24-hour pH Monitoring in Evaluating Patients Before and After Laparoscopic Fundoplication Surgery
DR Shiv Bagchi, MBBS MS FRCS(Edin) FMAS DMAS
World Laparoscopic Hospital Delhi INDIA
ABSTRACT:
Gastroesophageal Reflux Disease (GERD) remains a prevalent and challenging condition affecting millions of people worldwide. This review article offers a comprehensive synthesis of numerous literature sources. The existing body of research published regarding the role of 24- hour pH monitoring in the assessment of pre and post Laparoscopic Fundoplication, a commonly employed surgical approach for GERD management.
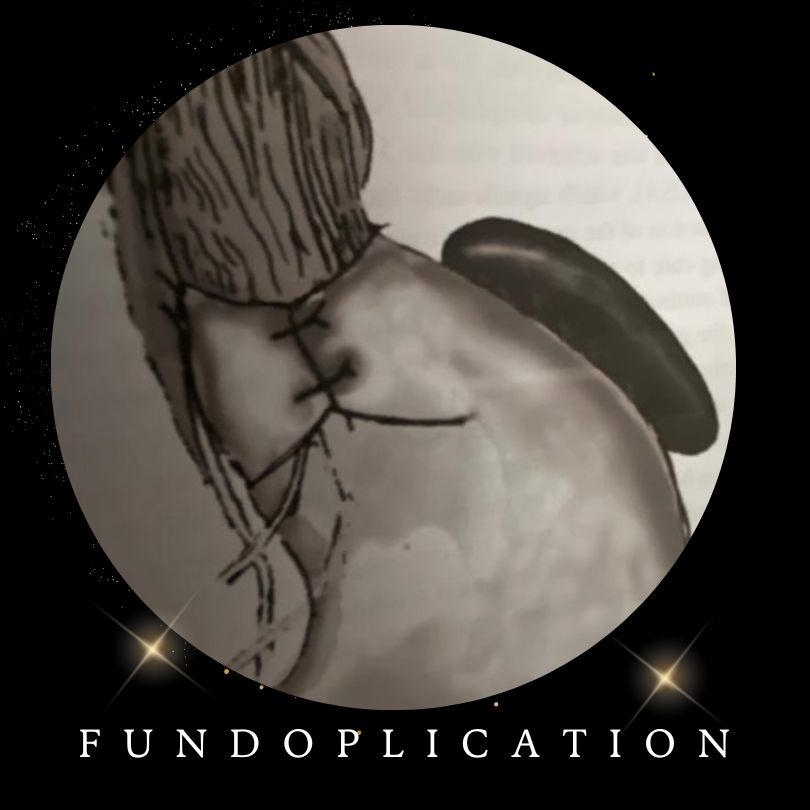
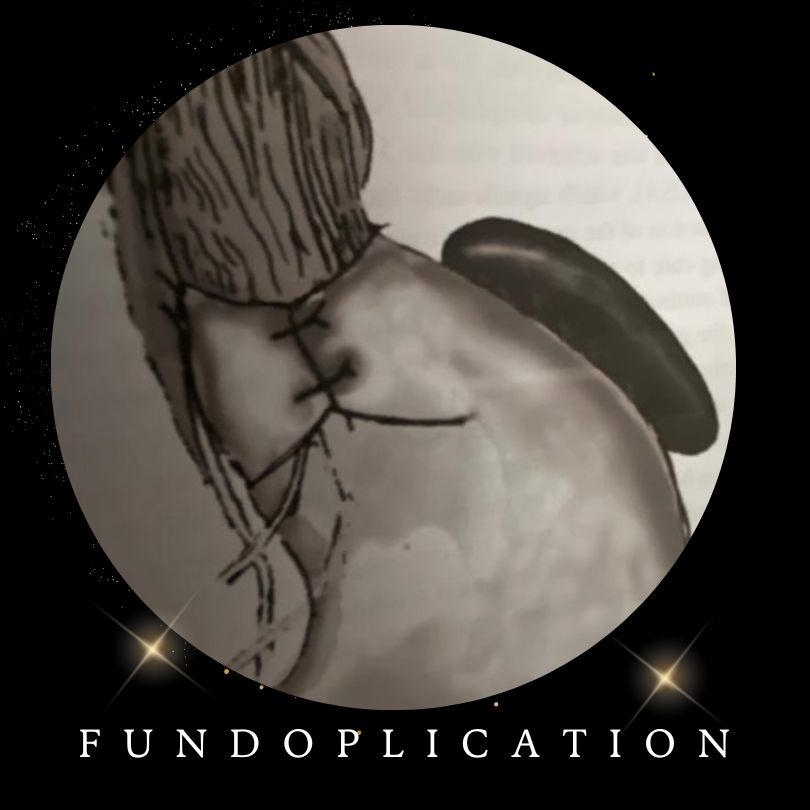
Basically, Laparoscopic fundoplication reinforces the Lower Esophageal Sphincter (LES) which gets impaired in GERD.
