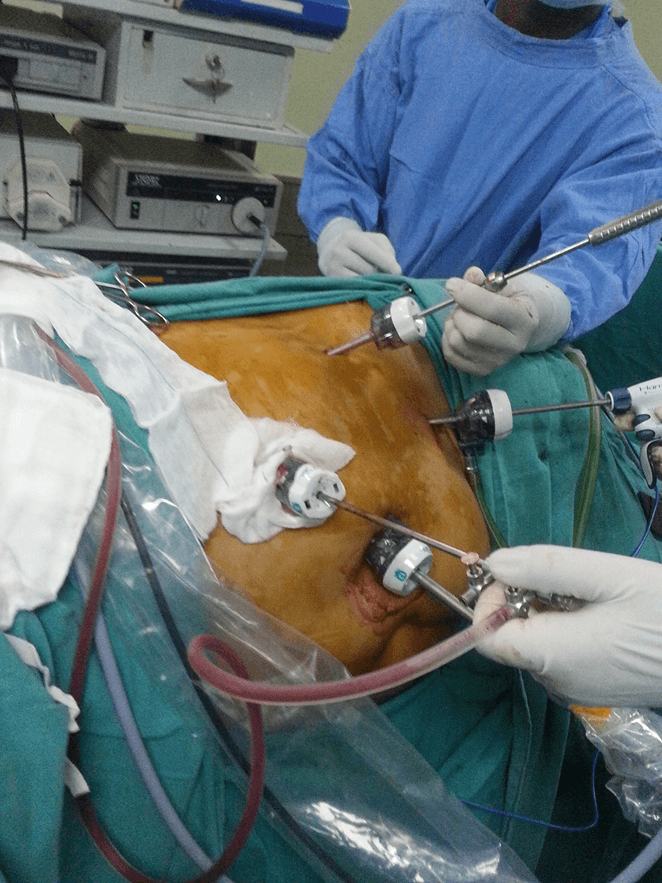
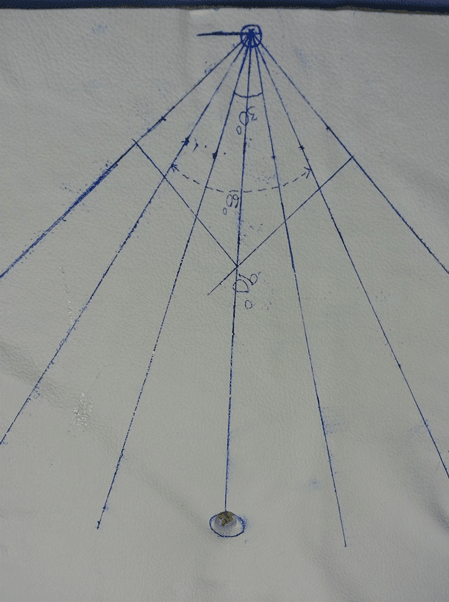
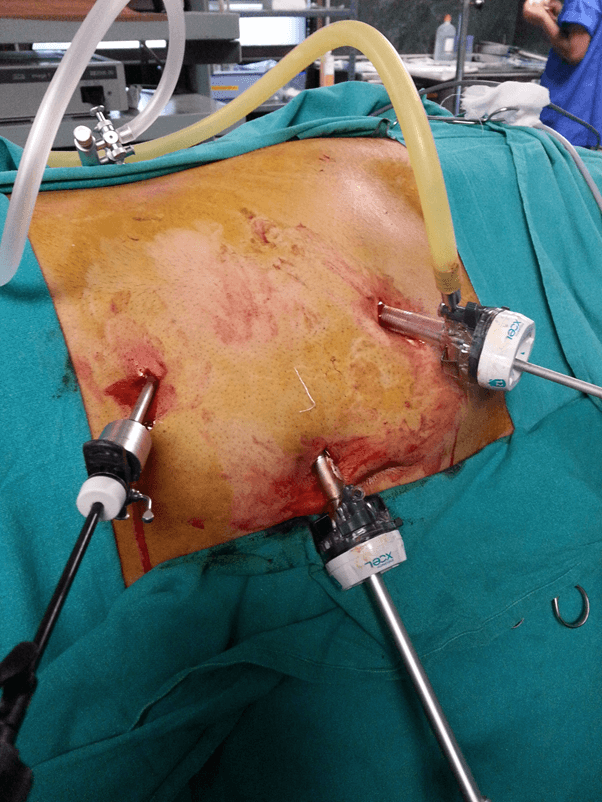
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Dummies.
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Dummies.

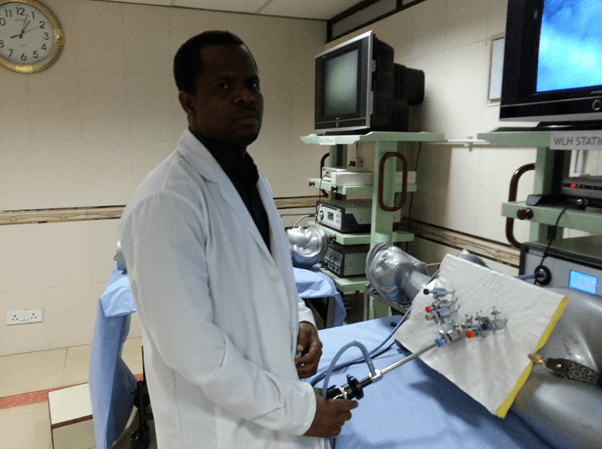
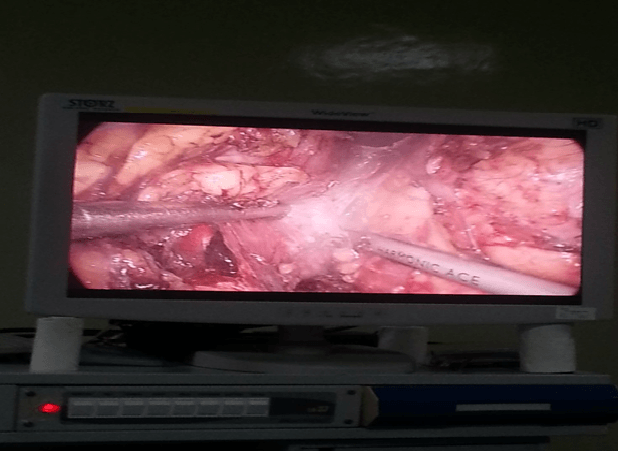
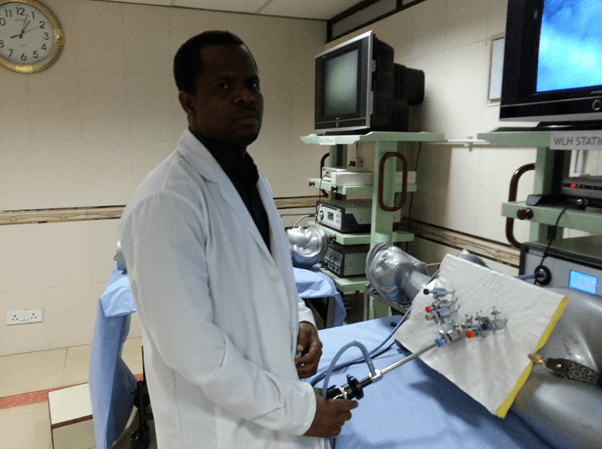
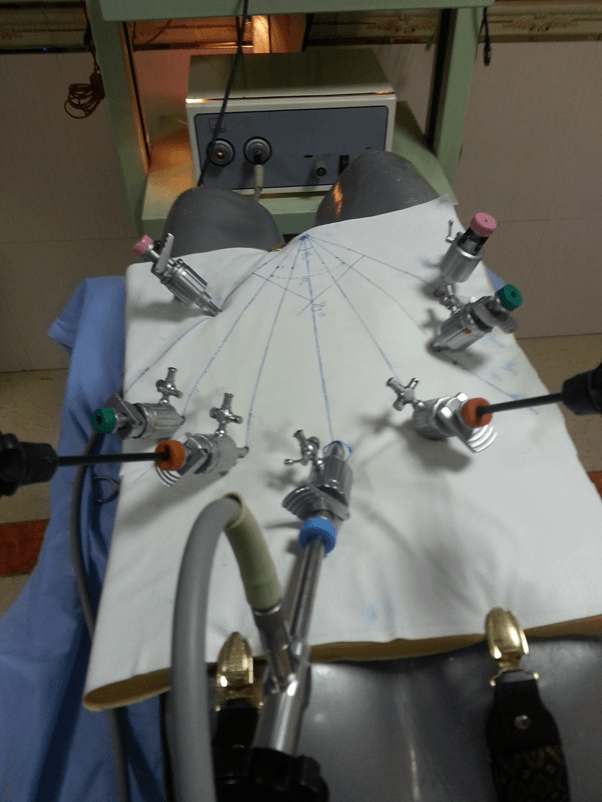
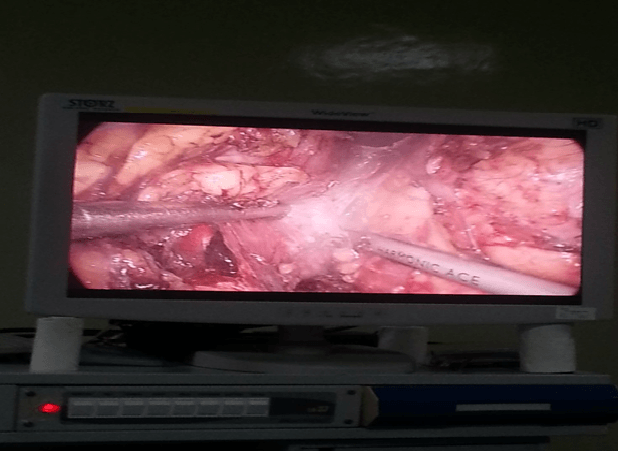
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Swine With Illumination.
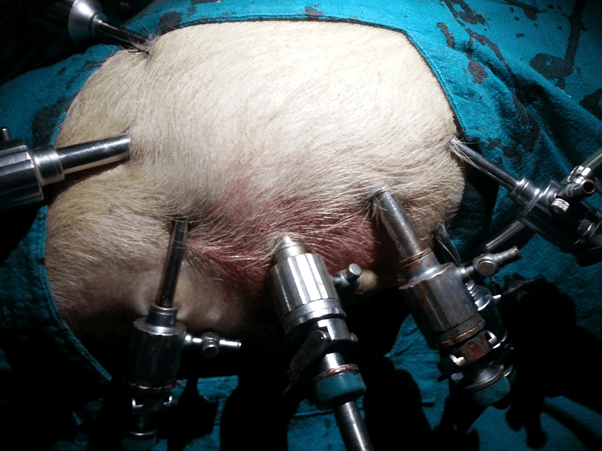
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Swine.
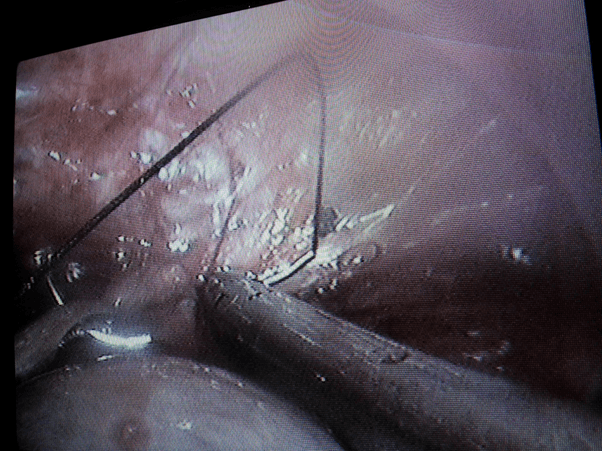
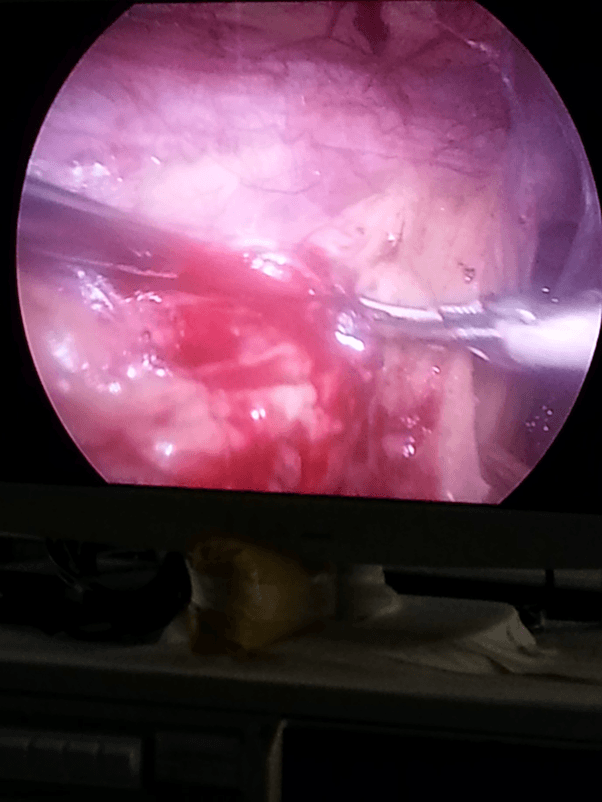
Picture Showing The Approximate Manipulation Angle While Knotting In The Upper Tract In A Swine.
Tying A Knot Around A Fixed Distance To Ensure The Manipulation Angle Is Maintained.
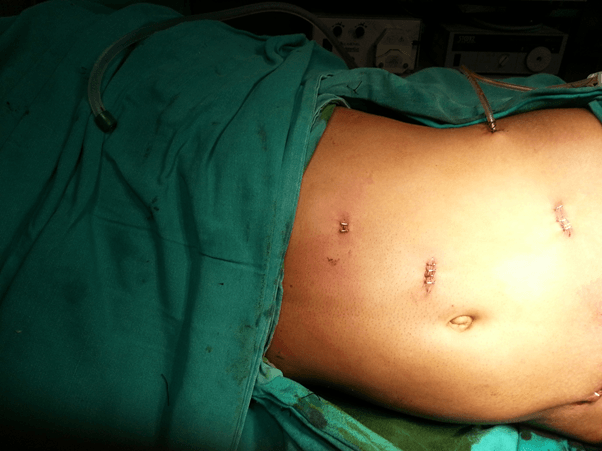
Arrangement Of Ports Positions For Tasks In The Pelvis.
Discription Of Ports Sites On The Anterior Abdominal Wall.
A Picture Of Ring Transfer In The Pelvis At 60 Degree Manipulation Angle.

Performing A Task With 90 Degree Manipulation Angle In The Pelvis.
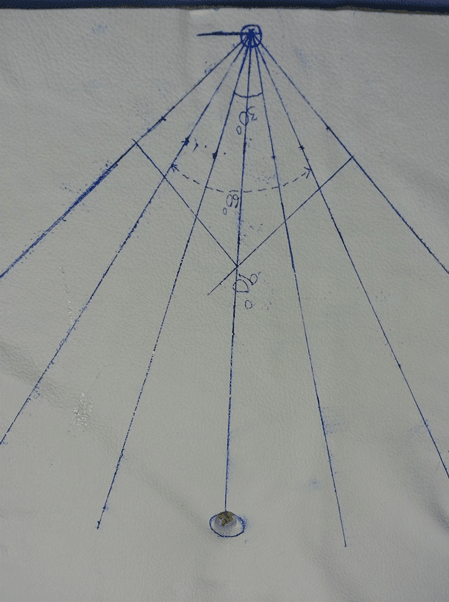
Estimation Of Manipulation Angles Determining Ports Positions On The Dry Lab Anterior Abdominal Wall.
Showing Instruments And Ports At Different Positions Of Task Performance.
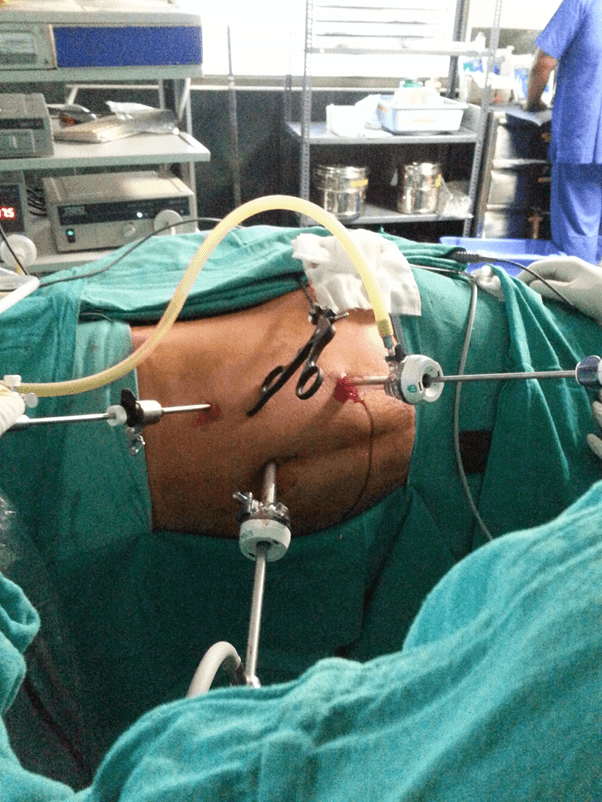
Picture Showing The Working Angle At One Of The Ports Positions In A Donor Nephrectomy.
Port Positions For Left Laparoscopic Donor Nephrectomy.
Ports Positions
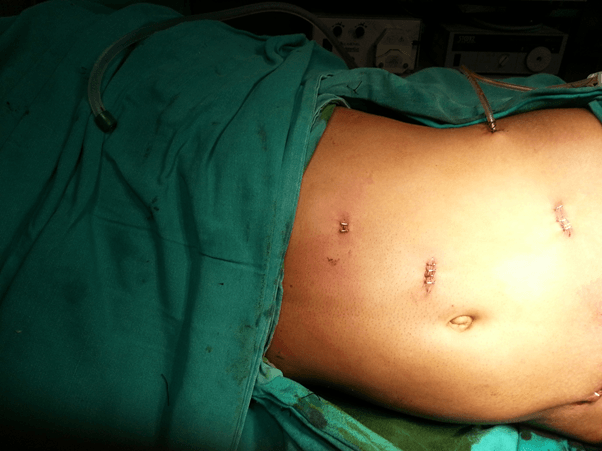
Sites Of Ports Positions After Left Donor Nephrectomy.
Picture Of Manipulation Angle.
Port Positions.
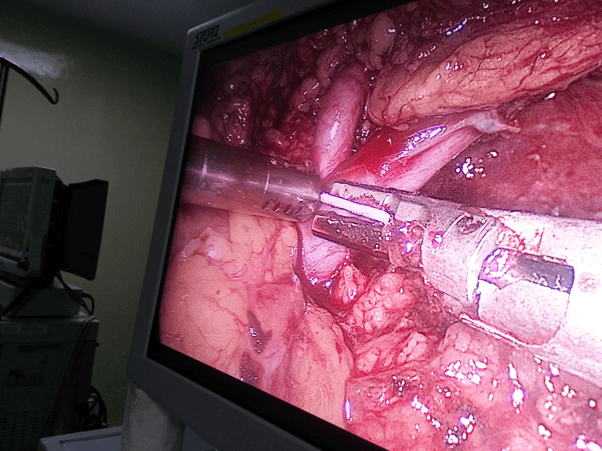
Manipulation angle at the hilum ( crutial target of dissection ).
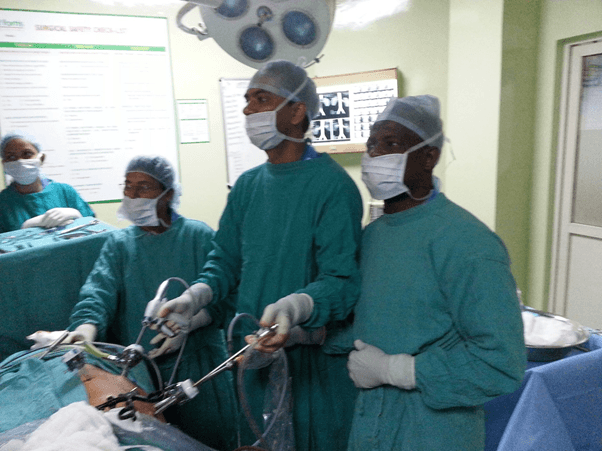
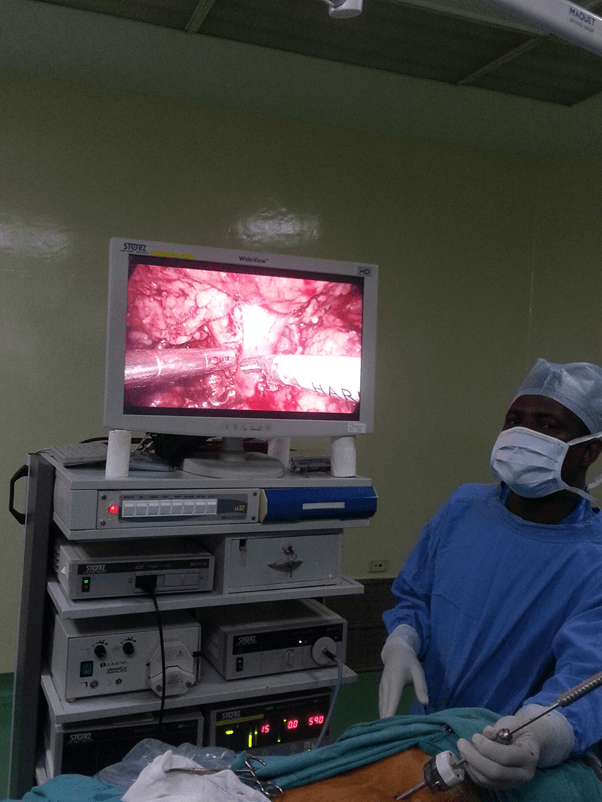
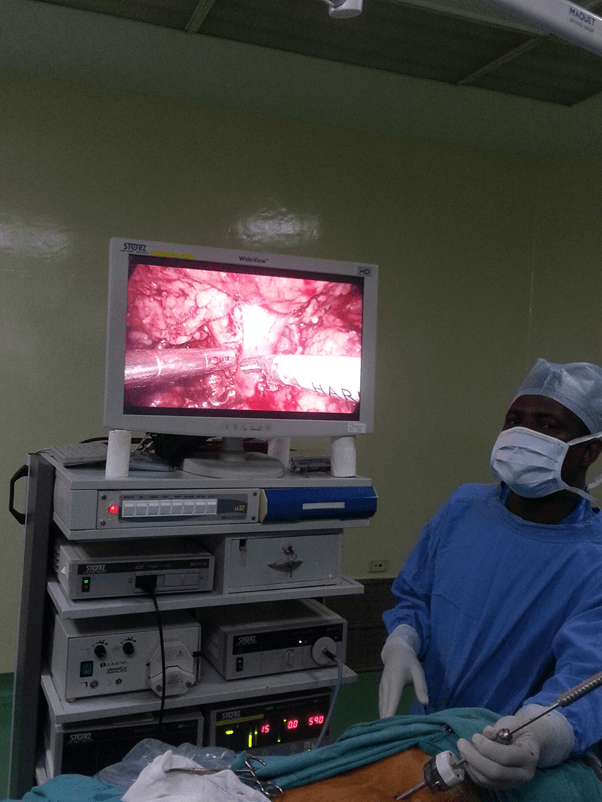
Laparoscopic Surgical Team of the Investigator.
Study Area.
The study was conducted world Laparoscopy Hosptital, Gurgaon. An accredited centre by The Global Open University of Nagaland, to train to masters and PhD in minimal access surgery. World Laparoscopy Hospital is the premier institute of Minimal Access Surgery. It was established to ensure the highest standard of training, treatment and research in laparoscopic and robotic surgery. It's been 12 years since World Laparoscopy Hospital is center of excellence for training in laparoscopic surgery. Laparoscopic Courses of World Laparoscopy Hospital are university recognized and is recognized by World Association of Laparoscopic Surgeons. Courses are internationally accredited by International Accreditation Organization, USA. Robotic Surgery Training is recognized by International College of Robotic Surgeons and endorsed by Intuitive Surgical incorporation da Vinci® Surgical System, USA. This institute excel in specialized medical care supported by comprehensive research and education.41
The Global Open University of Nagaland, is a joint public-private partnership venture between the Government of Nagaland and the World Institution Building Programme (WIBP). It is recognized as a State University by the University Grants Commission of India (UGC), the Association of Indian Universities (AIU) International Association of Educators for World Peace, to confer degrees as on par with the degrees conferred by its members. The Global Open University offers academic degree programmes at both undergraduate and postgraduate levels in many desciplines.42
Sample Size Determination/ Sampling Technique
Conventional sampling was used and 20 chosen based on the previous records of average number of Diploma students.
Study Population
The subjects were recruited as for routine laboratory work. Consecutive selection was done until the sample size was achieved.
Ethical Consideration
All ethical issues binding on the laboratory and research on animal subjects were respected.
Limitations Of The Study.
1. It was difficult to perform each urological procedure, as such regional representation were chosen.
2. The sizes of the animals were small, for which we could not demonstrate port placement for 90 degree manipulation angles in the wet lab, rather only dry lab was used for the lower tract representation.
3. Less number procedures on the lower urinary tract are performed laparoscopically in our centre, as such we could not have human timing representation as we did for the donor nephrectomy.
Conflicts Of Interest
No conflict of interest declared, neither any instrument name was mentioned
Results And Discussions
TABLE 1 A: Timing for surgeon‘s knot in upper urinary track with manipulation angle 30 0.
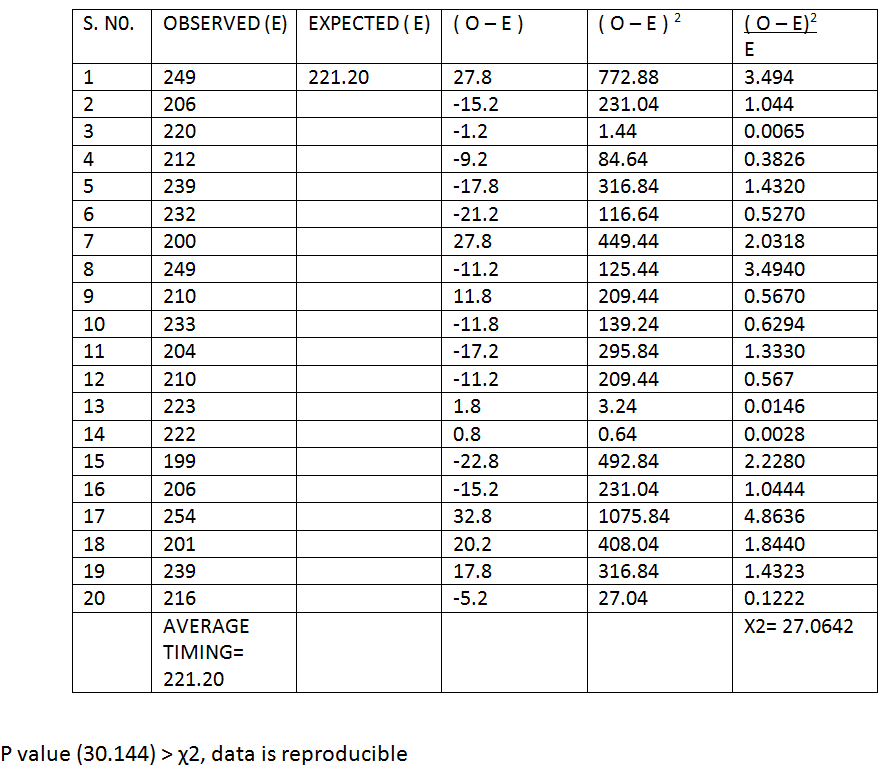
TABLE 1 B: Timing for surgeon‘s knot in upper urinary track with manipulation angle 600.
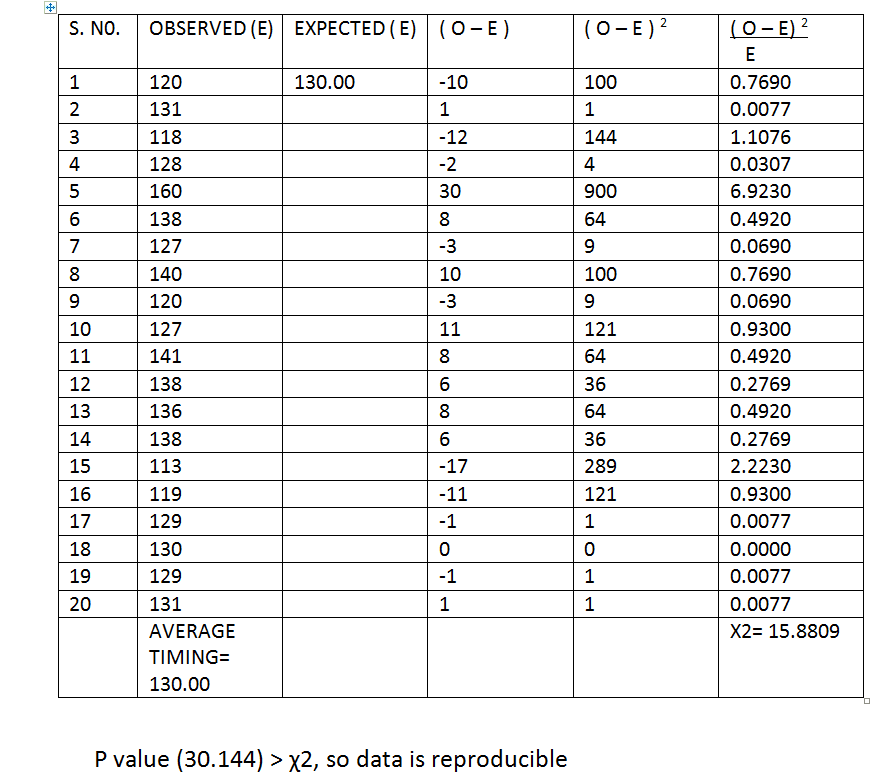
TABLE 1 C: Timing for surgeon‘s knot in upper urinary track with manipulation angle 90 0.
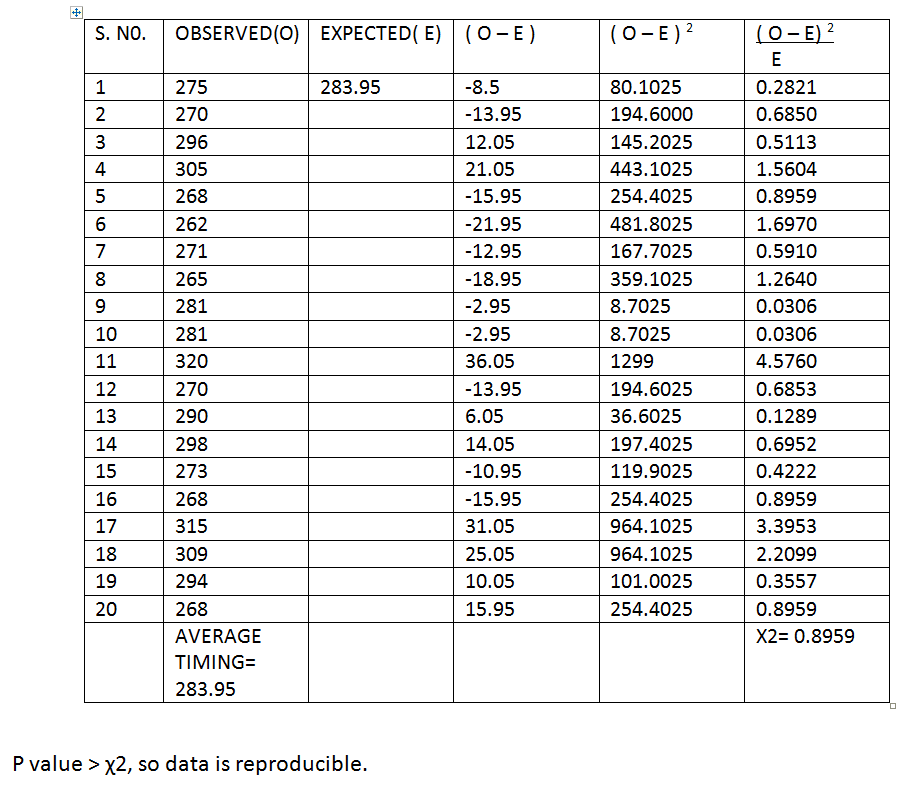
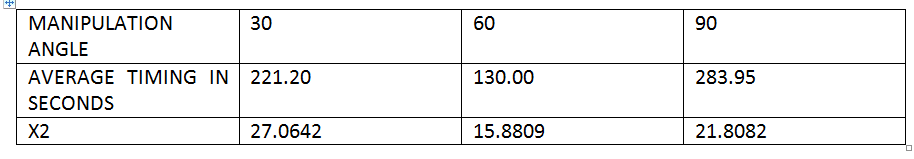
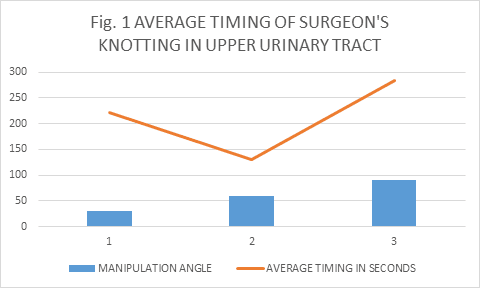
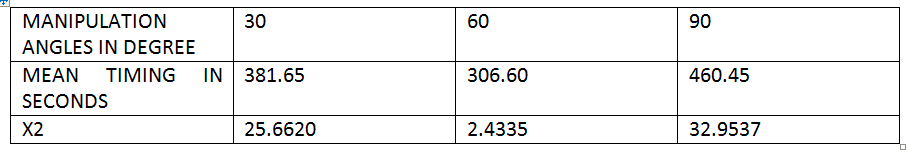
TABLE 1: Average timing of surgeon’s knotting in the region of the upper urinary tract with respective manipulation.
Discussion 1
Tables 1A, B and C showed readings of timing obtained while making a surgeon’s knot in the region of upper urinary tract in the dummy at different manipulation angles which were validated by χ2 tests and average obtained. The averge timing in seconds for 30, 60 and 90 degrees were 221.20, 130.00 and 283,95 respectively. Although all the readings were reproducible at P value( 30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees.
This is shown on figure 1.
TABLE 2A: Timing of clipping of renal vessels at 30 degree manipulation angle.
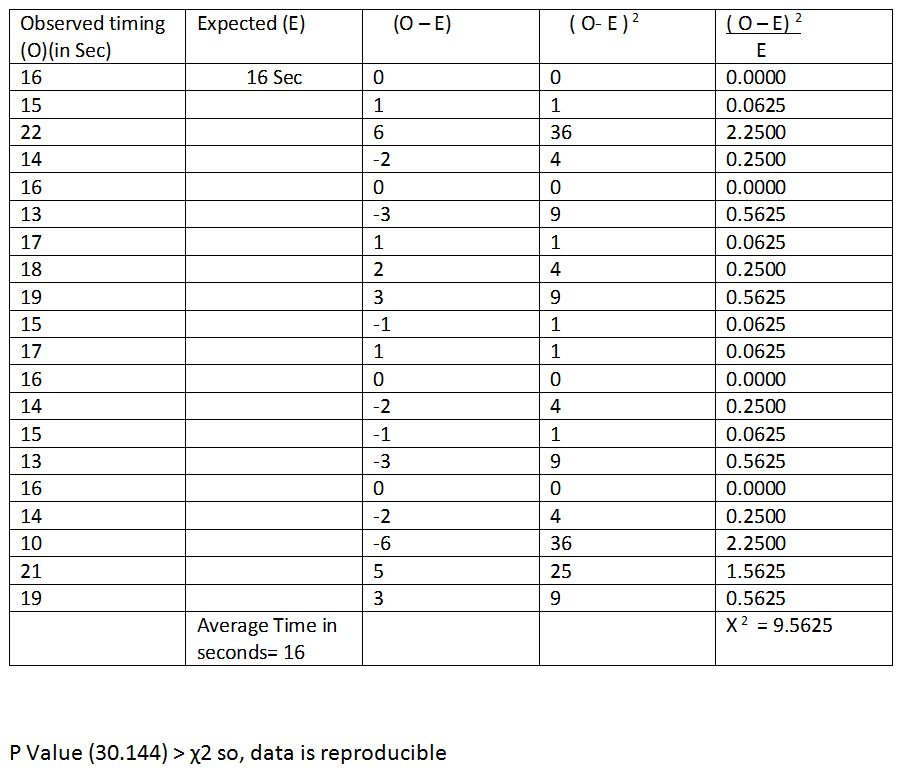
TABLE 2B: Timing of renal vessels clipping with manipulation angle of 60 degree.

TABLE 2c: Timing for renal vessel ligation with manipulation angle 90 0 .
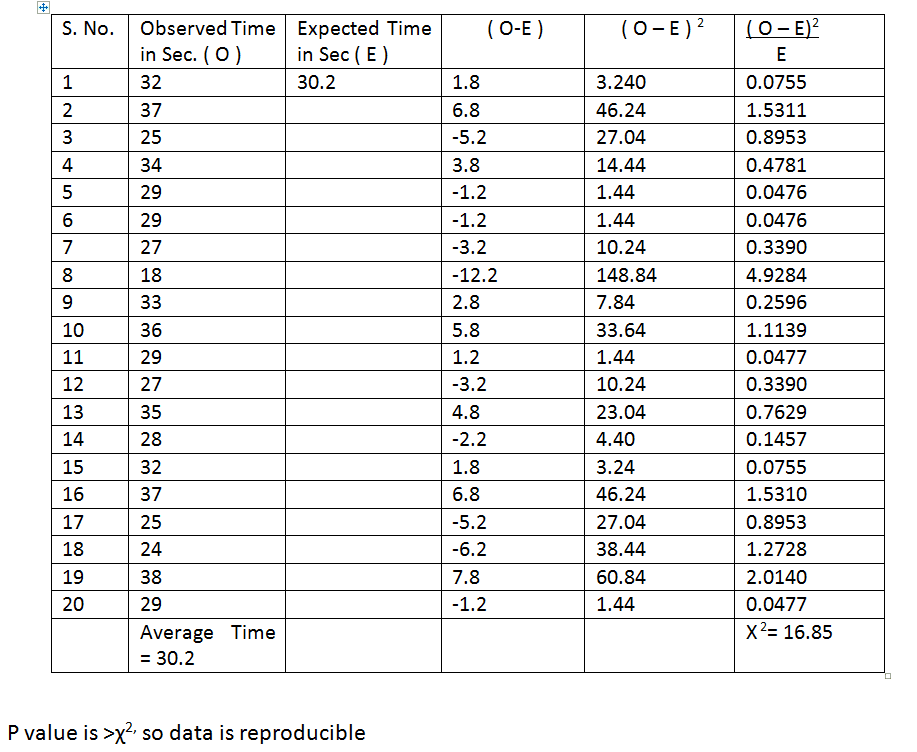
TABLE 2: Average timing of renal vessels clipping.
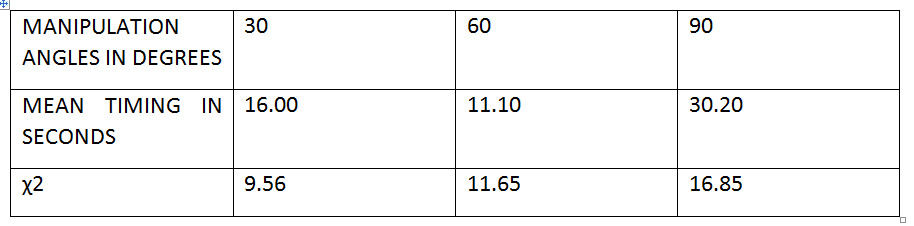
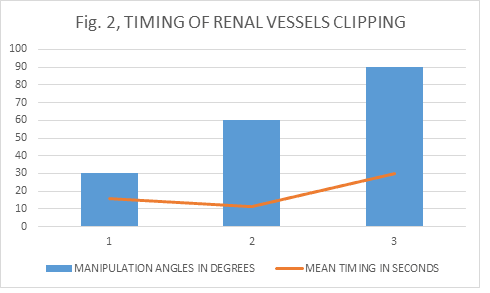
Discussion 2
Tables 2A, B and C showed readings of timing taken to clip a renal vessel in the swine at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 16.00, 11.10 and 30.20 respectively. Although all the readings were reproducible at P value (30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees, and the angle 60 followed by 30 were more reproducible than 90 degrees.