Basically, pH means Potential of Hydrogen ions (H+). More H+ ions, more acidic is the substance.
The main objective of this review article delves into the role of 24 - hour pH monitoring in evaluating the efficacy of laparoscopic Fundoplication both pre and post -surgery for GERD patients through extensive analysis of 35 relevant studies. The literature search encompassed diverse databases, inclusions/exclusions criteria and methodological rigor. The methodological review highlights several critical findings. Pre- fundoplication 24- hour pH monitoring not only establishes a baseline for Acid Exposure (pH <4) in GERD, it also helps patient’s selection, ensuring tailored surgical intervention. The comprehensive examination of these studies revealed significant trends in pH monitoring outcomes. The post-fundoplication 24-hour pH monitoring serves as an invaluable tool for evaluating the effectiveness of the procedure, providing insights into changes in Acid Exposure Time (AET), De Meester Score (DMS) and amelioration of symptoms of GERD. Preoperatively GERD patient exhibited abnormal acid (pH<4) reflux parameters and high DMS (>14.7) that often normalized following laparoscopic fundoplication. Post – fundoplication surgery this procedure demonstrated substantial reduction in esophageal acid exposure time (AET)and reduction of De Meester Score (DMS) and better symptom relief. After searching through various relevant. literatures e.g. Pub Med, Google Scholar, Google Search, Laparoscopic and Gastroenterology Journals, SAGE publications, The British Journal of Surgery and The American Journal of surgery, there were significant facts that came to light i.e. variations in pH level, the impact of pH monitoring, a treatment decision or comparative effectiveness of different methods. These findings have major clinical implications, throwing light on the best approach to pH monitoring in pre and post -operative fundoplication of GERD patients.
These findings underline the importance of pH monitoring in patient selection and surgical decision making i.e. whether to opt for laparoscopic Nissen fundoplication, Toupet or Partial fundoplication and post-operative assessment. They contribute to the ongoing conversation surrounding the optimal utilization of laparoscopic fundoplication as a viable treatment for GERD.
This review enhances our understanding of the usefulness of 24 -hour pH monitoring in the management of GERD and offers valuable insights for clinicians, researchers and patients.
It has been established among surgical and gastroenterologist professionals, that 24 -hour pH monitoring is the Gold Standard as a diagnostic tool to detect abnormal pathological acid reflux (pH <4). In GERD the clinical presentation may constitute a myriad of symptoms which may mimic other esophageal and extra esophageal diseases. Therefore, GERD diagnosis by symptoms only may be inaccurate. Endoscopy and Barium meal may be misleading. As there is not a single tool to precisely diagnose GERD in all its variances, the 24-hour pH monitoring analyzed in conjunction with the De MEESTER Score (DMS), is still a reliable method for scientific purposes as well as for clinical decision making.
The implications of this review after searching various relevant literatures are profound, emphasizing the pivotal role of 24- hour pH monitoring in the personalized management of GERD patients. The findings of this review article underpin the optimization of clinical practice, offering insights that improves outcomes and enhances quality of life for GERD patients. This review article also identifies gaps in various unanswered facts in searched literatures, emphasizing the need for further research regarding diagnosis, investigation and optimal treatment for patients.