This is shown on figure 2.
TABLE 3A: Timing of ligation of uretero- ureteric anastomosis with 30 degree manipulation angle.
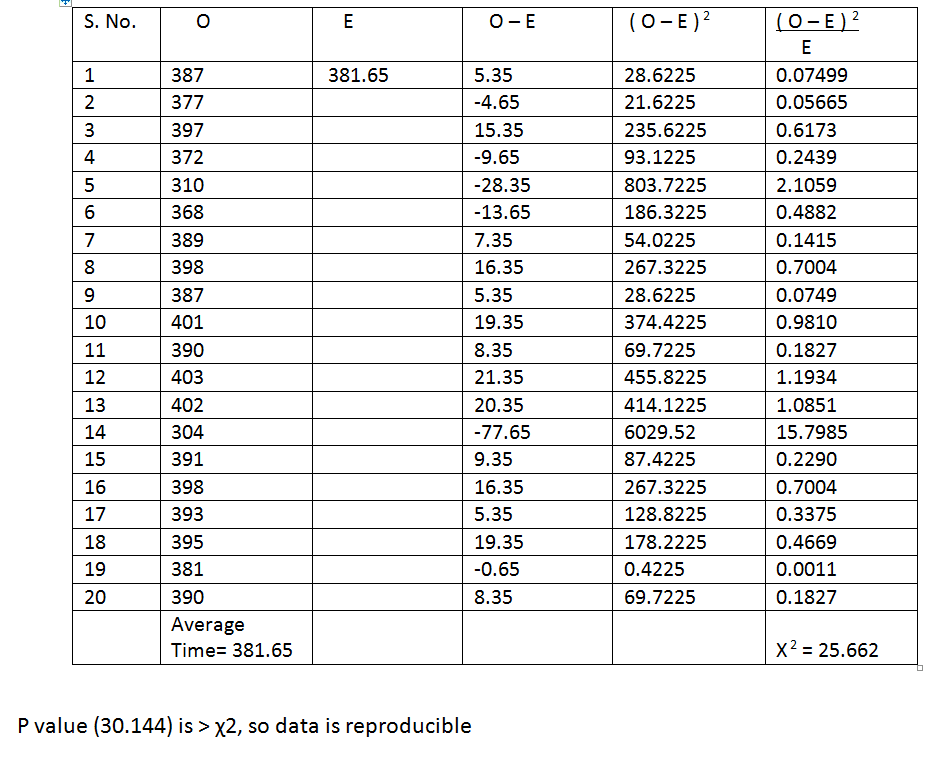
TABLE 3B: Uretro-ureteric anastamosis with manipulation angle 60 0.
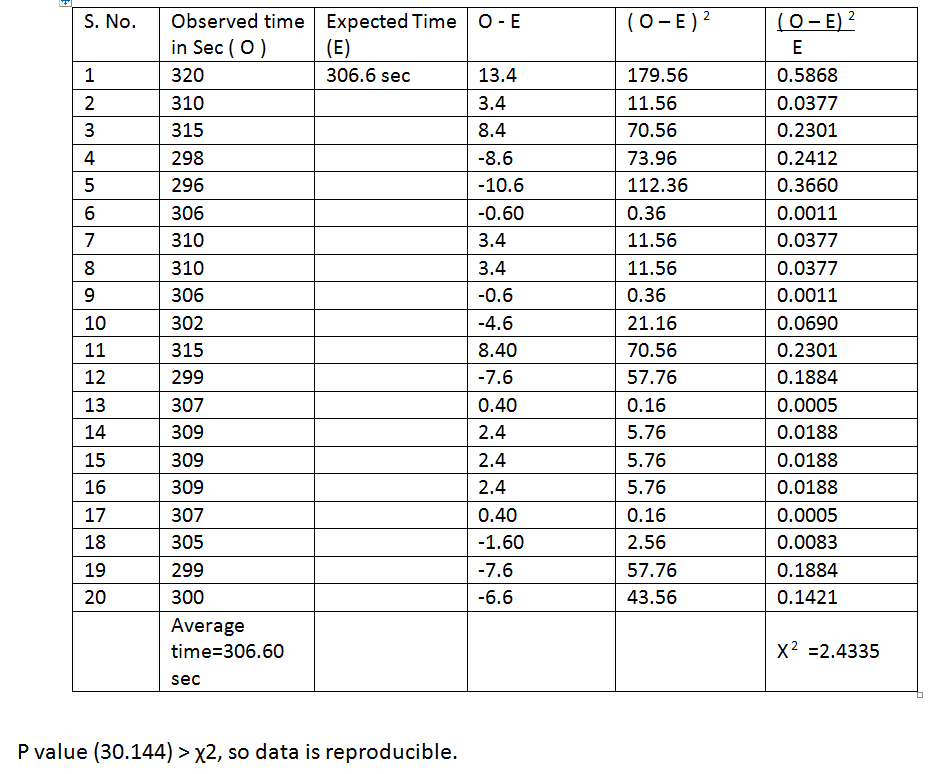
TABLE 4C: Timing for uretero-ureteric anastamosis at manipulation angle 90 0.
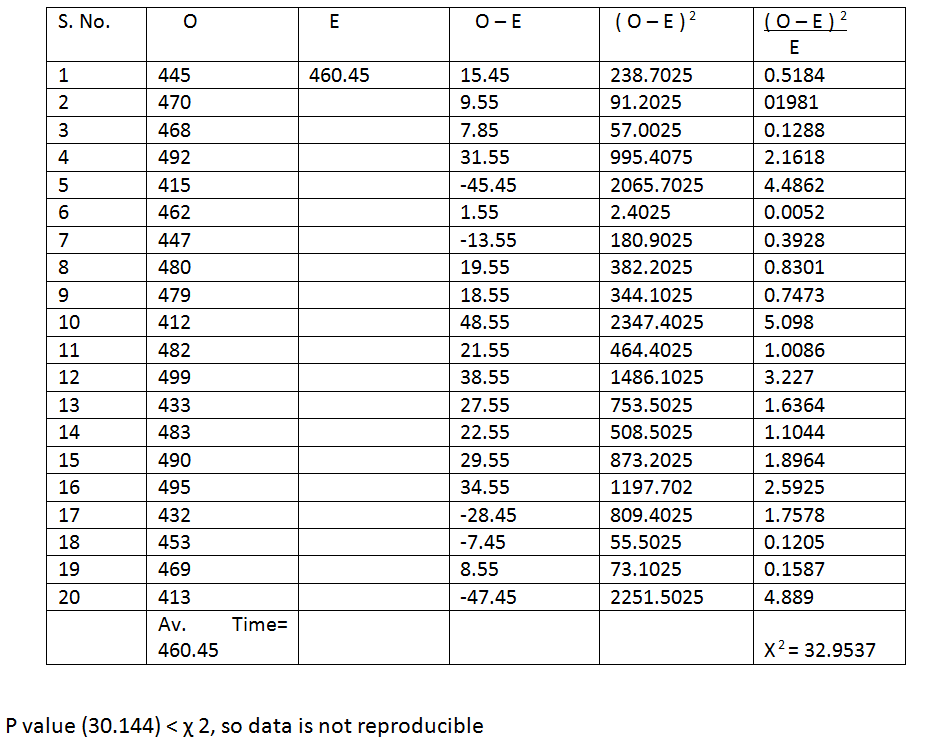
TABLE 4: Average Timing For Uretero-Ureteric Anastomosis.
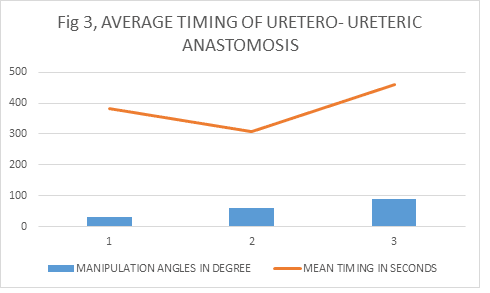
Discussion 3
Tables 3A, B and C showed readings of timing taken for uretero-ureteric anastomosis in the swine at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 381.65, 306.60 and 460.45 respectively. Only readings at 30 and 60 degrees were reproducible at P value (30.144), 5% level of significance; but the χ2 of readings at 90 was less than P value, indicating non reproducibility. These suggest that the 60 degree angle has shorter operative time then the 30; and also demonstrated that the more difficult a laparoscopic task is , is more likely it become non reproducible at an angle of 90 degrees and above, probably due to fatique from high elevation angle and shoulder over stretching due to poor ergonomics. 43
This is shown on figure 3.
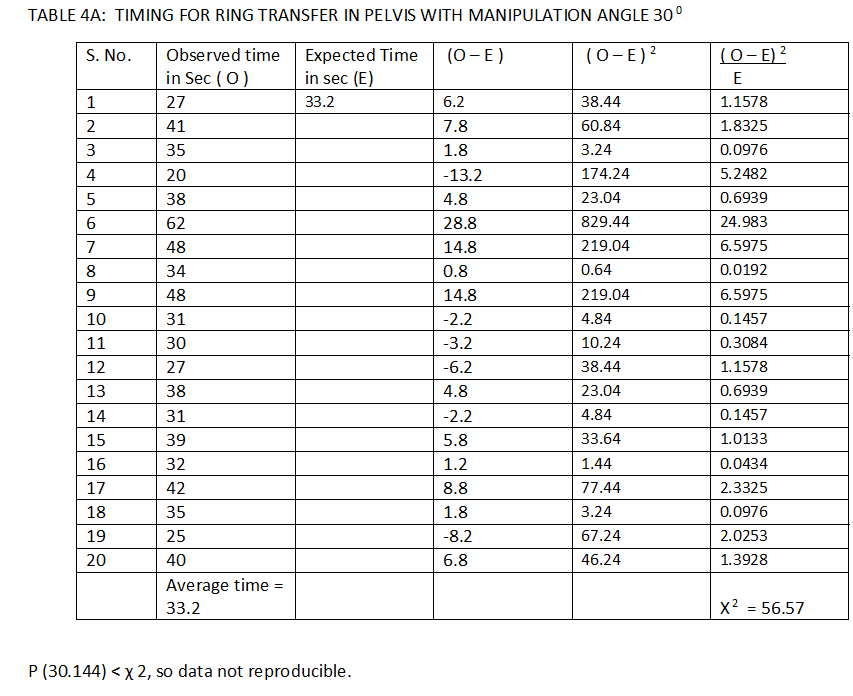
TABLE 4B: Time for ring transfer in pelvis with manipulation angle 60 0.
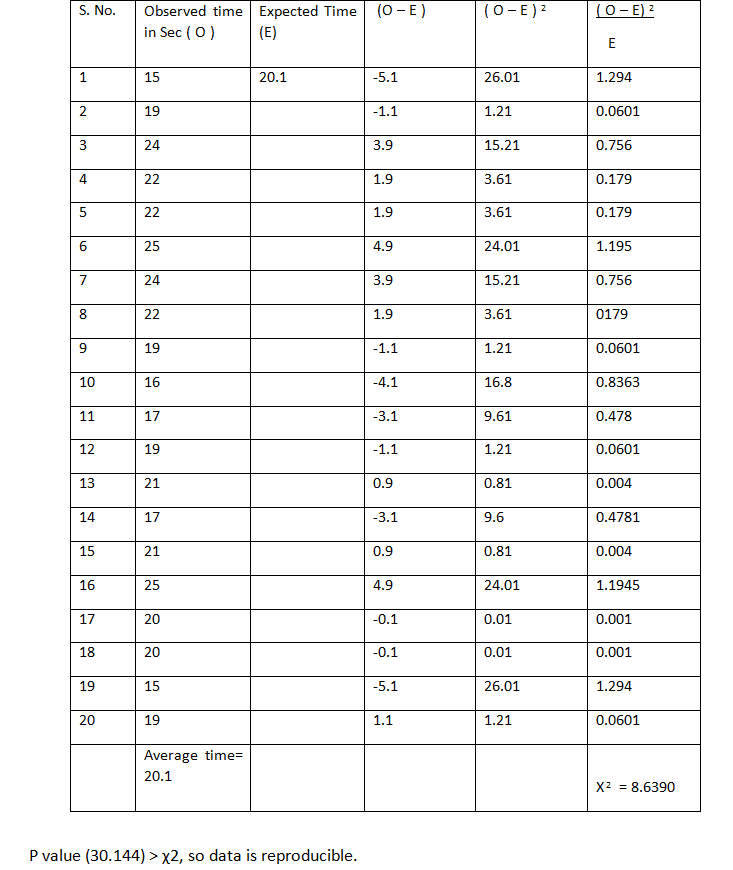
TABLE 4C: Timing for ring transfer in pelvis with manipulation angle 90 0.
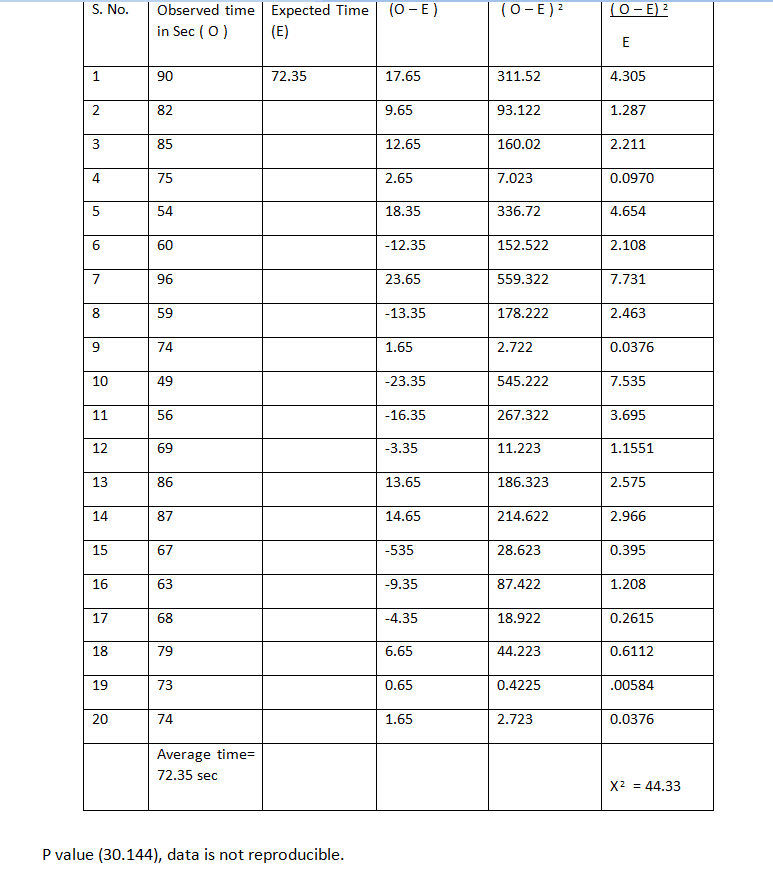
TABLE 4: Averge Timing Of Ring Transfer In The Pelvis
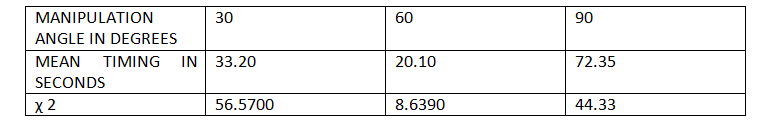
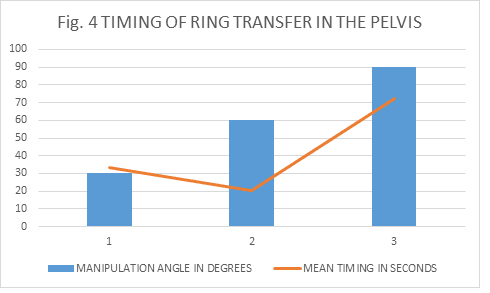
Discussion 4
Tables 4A, B and C showed readings of timing taken for ring transfer in the pelvic region of the dummies at different manipulation angles, which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 33.20, 20.10 and 72.35 respectively. Here only the readings at 60 degree manipulation angle were reproducible at P value (30.144), 5% level of significance: which further support any port position that will provide working angle of 6o degree as the ideal.
This is shown on figure 4.
TABLE 5A: time for surgeon’s knot in pelvis with manipulation angle 30 0.
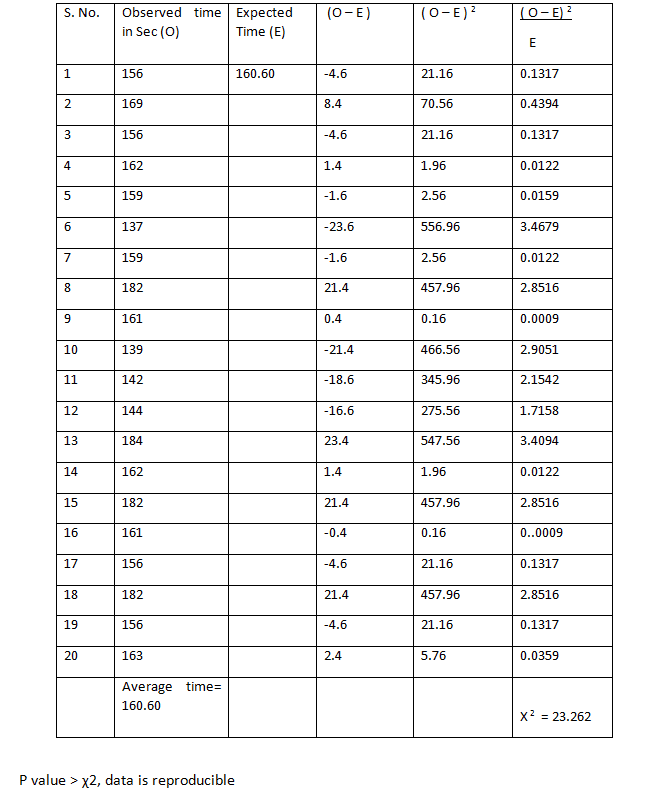
TABLE 5B: time for surgeon’s knotting in pelvis with manipulation angle 60 0.
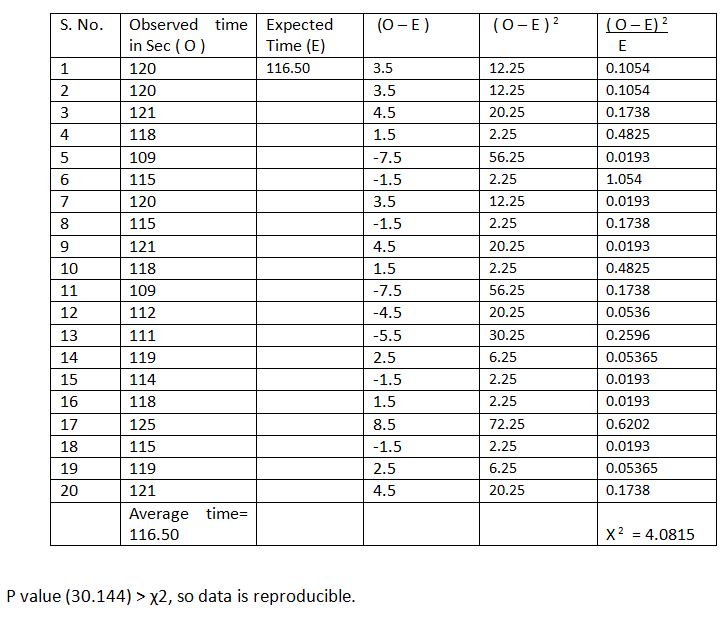
TABLE 5C: Time for surgeon’s knotting in pelvis with manipulation angle 90 0.