24-hour pH monitoring and esophageal manometry are the most reliable methods for revealing the level of functional modification established by anti- reflux surgery and makes clinical decision objectively to select appropriate patients of GERD. There are another two types of devices for pH monitoring i.e. Multichannel Intra luminal Impedance pH (MII-pH) and wireless pH monitoring (Bravo) technology however, they are extremely expensive. Typical 24-hour pH monitoring is the most effective and cost-effective tool to diagnose acid reflux and at present.
According to the searched articles it has been accepted by laparoscopic surgeons and gastroenterologists who have vast experience in treating GERD patients that laparoscopic Fundoplication is the most effective treatment to cure GERD when medical therapy fails. It is a widely held belief by majority of laparoscopic surgeons who have wealth of experience after following patients for 22 years Nissen fundoplication is the Gold Standard as an anti- reflux surgery for GERD. These surgeons have followed substantial numbers of patients of GERD after laparoscopic fundoplication. There is consistent improvement of pH level and symptom relief (Visick score 1 or 2). There are gaps and variations which are discussed in subsequent section of this review article.
There is need for further research in non - invasive and cost- effective Wireless pH monitoring also laparoscopic or robotic anti reflux surgery for GERD. In Conclusion, the integration of 24-hour pH monitoring as an adjunct essential to laparoscopic fundoplication illustrates a promising avenue for improving patient outcomes and optimizing the surgical approach. Future research should explore innovative technologies and procedure to further refine this approach. This Abstract provides a clear and succinct summary of this review highlighting the key findings and their relevance. This review article not only consolidates the current understanding of 24-hour pH monitoring in the context of laparoscopic fundoplication also recommends areas requiring further investigation and methodological refinements to advance this crucial aspect of Gastro Esophageal Reflux Disease (GERD) management.
INTRODUCTION:
Gastroesophageal Reflux Disease (GERD) is a global problem, stands as one of the most prevalent and challenging upper gastrointestinal disorders affecting millions of individuals worldwide. The incidence of GERD in the worldwide population is about 14%. In the USA between 25-30% of population suffer from GERD. It can cause considerable morbidity and mortality. The Gastroesophageal reflux disease (GERD)is a chronic backflow of stomach acid into the esophagus leading to range of distressing symptoms and complications (MONTREAL CONSENSUS 2006). In the pursuit of effective therapeutic interventions, the laparoscopic fundoplication has emerged as a prominent surgical solution for GERD aiming to alleviate symptoms and halt the progression of this chronic condition.
The success of laparoscopic fundoplication hinges significantly on the accurate evaluation of GERD not only before the procedure but, also in the critical post-operative phase. It is in this realm that 24 hour- pH monitoring ,a diagnostic modality that quantifies esophageal acid exposure plays an indispensable role .By providing a quantitative assessment of acid reflux (pH<4),this monitoring method enables clinicians to establish an objective diagnosis and patient selection ,ensuring that right candidates are chosen for the surgery.24 hour pH monitoring has emerged as the main pillar , the Gold Standard in the evaluation of the GERD.
By providing a detailed analysis of esophageal pH levels for 24 hours, this diagnostic technique offers critical insights into the frequency and duration of acid exposure time (AET) enabling both accurate diagnosis and informed treatment decisions. The pH level in lower esophagus less than 4(pH<4) is indicative of pathological acid reflux.
To gain a comprehensive understanding of the intricate interplay between 24- hour pH monitoring and laparoscopic fundoplication this review article rigorously and meticulously analyzed selected literature sources. The objective of this review is to gather findings from the existing body of knowledge and to provide an up to date and comprehensive evaluation of the role of 24 -hour pH monitoring in the context of pre and post laparoscopic fundoplication of GERD. This review strives to provide comprehensive understanding of the utility and effectiveness of laparoscopic fundoplication in ameliorating GERD symptoms.
The objective of this review article is to comprehensibly assess the role of 24 -hour pH monitoring in the context of pre and post laparoscopic fundoplication for GERD.