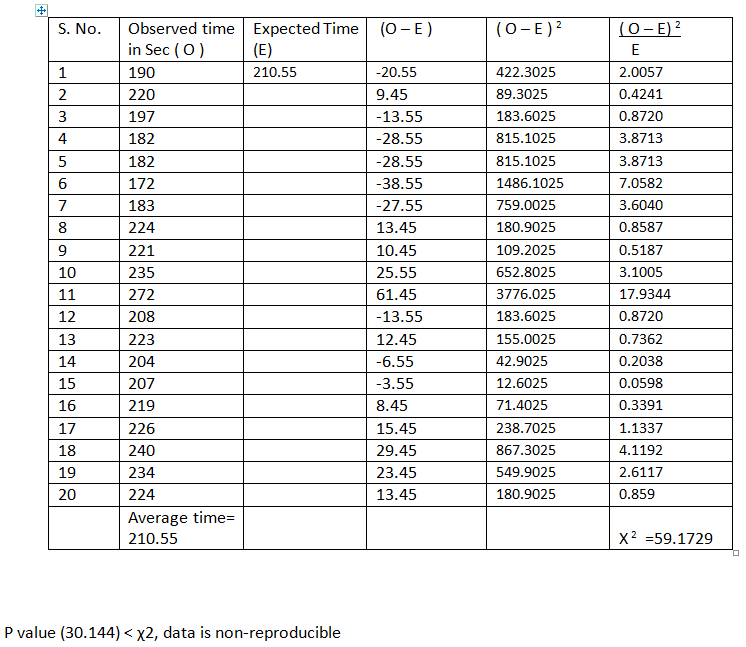
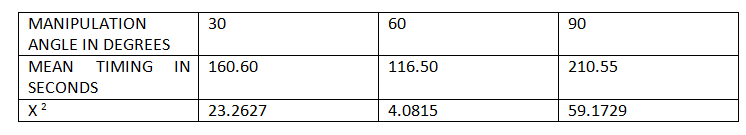
TABLE 5: Average Timing For Surgeon’s Knotting In The Pelvis.
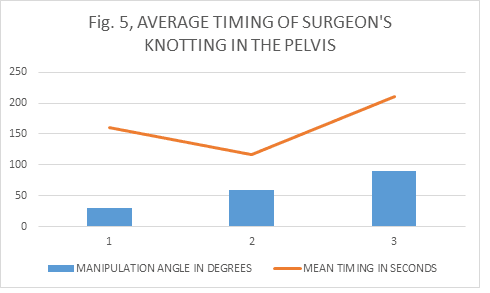
Discussion 5
Tables 5A, B and C showed readings of timing of surgeon’s knotting in the pelvic cavity of dummies at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 160.60, 116.50 and 210.55 respectively. Despite the facts that, the first two readings were reproducible at P value (30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time than that of 30 degrees. The readings of 90 degree angle were non reproducible for surgeons knotting in the pelvis indicating increased difficulties and time consumption when ports are positioned in such a way that will give working angle of 90 degrees and above.
This is shown on figure 5.
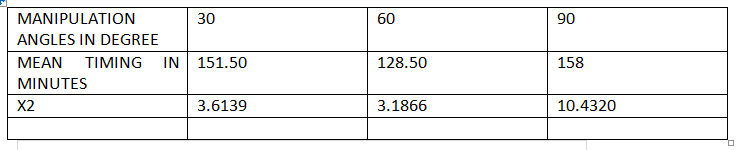
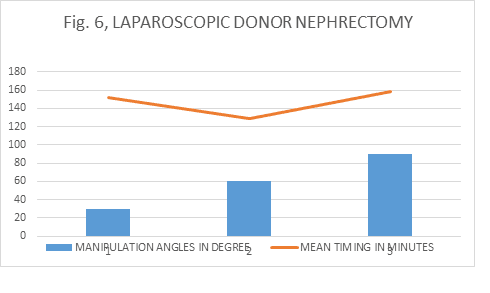
Laparoscopic Donour Nephrectomy
TABLE 6A: Timing of laparoscopic donour nephrectomy with approximate 30 degree manipulation angle.
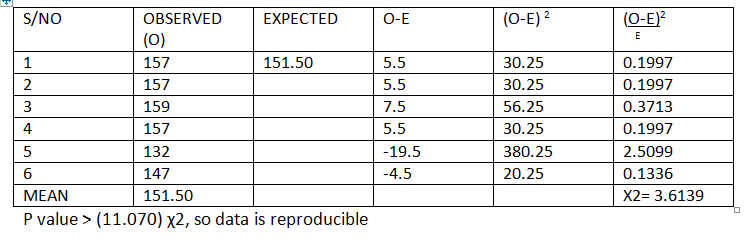
TABLE 6B: Timing of laparoscopic donor nephrectomy with approximate 30 degree manipulation angle.
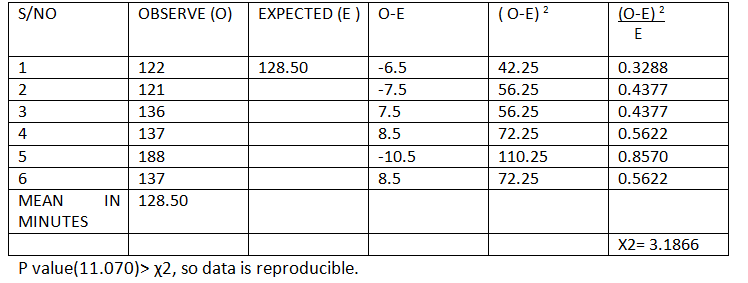
TABLE 6C: Approximate manipulation angle of 90 degrees and timing of donour nephrectomy in minutes.
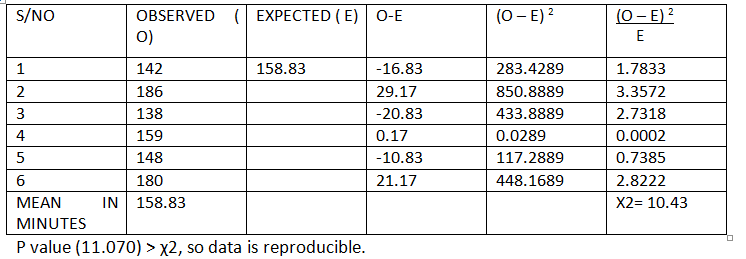
TABLE 6: Average duration of laparoscopic donor nephrectomy in minutes.
Discussion 6
Tables 6A, B and C showed readings of timing taken for laparoscopic donor nephrectomy and manipulation angles were approximated nearest to 30, 60 and 90 degrees. The readings obtained in minutes were validated by χ2 tests and average obtained. The averages were 151.50, 128.50 and 158.83 respectively. Although all the readings were reproducible at P value (11.070), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees, and the angle 60 followed by 30 were more reproducible than 90 degrees.
This is shown on figure 6.
Overall Discussion, Conclusion And Recommendations
5.1 Discusion
From all the discussions above, the average timing of all laparoscopic tasks were shorter with 60 degree manipulation and all were reproducible irrespective of the difficulty of the tasks then followed by 30 degree. The 90 degree angle has the longest operative time, and in some cases non reproducible, indication the closer the manipulation angle is to the 90 degrees and above, the more the likely to take longer operative time and the higher it approaches non reproducibility due to fatigue from increased elevation angle and shoulder overstretching. This is in keeping with the Baseball Diamond concepts of port positioning.
Conclusion
There is no “Ideal port position in urological laparoscopic procedures based on anatomical land marks, but the closer the ports positions are to make a manipulation angle of 60 degrees (Base Ball Diamond), the closer to ideal it will be.
Recommmendations
More work is to be done on the newly emerging laparoscopic urology particularly in the developing world.
References
1. Supe AN, Kulkarni GV, Supe PA. Ergonomics in laparoscopic surgery. J Min Access Surg 2010;6: 31-36.
2. Karthik S, Augustine AJ, Shibumon MM, Pai MV. Analysis of laparoscopic port site complications. A descriptive study. J Min Access surg 2013;9:59-64 .
3. Greberg CF, Gettman MT. Instrumentation for natural orifice transluminal endoscopic surgery and laparoendoscopic single-site surgery. Indian J urol 2010;26:385-8 .
4. Gupta NP, Gautam G. Laparoscopic nephrectomy for benign non-functioning kidneys. J Min Access Surg 2005; 149-54.
5. Maurya K, Sivanandam SE, Sukumar S, Bhat S, Kumar G, Nair B. Concomitant laparoscopic urological procedures: Does it contribute to morbidity? J Min Access Surg 2009; 5:67-71.
6 WORLD LAPAROSCOPY HOSPITAL. Cyberciti, DLF Phase II, NCR Delhi, Gurgaon, 122 002, India. Port position In Laparoscopy.
7. Gupta N, Raina P, Kumar A. Laparoscopic donor nephrectomy. J Min Access Surg 2005; 155-64.
8. McDougall EM, Finley D, Clayman RV et al. Basic urologic laparoscopy: A Standardized Guideline for Training Programs.American Urological Association Education and Research.2005; 20-25
9. Veenstra GM, Fossion LMCL, de Laet K, Luijten AAPM. Synchronous laparoscopic radical nephrectomy left and contralateral right hemicolectomy during the same endoscopic procedure. J Laparoendosc Adv Surg Tech 2004;
10 Chung BI, Liao JC. Laparoscopic radical nephrectomy in a pelvic ectopic kidney: Keys to success. JSLS. 2010; 14: 126–129.
11 Ganpule AP, Sharma R, Thimmegawda M, Veeramani M, Desai MR. Laparoscopic radical nephrectomy versus open radical nephrectomy in T1-T3 renal tumours. An outcome analysis. Indian J Urol 2008; 24:39-43
12 Rais-Bahrami S, Waingankar N, Richstone L. Upper tract urologic laparoEndoscopic single site surgery. Indian J Urol2012; 28:60-4
13 Kopp RP, Silbestin JL, Derweesh I. Laparoendoscopic single site radical nephrectomy with renal vein thrombectomy: Initial report. BMC Urology 2010; 8:10
14 Raman JD,Cadeddu JA.Single access Laparoscopic nephrectomy. Indian J Urol2008; 24:457-460
15 Greberg CF,Gettman MT. Instrumentation for natural orifice transluminal endoscopic surgery and laparoendoscopic single site surgery. Indian J Urol 2010; 26:385-8
16. Thiel DD. Navigating the difficult robotic assisted pyeloplasty. ISRN Urol 2012; 2:34
17. Singh O, Gupta SS, Hastir A, Arvind NK. Laparoscopic transperitoneal pyelopyelostomy and ureteroureterostomy of retrocaval ureter: Report of two cases and review of the literature. Journal of Minimal Access Surgery.Vol.2010; 6:53-55
18 Faddegon S,Tan YK, Olweny EO, Park SK, Sara L. Best BS, Cadeddu JA. Laparoendoscopic single-site (LESS) Pyeloplasty for horseshoe ureteropelvic junction obstruction. JSLS. 2012; 16:151–154.
19. Bansal P, Gupta A, Mongha R, Narayan S, Kundu AK, Chakraborty SC, et al. Laparoscopic versus open pyeloplasty: Comparison of the two surgical approaches- A single centre experience of three years. J Min Access Surg 2008; 3:76-9
20 Mellon MJ, Sethi A, Sundaram CP. Laparoscopic adrenalectomy: Surgical techniques. Indian J Urol 2008; 24:583-589
21 Kumar S, Bera MK, Vijay MK, Dutt A, Tiwari P, Kundu AK. Laparoscopic adrenalectomy: A single center experience. J Min Access Surg 2010; 6:100-105
22 : Dalvi AN, Thapar PM , Kumar KV, Kamble RS, Rege SA, Deshpande AA, Shah NS, Menon PS. Laparoscopic adrenalectomy: Gaining experience by graded approach. J Min Access Surg 2006; 2:59-66.
23 Sasaki et al. Laparoscopic single site adrenalectomy: Initial results of cosmetic satisfaction and the potential for post-operative pain reduction. BMC Urology 2013; 13:21
24 Nagraj HK, Kishore TA, Nagalakshmi S. Transperitoneal laparoscopic approach for retrocaval ureter. J Min Access Surg 2006; 2:81-2
25 Agrawal V, Bajaj J, Acharya H, Chanchalani R, Raina VK, Sharma D. Laparoscopic management of pediatric renal and ureteric stone. J P Urol 2013; 9:230-233
26 Ahlawat RK, Gaulam G. Suprapubic transvesical single-port technique for control of lower end of ureter during laparoscopic nephroureterectomy for upper tract transitional cell carcinoma. Indian J Urol 2011; 27:190-5
27 Cestari A, Buffi NM, Scapaticci E et at. Simplifying patient positioning and port placement during robotic assisted laparoscopic prostatectomy. European Urology 2010; 57:530-533
28. Ashis C, Adnan Q, Aziz A, Edward MD. Optimal port placement during laparoscopic radical prostatectomy. Can J Urol 2012; 19:6142-6146
29 Columbo JR, Santos B,Hafron J, Gianduzzo T, Haber GP, Kaouk JH. Robotic assisted radical prostatectomy: Surgical techniques. Int. Braz. J Urol2007; 33:803-9
30 Pow-Sang JM, Velasquez J, Myers MD, Rodriguez AR, Kang LC. Pure laparoscopic and robotic –assisted laparoscopic radical prostatectomy in the management of prostate cancer. Cancer control 2007; 14:250-7
31 Gerullis H, Kuemniel C, Popken G. Laparoscopic cystectomy with extracorporeal-assisted urinary diversion: Experience with 34 patients. European Urology 2007; 51:193-198
32 Cansino JR, Cisneros J, Aloso S et al. Laparoscopic radical cystectomy: Initial series and analysis of result. European Urology Suppl. 2006; 5:956-961
33 Vordos D, Hoznek A, Gettman M, Abbon CC. Laparoscopic cystectomy: Evolution of a new technique. EAU series 2005; 3:147-155
34 Peterson AC, Lance RS, Ahuja SK. Laparoscopic hand assisted radical cystectomy with ileal conduit urinary diversion. J Urol 2002; 168:2103-2105
35 Chan P. Management options of varicocele. Indian J Urol 2011; 27: 65-73
36 Link BA, Kruska JD, Wong C, Kropp BP. Two trocar laparoscopic varicocelectomy: Approach and outcomes. JSLS 2006; 10: 151–154.
37 Ivovic J. Laparoscopic surgery for varicocele in subfertile men. European Urology Suppl 2009; 8:626-627
38 Capolicchio JP, El-Sherbiny M, Brzezinski A, Eassa W, Jednak R. Dye-assisted lymphatic-sparing laparoscopic varicocelectomy. JPUrol 2013; 9:33-37
39 Moreira-Pinto J, Osorio A, Carvalho F, de Castro JR, de Sousa J, Enes C, Reis A,Cidade-Rodrigues J. Varicocelectomy in adolescents: Laparoscopic versus open high ligation technique. Afr J Paediatr Surg 2011; 8:40-43
40 Nerli RB, Reddy M, Devraju S, Prabha V, Hiremath MB, Jali S. Laparoscopic mitrafanoff appendicovesicostomy: Our experience in children. Indian J Urol 2012; 28: 28-31
41. www.worldlaparoscopyhospital.com/laparoscopic treatment training and research
42. www.globalopenuniversity.org
2.1 Literature Review
2.2 Laparoscopic Nephrectomy And Port Positioning :
There are various approaches to nephrectomy and the placement of ports depends on the approach and the side, and weither or not a single site laparoendoscopic approach is intended.
2.3 Transperitoneal Approach :
In this approach usually a 12–mm port is placed at umbilicus by open Hasson technique, which is often primarily used as a camera port. Another 12–mm laparoscopic port is placed between umbilical port and anterior superior iliac spine (spinoumbilical port) and a 5–mm port is placed in line with the camera port at about 3 cm below the costal margin and 3 cm lateral to the midline. The fourth usually for retraction if needed, is a 5 mm port placed 4 cm below the costal margin in anterior axillary line.7 Both kidneys have similar approach on either side.
Another approach is to place the laparoscopic port on the mid-clavicular line just at or above the upper border of the umbilicus. A working port usually 10/12mm is positioned a finger-breadth below the costal margin on the anterior axillary line. A second working port, is placed on the anterior axillary line just above the superior iliac crest. An additional working port may be placed on the mid-axillary line mid-way between the costal margin and the superior iliac crest to provide access for a retracting instrument and to mobilize the kidney laterally. For the extremely thin patient the port sites are all moved medially with the laparoscope at the umbilicus, the working ports on the mid-clavicular line and an additional port on the anterior axillary line.8
One other approach for the left kidney is to place the camera port at the paraumblical space at the lateral border of the rectus muscle at the level of the umbilicus while the patient is placed in the right lumbotomy position; through the open introduction technique according to Hasson. One additional 10-mm, and one 5-mm trocar are then inserted under laparoscopic vision in the epigastric and mid-clavicular positions.9
The left kidney can also be approached with the camera port placed just to the left of the umbilicus. The left hand 12-mm port placed along the lateral border of the rectus abdominis muscle lateral to the umbilicus. The right hand port placed on the lateral border of the rectus near the dome of the bladder. A fourth port to be placed laterally to retract the sigmoid colon medially.10
2.4 The Retroperitoneal Approach :
In the retroperitoneal laparoscopic approach, incision is made at tip of 12th rib and then blunt dissection or balloon used to create space and the working port is placed between the midaxillary line and the anterior axillary line (5cm above the iliac crest). A 5mm port is then inserted at the junction of the 12th rib and paraspinal muscles (renal angle).11
Another approach through the retroperitoneal space is obtained through a 15-20mm incision just below the tip of the 12th rib and the secondary ports are then placed along the inferior border of the costal margin using digital palpation through the balloon dilated incision site. After digital placement of all the secondary ports, the primary balloon-tip port is inserted. The posterior secondary 12mm port is placed at the lateral border of the paraspinal muscle along the inferior border of the 12th rib. An anterior port is placed near the anterior axillary line, just below the inferior tip of the 11th rib. An additional 5mm port may be placed, on the mid-axillary line at or above the level of the superior iliac crest, and used for retraction and suction. Often a 12 mm port is placed at Petit’s triangle just above the midportion of the iliac crest and a fingerbreadth superior to the iliac crest. 8
2.5 Hand-Assissted Laparoscopic (Hal) Nephrectomy:
The hand-assisted device for right renal surgery could be located at and just below the umbilicus on the midline. Alternatively, on the right side the hand port may be placed as a Gibson incision in the right lower quadrant. A port is placed on the mid-clavicular line just above the superior iliac crest; the laparoscope is positioned at this port site. A 12mm port is placed two finger breadths below the costal margin on the mid-clavicular line, to accommodate the EndoGIA stapling device. A 5mm port is placed on the mid-line in the epigastric region for placement of an instrument to retract the liver superiorly and medially.8
Conversely, on the left the incision for the HAL device is located on the midline, at and above the umbilicus on the mid- clavicular line just above the superior iliac crest, a 10mm port placed for positioning of the 10mm, 30 degree laparoscope. The laparoscope may then be used for visualization of the HAL device incision. An additional 12mm working port is placed on the mid-clavicular line 2 finger breadths below the costal margin. Retraction of the kidney laterally may be facilitated by an instrument placed through a 5mm port in the mid-axillary line, mid-way between the costal margin and superior iliac crest.8
2.6 Laparoendoscopic Single Site (Less) Nephrectomy) :
Since the advent of laparoscopy, urologist have tried to minimize scars and improve cosmesis, leading to the progression to laparoendoscopic single site urological procedure. Access is usually gain through the umbilicus, but others include trans abdominal or retroperitoneal flank approach, a suprapubic or mini pfannesteil approach or Gibson incisions.12
Either a specialised port or cluster conventional port can be used to obtain access. Conventional laparoscopic techniques are generally followed, although modifications in techniques and manoeuvres unique to single site surgeries are employed.12
During LESS nephrectomy, a peri- umbilical incision is made to the rectus fascia. The peritoneum is entered with an extra-long trocar. After pneumoperitoneum, another trocar, is placed 1-1.5 cm caudal and at the 4 o'clock position to the extra-long trocar, eventually functioning as the camera port. A 12 mm port is inserted 1.5 cm caudal to the second trocar, resulting in triangular configuration. A fourth 12 mm standard length trocar is placed 1 cm cephalad to the umbilical protuberance, through which liver or splenic retraction and control of the renal upper pole and adrenal gland is achieved.13
2.7 Natural Orifice Transluminal Endoscopic Nephrectomy :
Natural orifice trans luminal endoscopic surgery (NOTES), with the objective of incision free abdominal surgery through natural orifices, (mouth, vagina and rectum) has been described. Although there were reports on successful completion of six laparoscopic transvaginal nephrectomies using conventional instruments in a porcine model, there were note of limitations of the laparoscopic instruments making the procedure cumbersome and time consuming. Clayman and colleagues reported their experience with single port NOTES transvaginal nephrectomy and encountered similar difficulty until a purpose built multi lumen operating instruments were made available.14
Hybrid NOTES in which two natural orifices are used for approaches has also been described and tried for nephrectomies. Transvaginal NOTES hybrid combined with either trans gastric or trans vesical nephrectomy, transvesical –trans gastric have all been described.15
2.8 Laparoscopic Pyeloplasty :
Standard port placement described as ports placed in the upper and lower quadrant midclavicular lines and the camera port placed near the umbilicus. An assistant port is placed in the suprapubic midline.16
Another approach with a primary port at 2.5 cm to the right of umbilicus, a 5 mm port midway between the primary port and right costal margin, and on right mid-clavicular line, and another 5 mm port midway between the antero-superior iliac spine and the umbilicus was used while the patient was placed in the 45 left lateral position. Fourth flank port is placed for retraction.17
2.9 Less Pyeloplasty :
The patient is positioned in a modified flank fashion, and a 2.5-cm incision is made within the umbilical dimple to conceal the scar. After insufflation of the abdomen, three 5-mm trocars are placed through the anterior abdominal fascia in a triangular configuration. A 5-mm 45-degree laparoscope is used along with articulating laparoscopic instruments. The laparoscope is placed through the most medial trocar and positioned anteriorly in the abdomen so that the camera looks down onto the surgical field. The working instruments are placed through the 2 lateral trocar.18
2.10 Laparoscopic Adrenalectomy :
Laparoscopic adrenalectomy (LA) has become a gold standard in the management of most of the adrenal disorders, after it was decribed by Schuessler et al in 1993 and matched it success with open.19 Apart from advantages like early recovery, reduced hospital stay and cosmesis, the main benefits of LA over open adrenalectomy are decreased incidence of intra-operative and post-operative hemorrhage, decreased morbidity and mortality.
2.11 Transperitoneal Laparoscopic Adrenalectomy :
This involves putting 12mm port in the umbilicus or at the lateral border of rectus abdominis muscle just above the level of umbilicus. Two subcostal 5mm ports at midclavicular line and in the lateral border of the rectus and another 3.5mm subcostal trocar - anterior axillary line, for the left adrenals. The Right is approached through a mirror image and an additional epigastric port to the left of the liver for its retraction.20
Right adrenalectomy can also be performed with four ports. The primary Camera port 10 mm to be placed at about 3 cm lateral and cephalad to the umbilicus. Two working ports, 5 mm and 10 mm are placed in the midclavicular position, the upper one (5 mm) below the costal margin, and the lower one (10 mm), 10-12 cm below the upper one. Another 5 mm port is to be placed in the sub-xiphisternal position for liver retraction. A fifth 5 mm port, if required, is placed in the right anterior axillary line, to facilitate retraction or suction.20, 21
And another approach is to put the telescope’s trocar at the umbilicus while maintaining the positions of the other trocars.20 In the case of the left usually the first three ports are placed in a mirror image of the right. A fourth 5 mm port, if required, is placed in the left mid-axillary line to facilitate retraction 20, 21, 22
2.12 Retroperitoneal Lateral Laparoscopic Adrenalectomy :
Retroperitoneal lateral approach to the left adrenal gland is through an incision at the inferior edge of the 12th rib in which the camera port is placed, the second port 5mm at anterior axillary line midway between the iliac crest and costal margin, third port is placed posteriorly between the 12th rib and iliac crest along the lateral border of sacrospinatus muscles and the fourth port for retraction is placed cephalad to the first port at anterior axillary line. The right side is a mirrow image of the left but the liver lobe is retracted percutaneously reducing the ports number to three.23
Retroperitoneal posterior approach described by Walz et al, and thoracoscopic transdiaphragmatic approach described by Gill et al are not commonly used.20
2.13 Less- Adrenalectomy :
The approach is usually through trans umblical incision and placement of multichannel single Gelport and 3.5mm ports for flexible laparoscope, SILS dissector and tissue sealing device; and the adrenal gland approached anteriorly in cases of right side with no mobilization of the right lobe of the liver, and the left is approached laterally.23 Retroperitoneal LESS adrenalectomy has also been described.
2.14 Laparoscopic Approaches To The Ureter :
A three port approach with primary port at the umbilicus, one 5 mm port midway between the umbilicus and the medial costal margin and a 5 mm port midway between the anterosuperior iliac spine and the umbilicus, was described.24
Umblical port with, ipsilateral hypochondrium and iliac fossa as working ports have been described for approaches to upper and mid ureter while ipsilateral paraumblical and suprapubic ports for lower ureter while maintaining the umblical port.25
In cases of retrocaval ureter. A three port approach with a primary port at 2.5 cm to the right of umbilicus, a 5 mm port midway between the primary port and right costal margin, and on right mid-clavicular line, and another 5 mm port midway between the antero-superior iliac spine and the umbilicus was used while the patient is placed in the left lateral position. Mobilization of the ureter in the interaortocaval region require additional 5 mm port to be inserted at the flank.17
LESS approach to lower ureter through suprapubic transvesical port has been described. 26
2.15 Laparoscopic Prostatectomy :
Laparoscopic simple or radical prostatectomy has been performed through almost the same approach. The commonly described conventional laparoscopy is through a primary port placed upper side of the umbilicus. Then secondary ports at upper margin of the pubic bone and levels of the anterior superior iliac spines bilaterally and the fifth port at a point midline at about 15cm from the pubic bone. 27, 28 while others described both iliac fossae for the last two ports, most especially when it is to be robotic assisted, 29 others described the distance of the second and third ports to be 8-10cm from the camera port. 30
Transumblical LESS radical prostatectomy was first described in 2008 by Kaouk and colleagues, through the umbilicus using a single three-channel port, and two years later Desai et al published the initial series of single-port transvesical simple prostatectomy where a single-port device inserted percutaneously into the bladder through a 2-3 cm incision in the suprapubic skin crease was used.5
2.16 Laparoscopic Cystectomy :
Laparoscopic cystectomy has been described by many authors, but remains to be evaluated and is far from being a standard procedure. While some described a similar approach to prostatectomy with peri-umblical port, two others 8-10 cms away from the primary port and then bilateral iliac fossae,31 others described only four ports approach with 3-4cm supra-umblical camera port and two iliac fossae ports and suprapubic port32 and the sixth port is only needed during urinary diversion in radical surgeries.33
In the hand assisted approach a 7cm peri umblical incision is made as the hand port, Camera is placed at the left of the hand port in the midclavicular line at the level of the umbilicus, a second port is placed 5cm below the level of the umbilicus at right midclavicular line. A 10mm port is placed in the left anterior axillary line and a 5mm at midline about 5cm above the pubic symphisis.34
Kaouk et al described the laparoscopic radical cystectomy and pelvic node dissection through a single umbilical port and an extracorporeal urinary diversion by way of extension of the umbilical port site.5
2.17 Laparoscopic Varicocelectomies :
Laparoscopic varicocelectomy is generally performed transperitoneally, but extra or retroperitoneal has also been described. And two trocars or single trocar approaches described, but generally three trocars are required especially in bilateral cases.35
Varicocelectomy is performed in a trans peritoneal laparoscopic fashion with two ports placed at supraumblical and caudal and lateral to the umbilicus on the contralateral side of the varicocele.36
For the three ports approach, some described the sub-umblical camera port with secondary trocars at midline half way between umbilicus and pubic symphisis, and the other at midclavicular line 1-2cm below horizontal line to the umbilicus while maintaining subumblical camera port, 37 while others described umblical primary port and both lower abdominal quadrants ports. 38, 39
2.18 Mitrofanoff :
A four port transperitoneal approach is described, with camera at umbilicus, two 5mm at left lower quadrant and right midaxillary line at the level of the umbilicus. Fourth port at left midaxillary also at umblical level. 40
2.19 Other Less Procedures :
Single-site laparoscopic surgery has been reported in small numbers for a variety of other urological conditions. A mesh sling has been successfully removed from the bladder via a transvesical approach. Sacrocolpopexies, orchidopexy and orchidectomy have been successfully performed through a single-incision without complication.5
Methodology
Justification For The Study :
This study was justified by the difficulties, prolonged operative time, and unnecessary additional ports and other complications of wrong port positioning challenging laparoscopic urologist during various procedures. This result will minimize if not completely eliminate the above mentioned problems.
Materials And Methods :
This study (descriptive cross sectional study) was conducted on both dry and wet laboratories; and also some data were recorded from living donour nephrectomies. Different ports were inserted at different positions and provided manipulation angles of 30, 60 and 90 degrees and were used to perform surgeon’s knots on the dummies, renal vessels ligation and uretero-ureteric anastomosis on the swine to represent common laparoscopic tasks performed in the region of the upper urinary tracts. Timing for the procedures performed by Diploma students who had similar exposure to laparoscopic training were recorded for the respective angles.
Pelvic ring transfer and surgeons knot were also performed on the dummies to represent the common procedures performed on the region of lower urinary tracts and timing and manipulation angles were kept as above. The recorded timings were validated using χ2, presented on tables and graphs. The timings of laparoscopic donor nephrectomy was taken, manipulation angles estimated, validated and presented on charts.
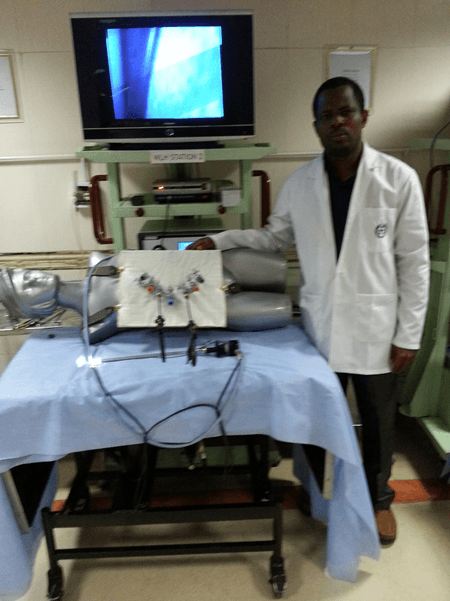
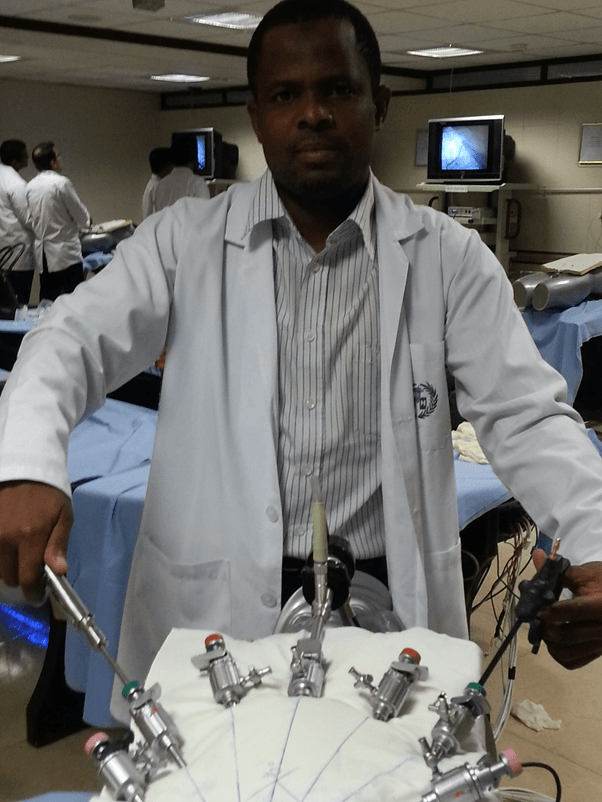
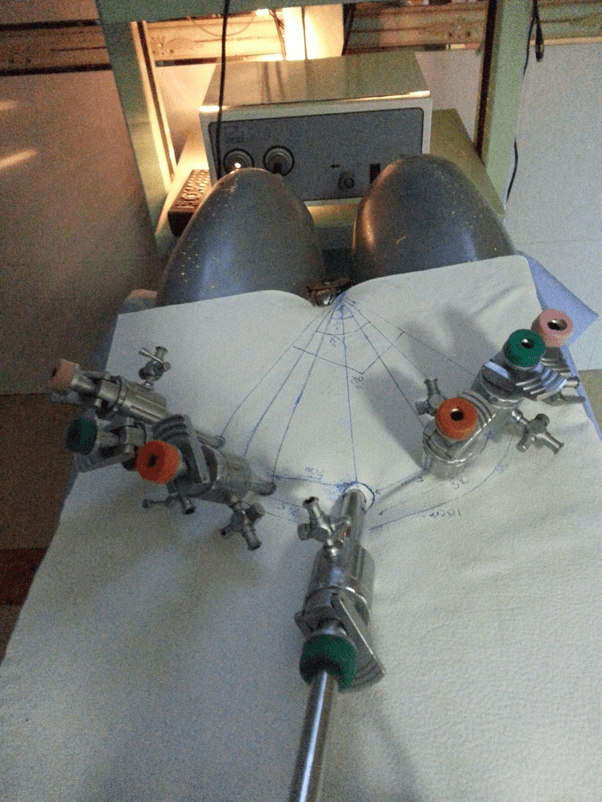
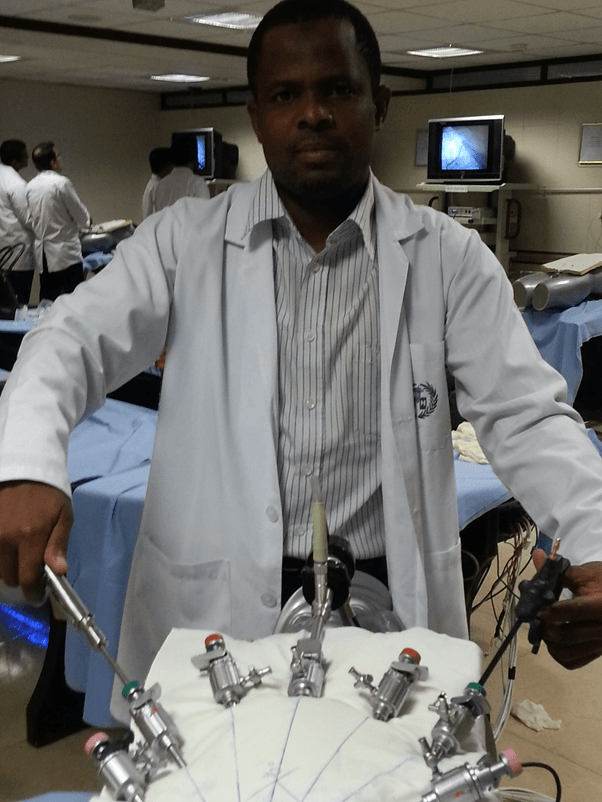
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Dummies.
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Dummies.

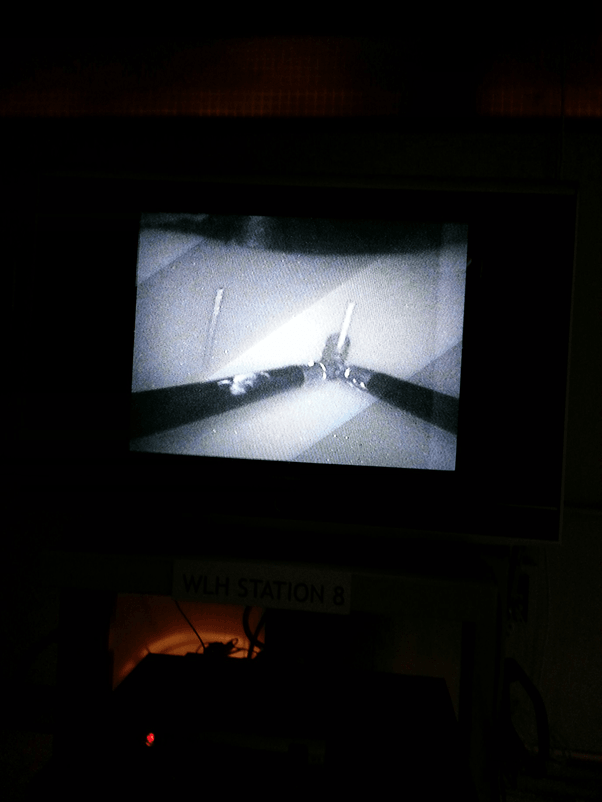
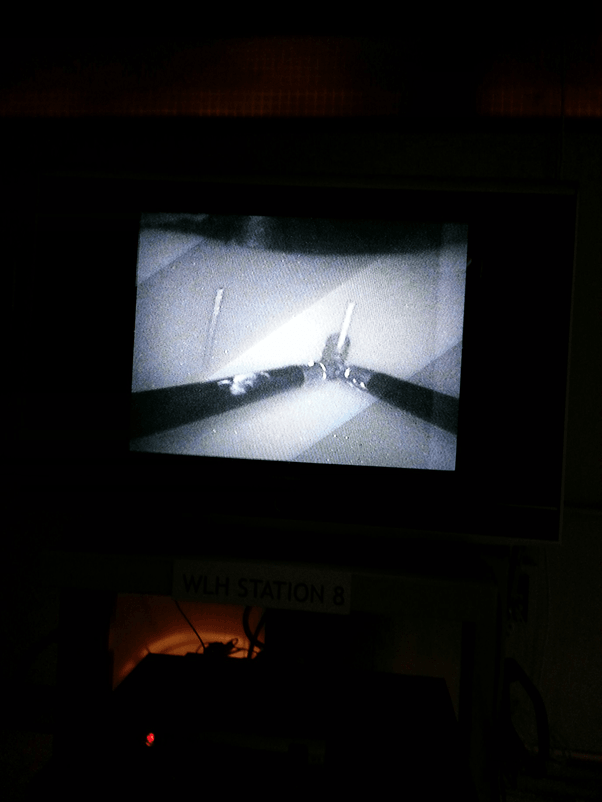
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Swine With Illumination.
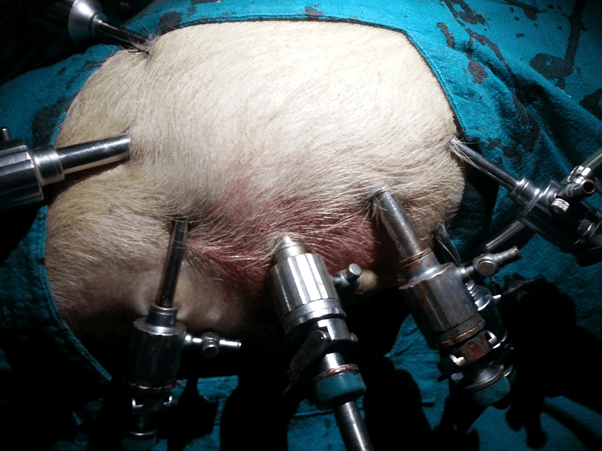
Picture Showing The Ports Positioning For The Upper Tract Tasks On The Swine.
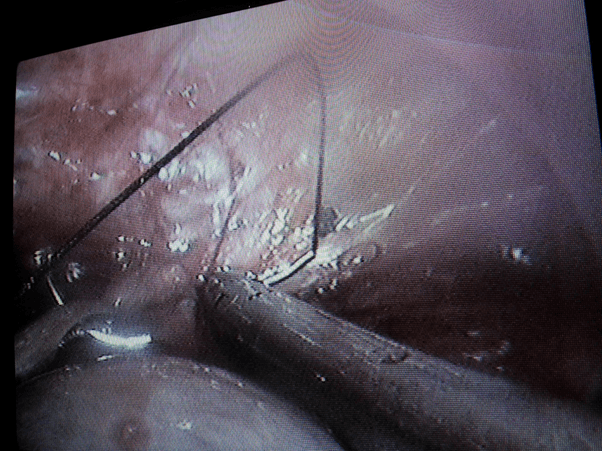
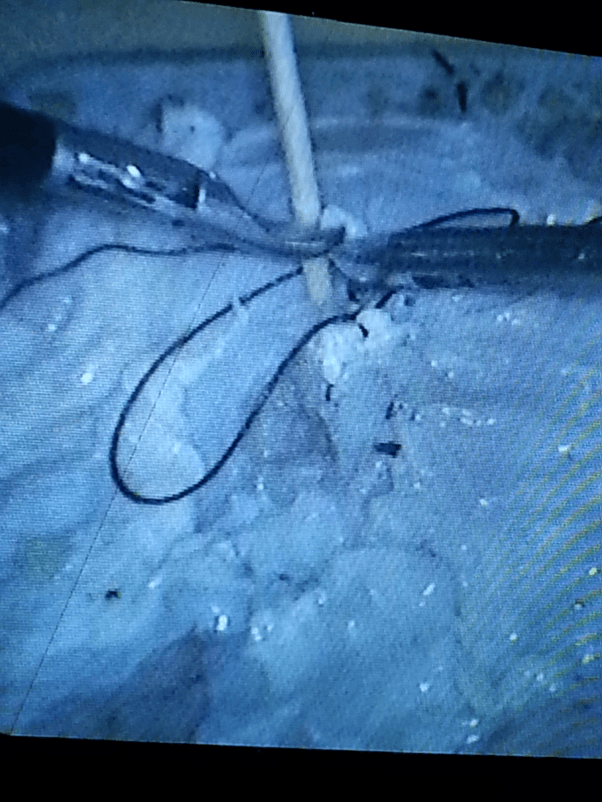
Picture Showing The Approximate Manipulation Angle While Knotting In The Upper Tract In A Swine.