This review aspires to bridge the present knowledge gap by critically evaluating the existing literatures on 24- hour pH monitoring pre and post laparoscopic fundoplication. The present review will traverse the essential phases of GERD management, scrutinizing the diagnostic significance of preoperative 24- hour pH monitoring, the effectiveness of laparoscopic fundoplication and the evolving fields of pH monitoring techniques. For this reason, it aims to furnish clinicians and researchers with a nuanced perspective on the evaluation and management of GERD and the evolving techniques rendered to enhance the diagnostic capabilities. The laparoscopic fundoplication (LFP) is a minimally invasive surgical procedure seeking to alleviate symptoms and reduce the reliance on long term medication i.e. Proton Pump Inhibitor (PPI), H2 antagonist. While the laparoscopic fundoplication has become popular, a comprehensive review of its outcomes, remain unfulfilled need in this review. This review article embarks on a comprehensive exploration of a multifaceted role of 24 -hour pH monitoring in the assessment of GERD, before and after laparoscopic fundoplication. The foundation of this analysis lies in the meticulous scrutiny of an extensive corpus of literature, comprising 35 pertinent studies chosen for their diverse methodological approaches and diverse profiles of the patients they encompass.
The rationale approach in an era where evidence-based medicine is paramount and comprehensive understanding of preoperative and postoperative 24-hour pH monitoring is pivotal. The selection of the most suitable candidate for this intervention and the evaluation of its efficiency postoperatively represent key challenges in clinical practice. Within the arsenal of the therapeutic interventions the laparoscopic fundoplication has emerged as the cornerstone in the management of GERD, offering respite to patients grappling with debilitating symptoms and complications. The procedure’s ability to restore normalcy to esophageal function, underscores its significance in the realm of surgical intervention. The optimization of patients’ care in Gastroesophageal Reflux Disease (GERD) and continued refinement of surgical interventions and the ability to identify the most suitable candidate for these procedures. The use of 24 -hour pH monitoring a diagnostic modality that allows for the precise quantification of acid reflux episodes forms as indispensable component in this intricate riddle. It is an established fact in laparoscopic surgical field, the 24 -hour pH monitoring has become the invaluable tool for objectively evaluating the success of the procedure, often heralding the normalization of acid reflux parameters. The choice of fundoplication technique, the anticipation of complications and the predictability of outcomes are intricately linked to nuanced insights that 24-hour pH monitoring provides.
As such this review aspires to equip healthcare practitioners, researchers and patients with profound understanding of the indispensable role of 24 -hour pH monitoring holds within the context of laparoscopic fundoplication. Drawing from a pool of 35 literature sources, main objective is to synthesize the available evidence and insights, providing a comprehensive analysis of the current state of knowledge in this dynamic field. In the subsequent sections, extensive data extracted from 35 chosen studies will be analyzed exploring the distinct tapestry of preoperative and postoperative pH monitoring in GERD management. By dissecting the trends, drawing parallels and highlighting disparities in the existing literature, the aim is to illuminate various dimensions of this crucial diagnostic tool. The review article also strives to explore and identify areas where further research is warranted.
The comprehensive review article aims to serve as an invaluable resource in the relentless quest to elevate the quality of care dispensed to GERD patients. It offers clinicians a multidimensional perspective, researchers fresh avenues for exploration, a holistic view of the diagnostic perplexity in GERD management. As we traverse the terrain of pre and post laparoscopic fundoplication, the main objective is to deliver an in-depth analysis that underscores the evolving and indispensable role of pH monitoring, fostering a profound appreciation for its clinical significance. Nonetheless, the field of 24-hour pH monitoring in GERD management is not without nuances and complexity. The advent of Impedance multichannel intraluminal pH monitoring (MII-pH monitoring) has introduced new diagnostic dimensions and choice of pH monitoring techniques.
Though laparoscopic fundoplication is an accepted treatment for GERD. However, few articles published reveal failure rate from laparoscopic fundoplication ranges from 10 to 20 % of which 3-6% patients will require revisional surgery, carries greater technical challenges also results in higher complications rate ranging from o to 44 % also higher mortality. Knowing the risk associated with laparoscopic revisional fundoplication, it is imperative to select the right candidate for a primary laparoscopic fundoplication. The 24 -hour pH monitoring device in the lower esophagus, can record continuously, pH for a 24-hour period before and after laparoscopic fundoplication, also analyzed Acid Exposure.
Time (AET), DeMeester score (DMS) and effectiveness of surgical intervention. The 24-hour pH monitoring can provide comprehensive report of recorded data including any improvement or complications observed. Based on the results healthcare team can make a clinical decision on post- operative management including any additional intervention if necessary.