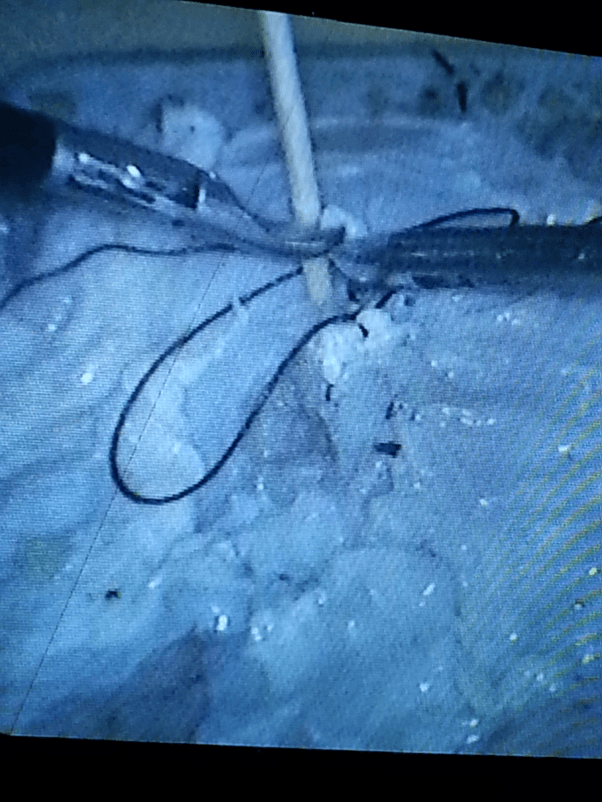
Tying A Knot Around A Fixed Distance To Ensure The Manipulation Angle Is Maintained.
Arrangement Of Ports Positions For Tasks In The Pelvis.
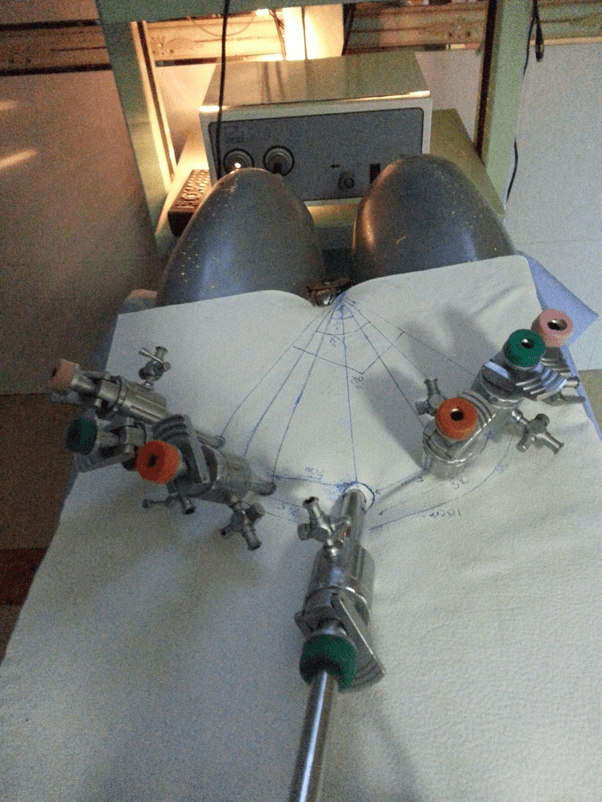
Discription Of Ports Sites On The Anterior Abdominal Wall.
A Picture Of Ring Transfer In The Pelvis At 60 Degree Manipulation Angle.

Performing A Task With 90 Degree Manipulation Angle In The Pelvis.
Estimation Of Manipulation Angles Determining Ports Positions On The Dry Lab Anterior Abdominal Wall.
Showing Instruments And Ports At Different Positions Of Task Performance.
Picture Showing The Working Angle At One Of The Ports Positions In A Donor Nephrectomy.
Port Positions For Left Laparoscopic Donor Nephrectomy.
Ports Positions
Sites Of Ports Positions After Left Donor Nephrectomy.
Picture Of Manipulation Angle.
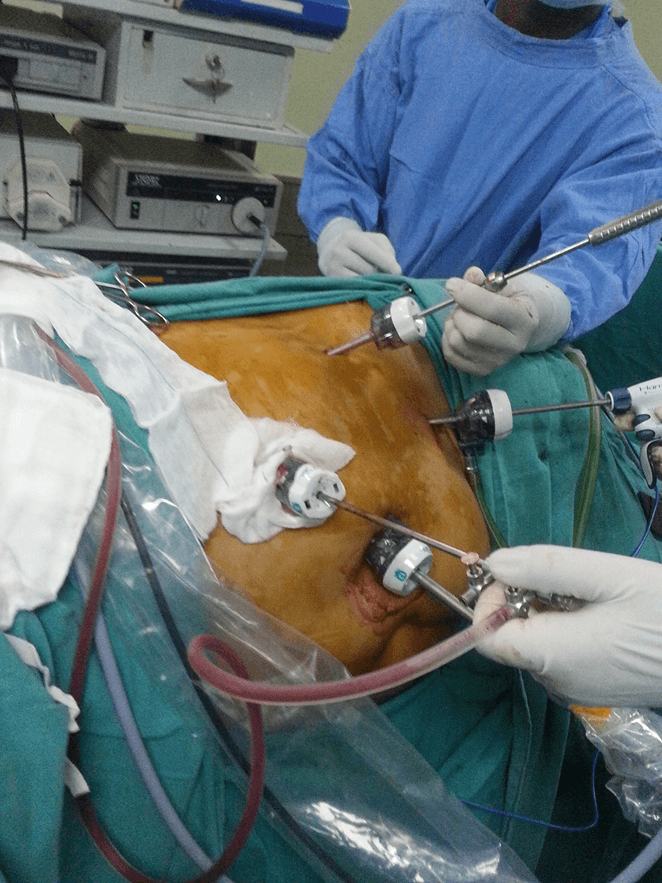
Port Positions.
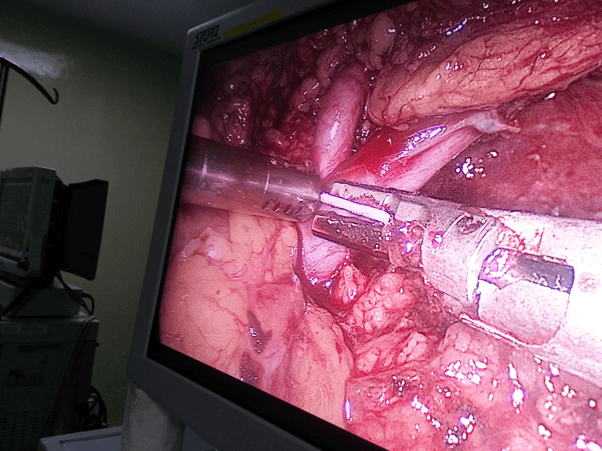
Manipulation angle at the hilum ( crutial target of dissection ).
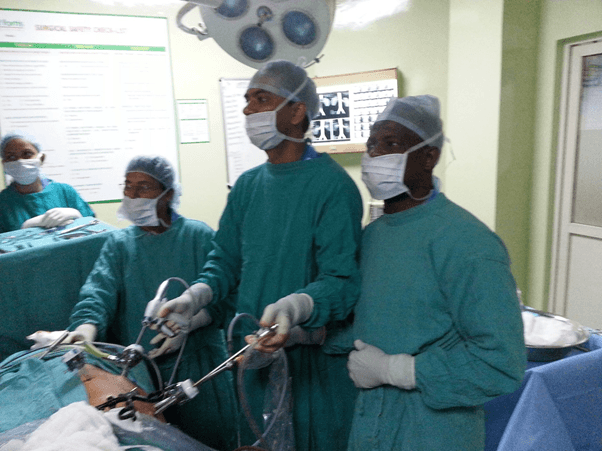
Laparoscopic Surgical Team of the Investigator.
Study Area.
The study was conducted world Laparoscopy Hosptital, Gurgaon. An accredited centre by The Global Open University of Nagaland, to train to masters and PhD in minimal access surgery. World Laparoscopy Hospital is the premier institute of Minimal Access Surgery. It was established to ensure the highest standard of training, treatment and research in laparoscopic and robotic surgery. It's been 12 years since World Laparoscopy Hospital is center of excellence for training in laparoscopic surgery. Laparoscopic Courses of World Laparoscopy Hospital are university recognized and is recognized by World Association of Laparoscopic Surgeons. Courses are internationally accredited by International Accreditation Organization, USA. Robotic Surgery Training is recognized by International College of Robotic Surgeons and endorsed by Intuitive Surgical incorporation da Vinci® Surgical System, USA. This institute excel in specialized medical care supported by comprehensive research and education.41
The Global Open University of Nagaland, is a joint public-private partnership venture between the Government of Nagaland and the World Institution Building Programme (WIBP). It is recognized as a State University by the University Grants Commission of India (UGC), the Association of Indian Universities (AIU) International Association of Educators for World Peace, to confer degrees as on par with the degrees conferred by its members. The Global Open University offers academic degree programmes at both undergraduate and postgraduate levels in many desciplines.42
Sample Size Determination/ Sampling Technique
Conventional sampling was used and 20 chosen based on the previous records of average number of Diploma students.
Study Population
The subjects were recruited as for routine laboratory work. Consecutive selection was done until the sample size was achieved.
Ethical Consideration
All ethical issues binding on the laboratory and research on animal subjects were respected.
Limitations Of The Study.
1. It was difficult to perform each urological procedure, as such regional representation were chosen.
2. The sizes of the animals were small, for which we could not demonstrate port placement for 90 degree manipulation angles in the wet lab, rather only dry lab was used for the lower tract representation.
3. Less number procedures on the lower urinary tract are performed laparoscopically in our centre, as such we could not have human timing representation as we did for the donor nephrectomy.
Conflicts Of Interest
No conflict of interest declared, neither any instrument name was mentioned
Results And Discussions
TABLE 1 A: Timing for surgeon‘s knot in upper urinary track with manipulation angle 30 0.
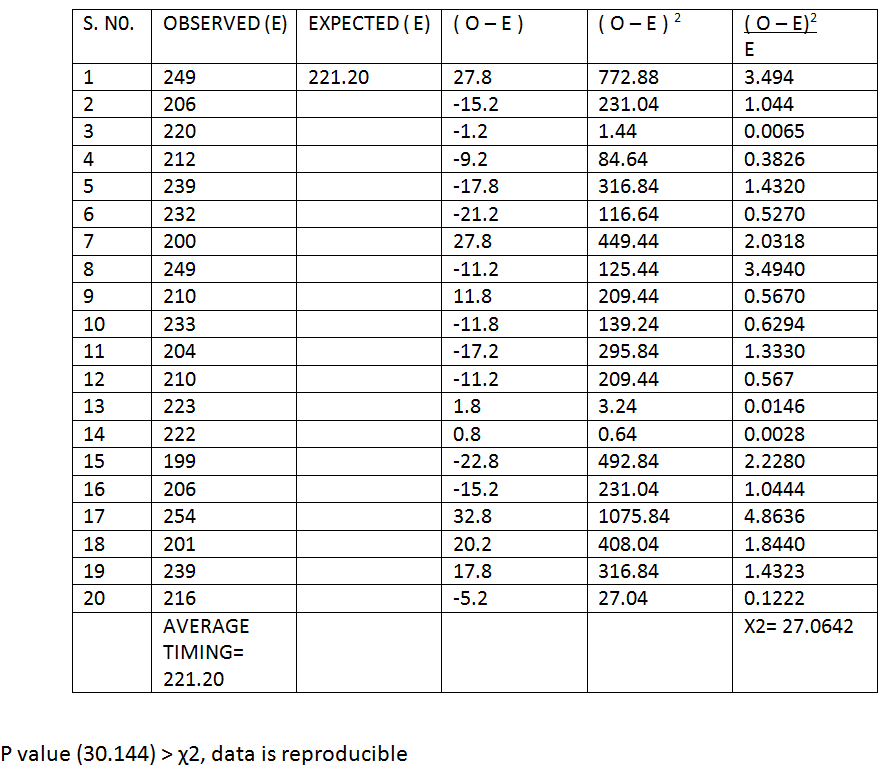
TABLE 1 B: Timing for surgeon‘s knot in upper urinary track with manipulation angle 600.
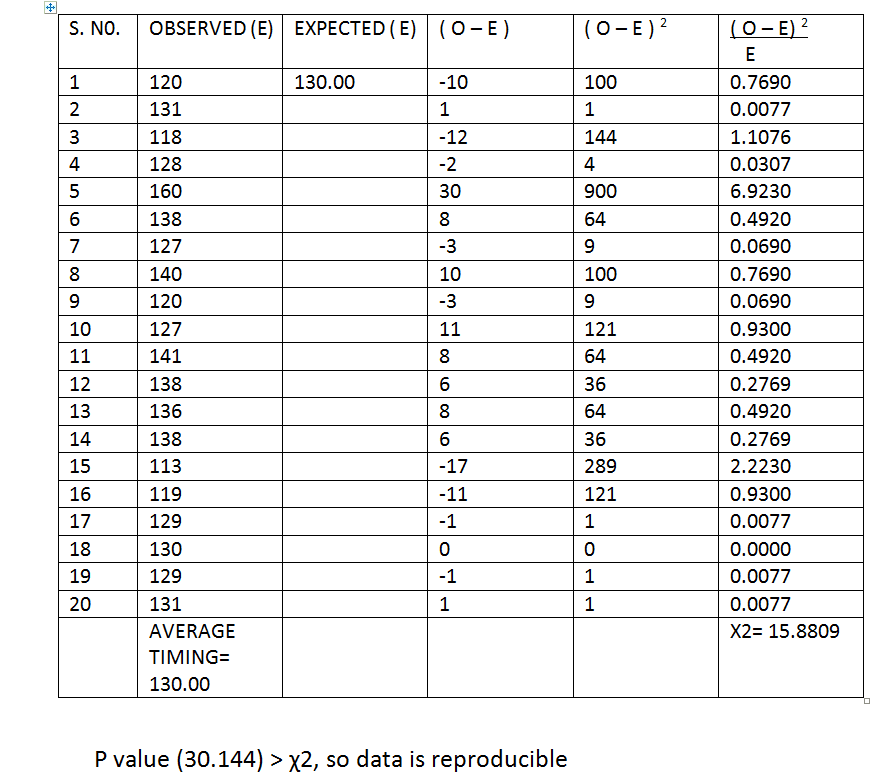
TABLE 1 C: Timing for surgeon‘s knot in upper urinary track with manipulation angle 90 0.
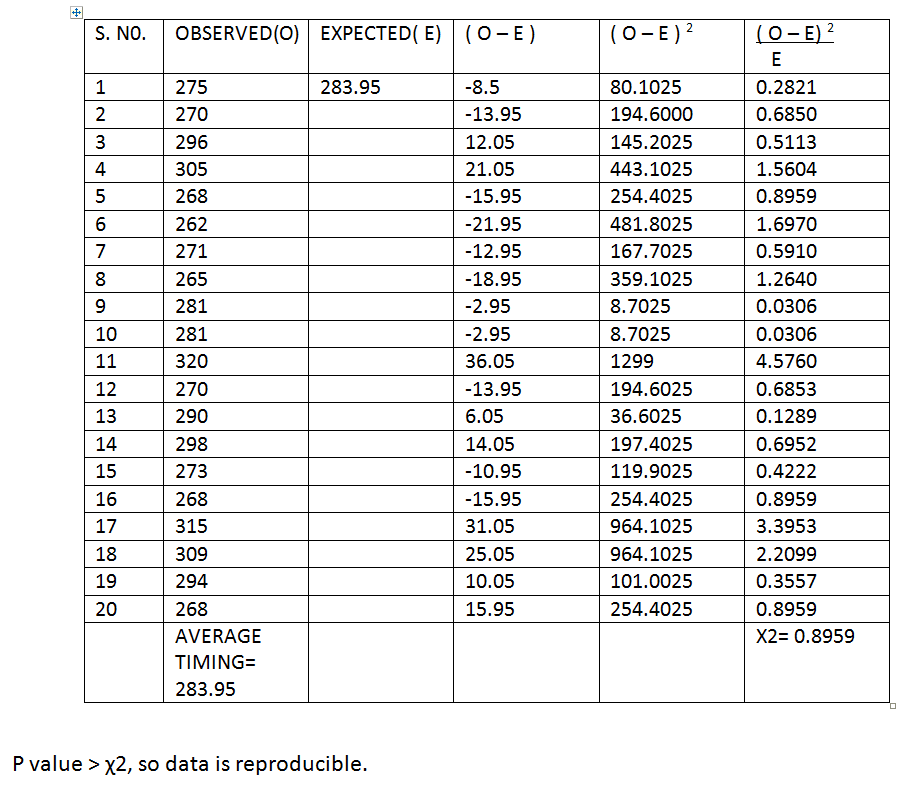
TABLE 1: Average timing of surgeon’s knotting in the region of the upper urinary tract with respective manipulation.
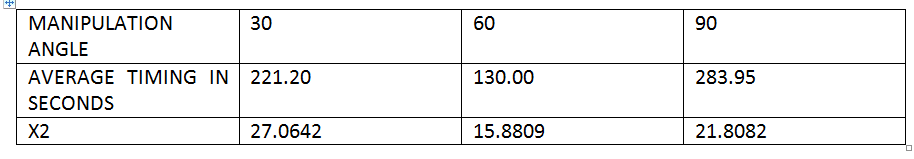
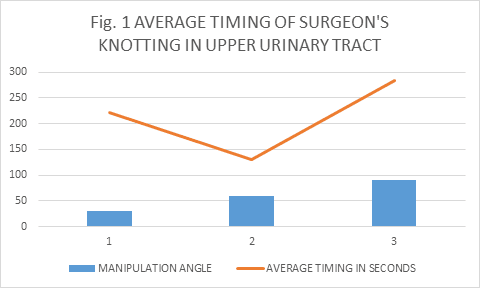
Discussion 1
Tables 1A, B and C showed readings of timing obtained while making a surgeon’s knot in the region of upper urinary tract in the dummy at different manipulation angles which were validated by χ2 tests and average obtained. The averge timing in seconds for 30, 60 and 90 degrees were 221.20, 130.00 and 283,95 respectively. Although all the readings were reproducible at P value( 30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees.
This is shown on figure 1.
TABLE 2A: Timing of clipping of renal vessels at 30 degree manipulation angle.
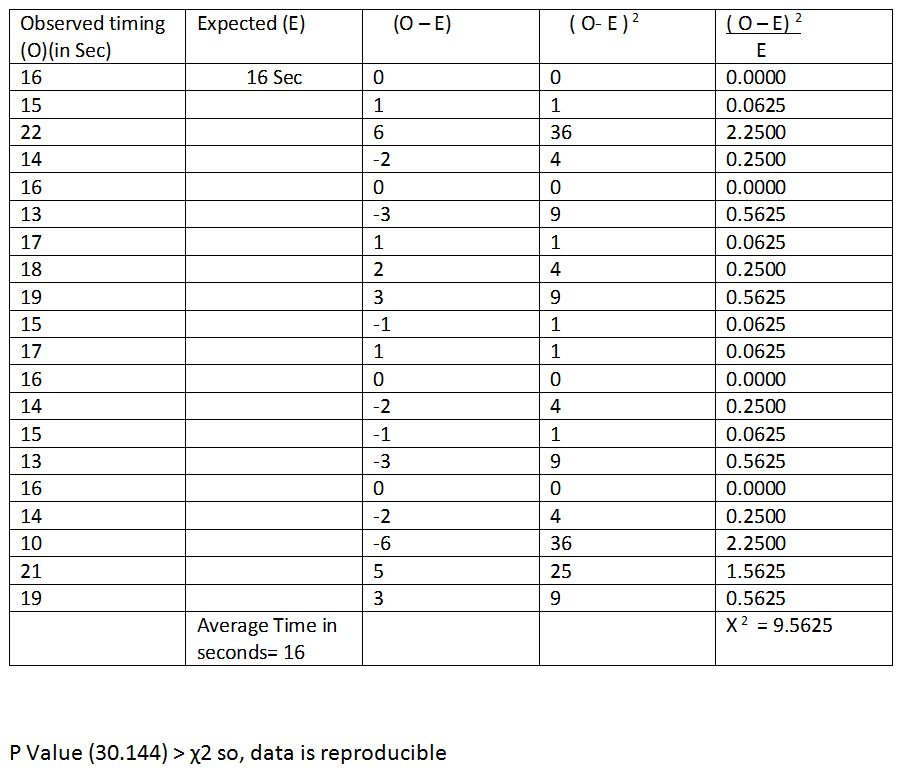
TABLE 2B: Timing of renal vessels clipping with manipulation angle of 60 degree.

TABLE 2c: Timing for renal vessel ligation with manipulation angle 90 0 .
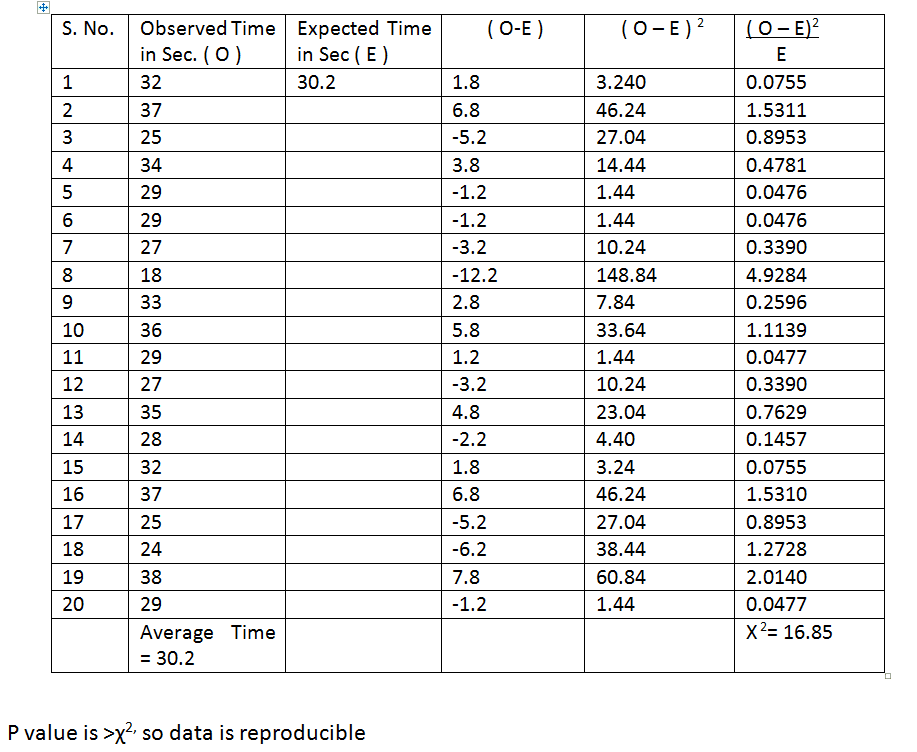
TABLE 2: Average timing of renal vessels clipping.
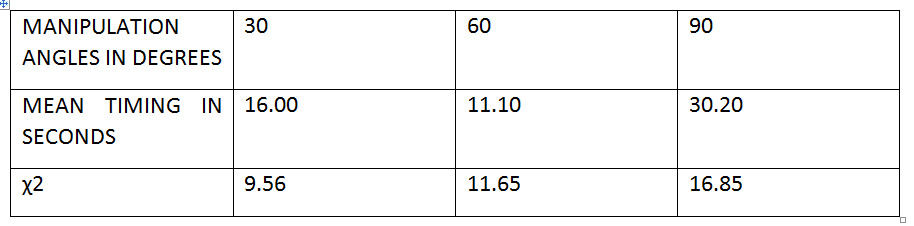
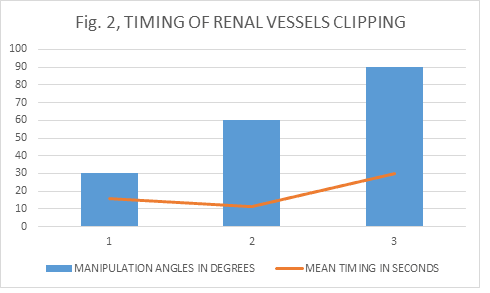
Discussion 2
Tables 2A, B and C showed readings of timing taken to clip a renal vessel in the swine at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 16.00, 11.10 and 30.20 respectively. Although all the readings were reproducible at P value (30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees, and the angle 60 followed by 30 were more reproducible than 90 degrees.
This is shown on figure 2.
TABLE 3A: Timing of ligation of uretero- ureteric anastomosis with 30 degree manipulation angle.
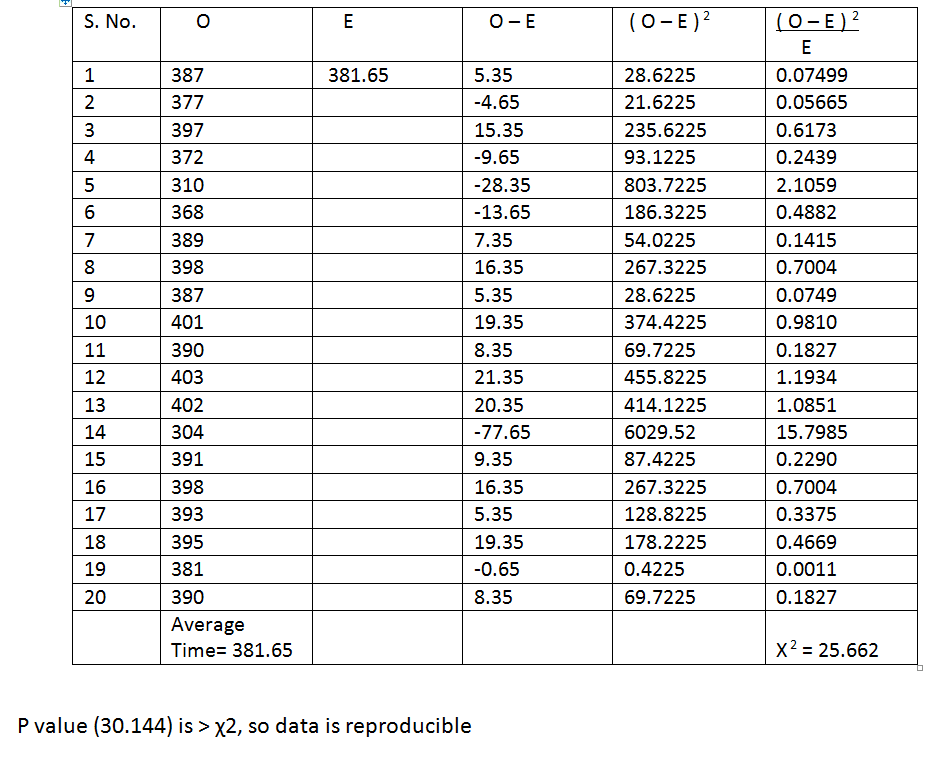
TABLE 3B: Uretro-ureteric anastamosis with manipulation angle 60 0.
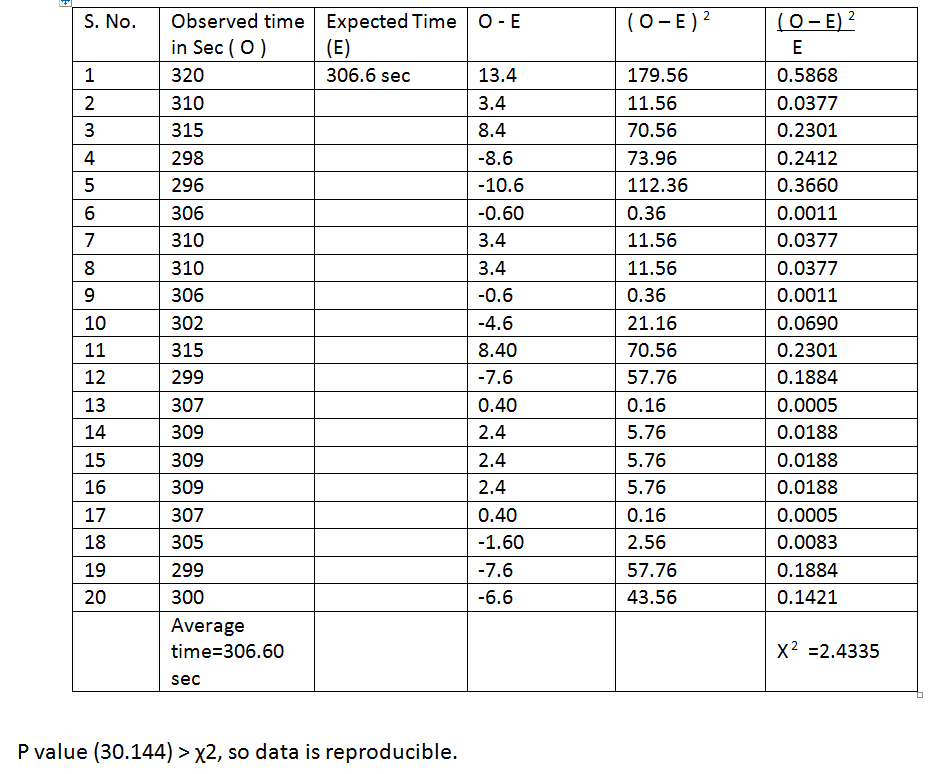
TABLE 4C: Timing for uretero-ureteric anastamosis at manipulation angle 90 0.
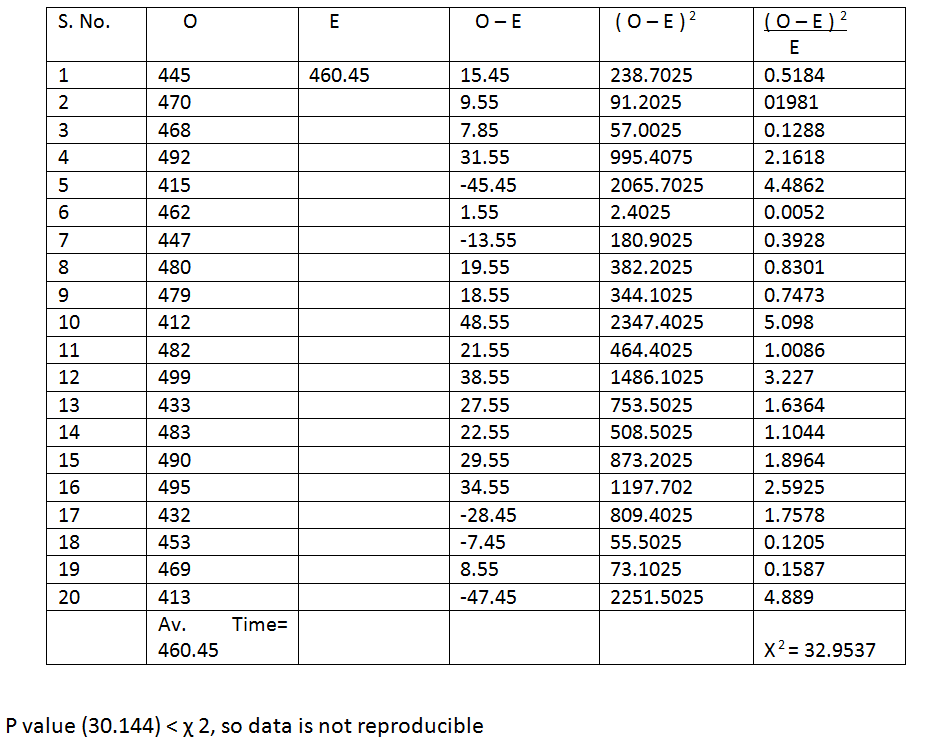
TABLE 4: Average Timing For Uretero-Ureteric Anastomosis.
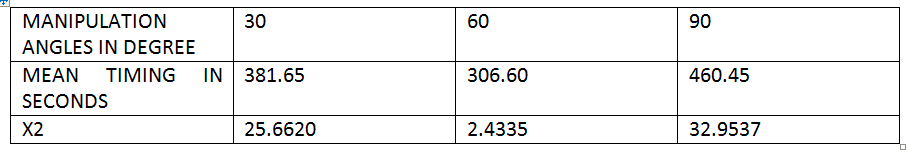
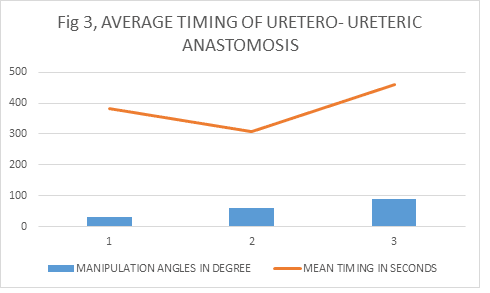
Discussion 3
Tables 3A, B and C showed readings of timing taken for uretero-ureteric anastomosis in the swine at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 381.65, 306.60 and 460.45 respectively. Only readings at 30 and 60 degrees were reproducible at P value (30.144), 5% level of significance; but the χ2 of readings at 90 was less than P value, indicating non reproducibility. These suggest that the 60 degree angle has shorter operative time then the 30; and also demonstrated that the more difficult a laparoscopic task is , is more likely it become non reproducible at an angle of 90 degrees and above, probably due to fatique from high elevation angle and shoulder over stretching due to poor ergonomics. 43
This is shown on figure 3.
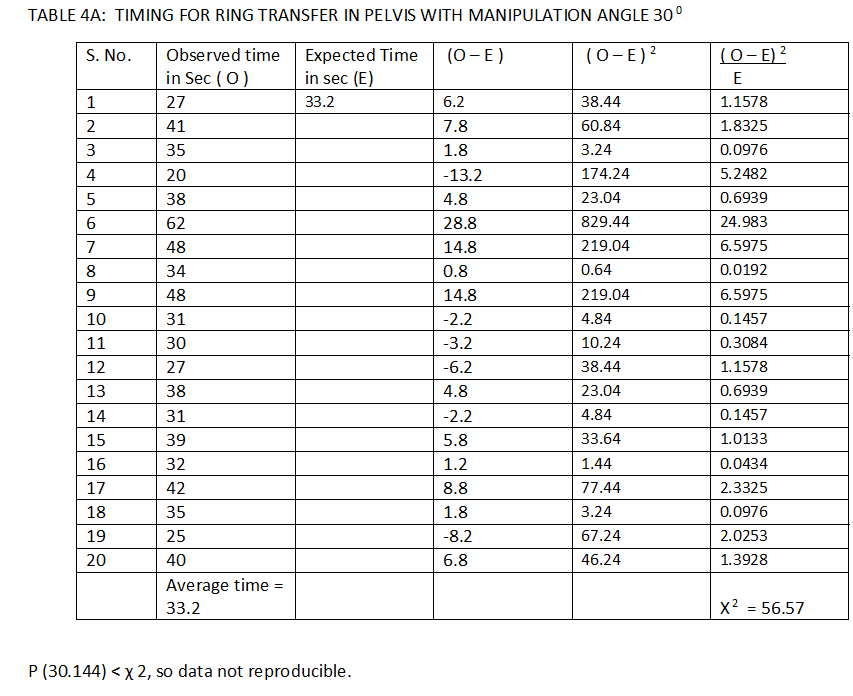
TABLE 4B: Time for ring transfer in pelvis with manipulation angle 60 0.
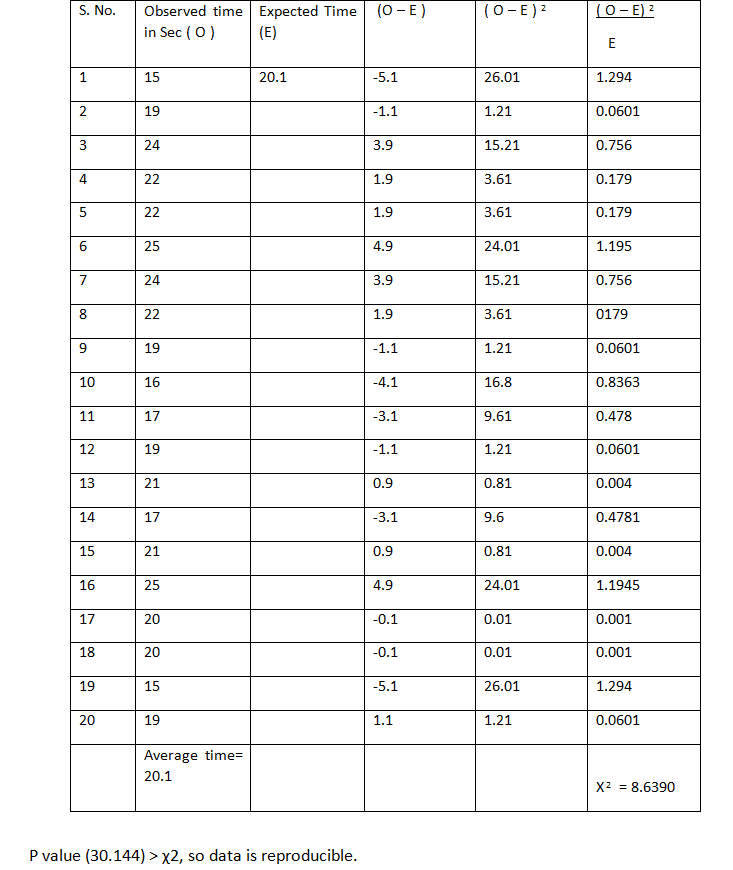
TABLE 4C: Timing for ring transfer in pelvis with manipulation angle 90 0.
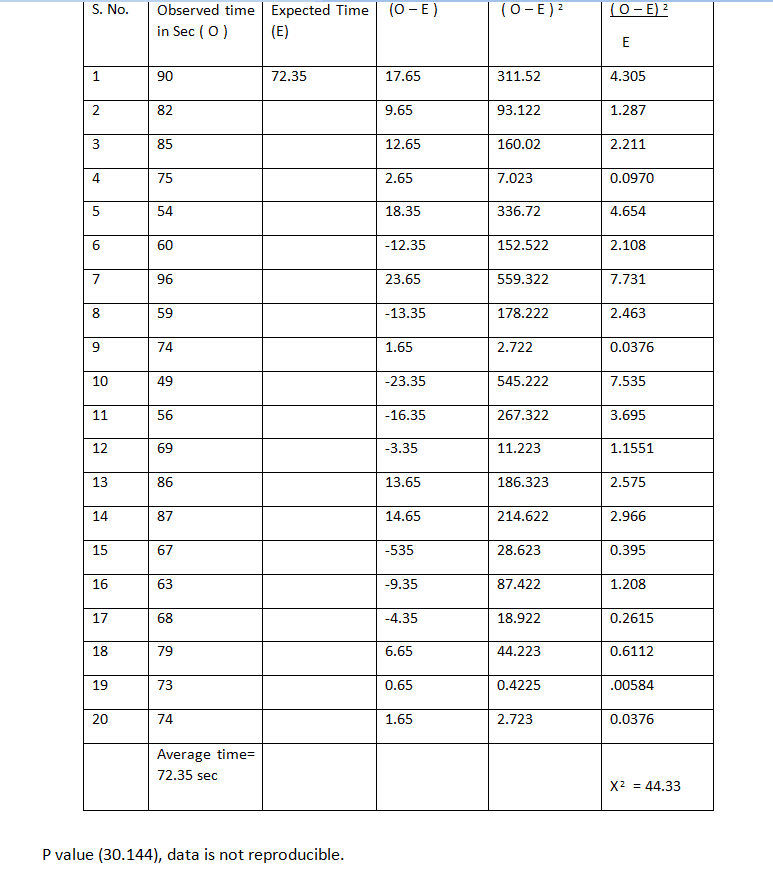
TABLE 4: Averge Timing Of Ring Transfer In The Pelvis
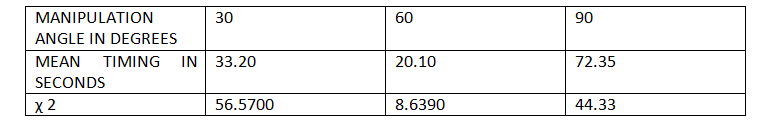
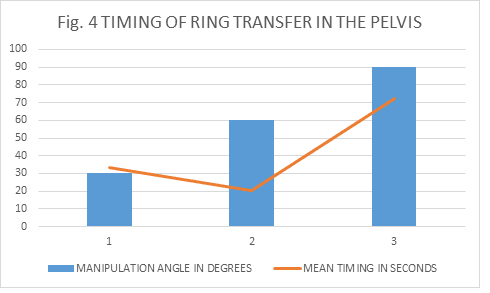
Discussion 4
Tables 4A, B and C showed readings of timing taken for ring transfer in the pelvic region of the dummies at different manipulation angles, which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 33.20, 20.10 and 72.35 respectively. Here only the readings at 60 degree manipulation angle were reproducible at P value (30.144), 5% level of significance: which further support any port position that will provide working angle of 6o degree as the ideal.