This review not only aims to synthesize the collective evidence from diverse studies but also strives to offer insights into methodological disparities across the literature, thereby elucidating potential sources of variations in reported outcomes. By critically appraising the strength, limitations and clinical implications of the existing body of research, this review attempts to contribute to the refinement of clinical decision making in managing GERD.
This introduction aspires to provide the importance of 24 -hour pH monitoring and laparoscopic fundoplication.
MATERIALS:
This review compiled data from a diverse set of studies extracted from a diverse set of literature extracted from 35 surgical and gastroenterology journals last 32 years. These sources encompassed articles published in various well-known peer review journals representing the collective knowledge derived from multiple clinical and academic settings. Most of the studies reveal pH monitoring were performed in hospital setting.
The inclusion of studies in this review was guided by predefined criteria. Articles were considered eligible which are focused on the role of 24-hour pH monitoring in GERD patients both before and after undergoing laparoscopic fundoplication. These criteria were carefully chosen to ensure inclusion of studies that provided suitable for clinical application also for laparoscopic fundoplication for GERD management.
These selected 35 articles featured diverse characteristics reflecting the breath of research in the field of GERD management. These characteristics included publication year, study design, ranging from case reports to randomized control trials, sample sizes that vary from small cohorts to large scale studies and demographics of patient population all age group under investigation.
Furthermore, the selective studies represent a range of geographical regions, adding to the breadth and diversity of the data reviewed. GERD patients were followed up from 6 weeks to 20 years after laparoscopic fundoplication. Preoperatively all patients had 24 -hour pH monitoring and DMS Score, results were noted, postoperative outcomes were assessed by pH monitoring, DM Score for symptom control. There are mainly three types of pH monitoring devices to measure acid (pH) in lower esophagus. Most commonly used is Ambulatory pH monitoring which provides continuous pH monitoring over a period of 24 hours. allowing for a comprehensive assessment of acid reflux patterns. It can monitor data during various daily activities, meals and sleep. It is an invasive procedure involving insertion of nasogastric tube which can be uncomfortable for the patient and may impact daily activities. Despite a few drawbacks, this device for pH monitoring is mostly used and it is also cost effective. In few cases multichannel intraluminal pH monitor (MII-pH) devices were used, which is also an invasive procedure, inserting a nasogastric tube. It can detect acid reflux and non- acid reflux both in lower esophagus for 48 hours. In one case study Wireless esophageal pH monitoring (Bravo pH system) was used, which is non-invasive. It provides an accurate data of acid (pH) in lower esophagus without the discomfort of a patient not having a nasal catheter. The capsule contains a tiny battery with acid (pH)sensor and transmitter.
The data extracted from these selected studies included the methods employed for 24 -hour pH monitoring, the specifics metrics used for the assessment of acid reflux e.g. De Meester Score (DMS), Acid Exposure Time (AET)and key findings from both the pre and postoperative phases. The data extraction process was systematic, focused on to obtain the essential information that contributed to a comprehensive understanding of the role of laparoscopic fundoplication in GERD management. By collecting data from a vast array of surgical and gastroenterology journals, this review was able to provide a comprehensive spectrum of characteristic findings, offering clinicians and surgeons a representative overview of the literatures in this field.
METHODS:
An archive of systematic and comprehensive literature review was conducted across a range of surgical and gastroenterological journals and database including PubMed, MEDLINE, Google scholar, Surgical journals and gastroenterology journals. The search strategy incorporated a set of targeted keywords such as ‘24 -hour pH monitoring ‘Laparoscopic Fundoplication’ ‘GERD’ and relevant synonyms. No data restrictions were applied during this search to ensure the inclusion of relevant studies from different times.
In accordance with the objective of this review. specific inclusion and exclusion criteria were established. Articles mainly focused on 24-hour pH monitoring before and after fundoplication for GERD management, though few articles were reviewed about other devices for pH monitoring e.g. Multichannel Intraluminal Impedance pH monitor (MII-pH), Wireless pH monitor (Bravo) The exclusion criteria consisted of studies lacking relevant data, non -peer reviewed sources and those not published in English. The search process aimed to retrieve articles reflecting wide spectrum of patient population, all age group from children to adults, all gender male female, variable BMI group normal weight, overweight, obese, study designs and pH monitoring protocols to offer comprehensive perspective.