This is shown on figure 4.
TABLE 5A: time for surgeon’s knot in pelvis with manipulation angle 30 0.
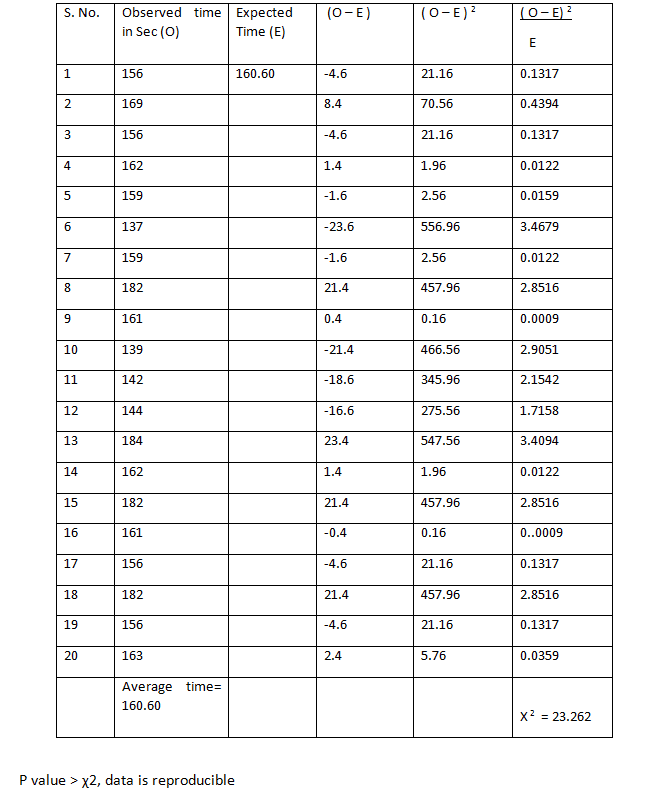
TABLE 5B: time for surgeon’s knotting in pelvis with manipulation angle 60 0.
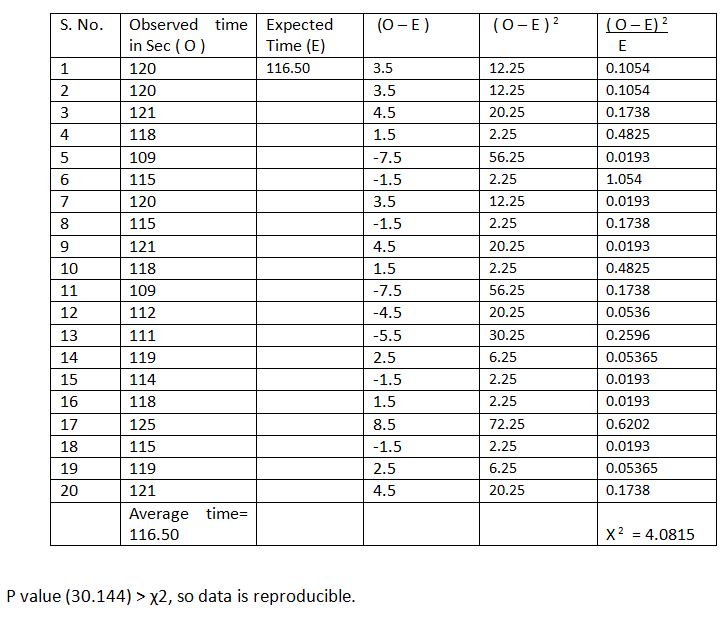
TABLE 5C: Time for surgeon’s knotting in pelvis with manipulation angle 90 0.
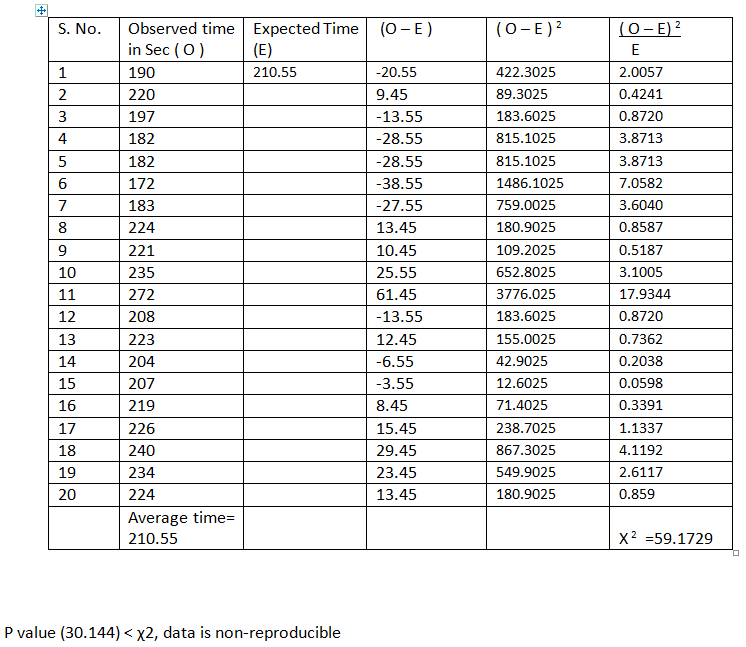
TABLE 5: Average Timing For Surgeon’s Knotting In The Pelvis.
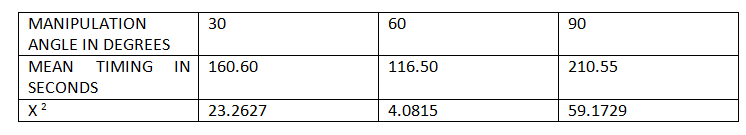
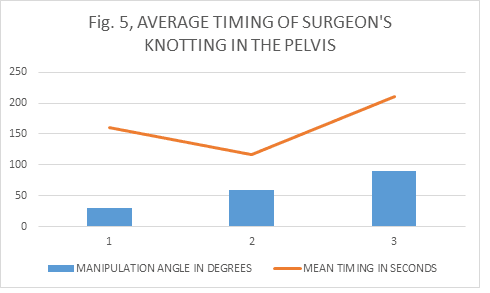
Discussion 5
Tables 5A, B and C showed readings of timing of surgeon’s knotting in the pelvic cavity of dummies at different manipulation angles which were validated by χ2 tests and average obtained. The average timing in seconds for 30, 60 and 90 degrees were 160.60, 116.50 and 210.55 respectively. Despite the facts that, the first two readings were reproducible at P value (30.144), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time than that of 30 degrees. The readings of 90 degree angle were non reproducible for surgeons knotting in the pelvis indicating increased difficulties and time consumption when ports are positioned in such a way that will give working angle of 90 degrees and above.
This is shown on figure 5.
Laparoscopic Donour Nephrectomy
TABLE 6A: Timing of laparoscopic donour nephrectomy with approximate 30 degree manipulation angle.
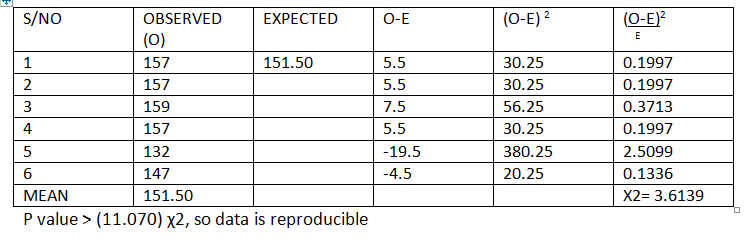
TABLE 6B: Timing of laparoscopic donor nephrectomy with approximate 30 degree manipulation angle.
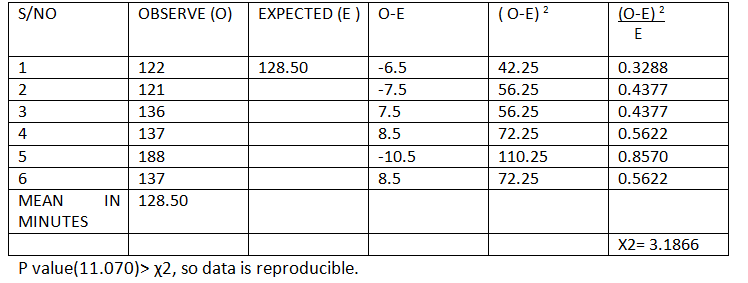
TABLE 6C: Approximate manipulation angle of 90 degrees and timing of donour nephrectomy in minutes.
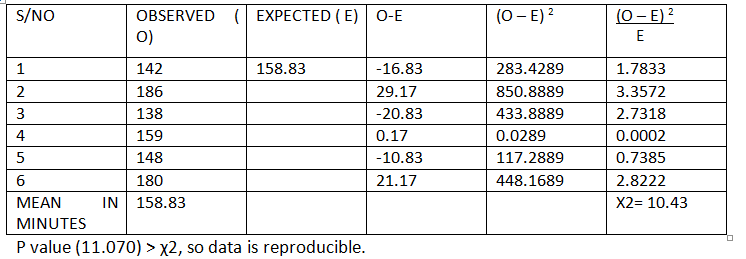
TABLE 6: Average duration of laparoscopic donor nephrectomy in minutes.
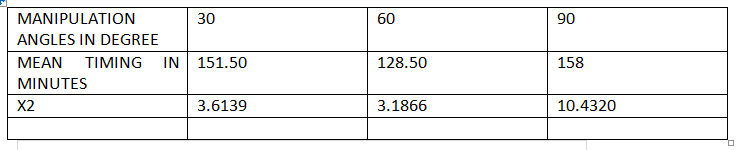
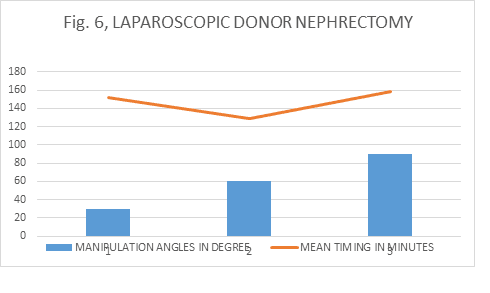
Discussion 6
Tables 6A, B and C showed readings of timing taken for laparoscopic donor nephrectomy and manipulation angles were approximated nearest to 30, 60 and 90 degrees. The readings obtained in minutes were validated by χ2 tests and average obtained. The averages were 151.50, 128.50 and 158.83 respectively. Although all the readings were reproducible at P value (11.070), 5% level of significance: it has clearly demonstrated that the 60 degree angle has shorter operative time followed by 30 and then 90 degrees, and the angle 60 followed by 30 were more reproducible than 90 degrees.
This is shown on figure 6.
Overall Discussion, Conclusion And Recommendations
5.1 Discusion
From all the discussions above, the average timing of all laparoscopic tasks were shorter with 60 degree manipulation and all were reproducible irrespective of the difficulty of the tasks then followed by 30 degree. The 90 degree angle has the longest operative time, and in some cases non reproducible, indication the closer the manipulation angle is to the 90 degrees and above, the more the likely to take longer operative time and the higher it approaches non reproducibility due to fatigue from increased elevation angle and shoulder overstretching. This is in keeping with the Baseball Diamond concepts of port positioning.
Conclusion
There is no “Ideal port position in urological laparoscopic procedures based on anatomical land marks, but the closer the ports positions are to make a manipulation angle of 60 degrees (Base Ball Diamond), the closer to ideal it will be.
Recommmendations
More work is to be done on the newly emerging laparoscopic urology particularly in the developing world.
References
1. Supe AN, Kulkarni GV, Supe PA. Ergonomics in laparoscopic surgery. J Min Access Surg 2010;6: 31-36.
2. Karthik S, Augustine AJ, Shibumon MM, Pai MV. Analysis of laparoscopic port site complications. A descriptive study. J Min Access surg 2013;9:59-64 .
3. Greberg CF, Gettman MT. Instrumentation for natural orifice transluminal endoscopic surgery and laparoendoscopic single-site surgery. Indian J urol 2010;26:385-8 .
4. Gupta NP, Gautam G. Laparoscopic nephrectomy for benign non-functioning kidneys. J Min Access Surg 2005; 149-54.
5. Maurya K, Sivanandam SE, Sukumar S, Bhat S, Kumar G, Nair B. Concomitant laparoscopic urological procedures: Does it contribute to morbidity? J Min Access Surg 2009; 5:67-71.
6 WORLD LAPAROSCOPY HOSPITAL. Cyberciti, DLF Phase II, NCR Delhi, Gurgaon, 122 002, India. Port position In Laparoscopy.
7. Gupta N, Raina P, Kumar A. Laparoscopic donor nephrectomy. J Min Access Surg 2005; 155-64.
8. McDougall EM, Finley D, Clayman RV et al. Basic urologic laparoscopy: A Standardized Guideline for Training Programs.American Urological Association Education and Research.2005; 20-25
9. Veenstra GM, Fossion LMCL, de Laet K, Luijten AAPM. Synchronous laparoscopic radical nephrectomy left and contralateral right hemicolectomy during the same endoscopic procedure. J Laparoendosc Adv Surg Tech 2004;
10 Chung BI, Liao JC. Laparoscopic radical nephrectomy in a pelvic ectopic kidney: Keys to success. JSLS. 2010; 14: 126–129.
11 Ganpule AP, Sharma R, Thimmegawda M, Veeramani M, Desai MR. Laparoscopic radical nephrectomy versus open radical nephrectomy in T1-T3 renal tumours. An outcome analysis. Indian J Urol 2008; 24:39-43
12 Rais-Bahrami S, Waingankar N, Richstone L. Upper tract urologic laparoEndoscopic single site surgery. Indian J Urol2012; 28:60-4
13 Kopp RP, Silbestin JL, Derweesh I. Laparoendoscopic single site radical nephrectomy with renal vein thrombectomy: Initial report. BMC Urology 2010; 8:10
14 Raman JD,Cadeddu JA.Single access Laparoscopic nephrectomy. Indian J Urol2008; 24:457-460
15 Greberg CF,Gettman MT. Instrumentation for natural orifice transluminal endoscopic surgery and laparoendoscopic single site surgery. Indian J Urol 2010; 26:385-8
16. Thiel DD. Navigating the difficult robotic assisted pyeloplasty. ISRN Urol 2012; 2:34
17. Singh O, Gupta SS, Hastir A, Arvind NK. Laparoscopic transperitoneal pyelopyelostomy and ureteroureterostomy of retrocaval ureter: Report of two cases and review of the literature. Journal of Minimal Access Surgery.Vol.2010; 6:53-55
18 Faddegon S,Tan YK, Olweny EO, Park SK, Sara L. Best BS, Cadeddu JA. Laparoendoscopic single-site (LESS) Pyeloplasty for horseshoe ureteropelvic junction obstruction. JSLS. 2012; 16:151–154.
19. Bansal P, Gupta A, Mongha R, Narayan S, Kundu AK, Chakraborty SC, et al. Laparoscopic versus open pyeloplasty: Comparison of the two surgical approaches- A single centre experience of three years. J Min Access Surg 2008; 3:76-9
20 Mellon MJ, Sethi A, Sundaram CP. Laparoscopic adrenalectomy: Surgical techniques. Indian J Urol 2008; 24:583-589
21 Kumar S, Bera MK, Vijay MK, Dutt A, Tiwari P, Kundu AK. Laparoscopic adrenalectomy: A single center experience. J Min Access Surg 2010; 6:100-105
22 : Dalvi AN, Thapar PM , Kumar KV, Kamble RS, Rege SA, Deshpande AA, Shah NS, Menon PS. Laparoscopic adrenalectomy: Gaining experience by graded approach. J Min Access Surg 2006; 2:59-66.
23 Sasaki et al. Laparoscopic single site adrenalectomy: Initial results of cosmetic satisfaction and the potential for post-operative pain reduction. BMC Urology 2013; 13:21
24 Nagraj HK, Kishore TA, Nagalakshmi S. Transperitoneal laparoscopic approach for retrocaval ureter. J Min Access Surg 2006; 2:81-2
25 Agrawal V, Bajaj J, Acharya H, Chanchalani R, Raina VK, Sharma D. Laparoscopic management of pediatric renal and ureteric stone. J P Urol 2013; 9:230-233
26 Ahlawat RK, Gaulam G. Suprapubic transvesical single-port technique for control of lower end of ureter during laparoscopic nephroureterectomy for upper tract transitional cell carcinoma. Indian J Urol 2011; 27:190-5
27 Cestari A, Buffi NM, Scapaticci E et at. Simplifying patient positioning and port placement during robotic assisted laparoscopic prostatectomy. European Urology 2010; 57:530-533
28. Ashis C, Adnan Q, Aziz A, Edward MD. Optimal port placement during laparoscopic radical prostatectomy. Can J Urol 2012; 19:6142-6146
29 Columbo JR, Santos B,Hafron J, Gianduzzo T, Haber GP, Kaouk JH. Robotic assisted radical prostatectomy: Surgical techniques. Int. Braz. J Urol2007; 33:803-9
30 Pow-Sang JM, Velasquez J, Myers MD, Rodriguez AR, Kang LC. Pure laparoscopic and robotic –assisted laparoscopic radical prostatectomy in the management of prostate cancer. Cancer control 2007; 14:250-7
31 Gerullis H, Kuemniel C, Popken G. Laparoscopic cystectomy with extracorporeal-assisted urinary diversion: Experience with 34 patients. European Urology 2007; 51:193-198
32 Cansino JR, Cisneros J, Aloso S et al. Laparoscopic radical cystectomy: Initial series and analysis of result. European Urology Suppl. 2006; 5:956-961
33 Vordos D, Hoznek A, Gettman M, Abbon CC. Laparoscopic cystectomy: Evolution of a new technique. EAU series 2005; 3:147-155
34 Peterson AC, Lance RS, Ahuja SK. Laparoscopic hand assisted radical cystectomy with ileal conduit urinary diversion. J Urol 2002; 168:2103-2105
35 Chan P. Management options of varicocele. Indian J Urol 2011; 27: 65-73
36 Link BA, Kruska JD, Wong C, Kropp BP. Two trocar laparoscopic varicocelectomy: Approach and outcomes. JSLS 2006; 10: 151–154.
37 Ivovic J. Laparoscopic surgery for varicocele in subfertile men. European Urology Suppl 2009; 8:626-627
38 Capolicchio JP, El-Sherbiny M, Brzezinski A, Eassa W, Jednak R. Dye-assisted lymphatic-sparing laparoscopic varicocelectomy. JPUrol 2013; 9:33-37
39 Moreira-Pinto J, Osorio A, Carvalho F, de Castro JR, de Sousa J, Enes C, Reis A,Cidade-Rodrigues J. Varicocelectomy in adolescents: Laparoscopic versus open high ligation technique. Afr J Paediatr Surg 2011; 8:40-43
40 Nerli RB, Reddy M, Devraju S, Prabha V, Hiremath MB, Jali S. Laparoscopic mitrafanoff appendicovesicostomy: Our experience in children. Indian J Urol 2012; 28: 28-31
41. www.worldlaparoscopyhospital.com/laparoscopic treatment training and research
42. www.globalopenuniversity.org