The initial search yielded a substantial number of articles. Duplicates were first removed and titles, abstracts were reviewed to assess the relevance. The full text of the remaining articles was scrutinized to ensure they met the predefined inclusion criteria. Though this process a total of 35 articles from surgical and gastrointestinal journals were selected for detail analysis. Data extraction has been meticulous and systematic procedure. Information from the selected articles were recorded. Information from the selected articles were recorded including publication details e.g. title, author, journal, publication year, study characteristic e.g. study design, sample size, patient demographics and specifics related to methods and findings of 24-hour pH monitoring. The extracted data was compiled in a structured format to facilitate subsequent analysis.
According to published literatures 35 reviewed approximately, there are three types of known pH monitoring devices available in the market e.g. Firstly, there is the Ambulatory 24-hour pH monitoring device which is the most common and is cost effective. Secondly the Multi channel Intraluminal Impedance pH monitor (MII-Ph). And thirdly, Wireless capsule technology (Bravo). In ambulatory 24-hour pH monitoring and MII-pH system, a nasogastric catheter is inserted 5 cm above the lower esophageal sphincter. MII-pH is inserted into the lower esophagus for 48 hours. This device can detect acidic and non- acidic reflux. Both are invasive procedures.
Wireless capsule technology is non- invasive. The wireless capsule adheres to the esophageal mucosal wall and transmits data to a recorder worn by the patient. The Wireless device can monitor acidic reflux for 96 hours. Fasting is recommended for the patient undergoing pH monitoring before and after laparoscopic fundoplication. Ambulatory 24 -hour pH monitoring is widely used, the most reliable, and cost effective. It provides quantitative data on esophageal Acid Exposure episodes and on temporal correlate between patient’s symptoms and a reflux event. To analyze the results of pH monitoring correctly, it is recommended to interpret in order i.e. Firstly, visual inspection, then computer calculation and then symptom correlation.
4-6 hours of fasting is recommended before pH monitoring to ensure the accuracy of the results because the presence of food in the stomach can affect the acidity of gastric contents.
After laparoscopic fundoplication, the fasting requirement still applicable for pH monitoring particularly if the procedure aims to assess the effectiveness of the surgery. A fasting period allows for the assessment of acid reflux in a controlled and consistent manner.
It is vitally important for patients to follow the specific fasting instructions provided by health care provider where pH monitoring is being performed. Patient should also communicate any concerns or question about fasting requirements to their health care team to ensure that the pH monitoring is conducted accurately and effectively.
Proton Pump Inhibitor (PPI), H2 antagonist antacids should be stopped week before pH monitoring procedure.
The data has been extracted after searching through 35 articles. There are commonly three types of Laparoscopic Fundoplication presently performed for GERD i.e. Laparoscopic Nissen fundoplication (360-degree wrap), Laparoscopic Toupet fundoplication (270-degree wrap) and Laparoscopic Partial fundoplication. Nissen fundoplication is the most commonly performed surgical procedure worldwide for GERD patients.
The main objective of Laparoscopic Fundoplication is to reinforce Lower Esophageal Sphincter (LES) which becomes impaired in Gastroesophageal Reflux Disease (GERD).
By following this methodology, the review sought to encompass a diverse and representative set of articles from surgical and gastroenterology journals, ensuring a comprehensive examination of the role of24-hour pH monitoring in context of laparoscopic fundoplication for GERD management.
In summary, while the reviewed literatures collectively provide valuable insights into the use of 24-hour pH monitoring in GERD management, a comprehensive quality assessment of the methods reveal variations in pH monitoring protocols, adherence to criteria e.g. DeMeester Score (DMS) which quantifies acid exposure, incorporated contemporary pH monitoring i.e. Wireless capsule pH monitoring (Bravo), Patients’ experiences and demographic considerations.
These findings underscore the need for standardization, patient centric approaches and greater attention to validation in future research with aim of enhancing the accuracy and clinical applicability of pH monitoring in the context of GERD and laparoscopic fundoplication. The inclusion of contemporary pH monitoring technology such as Wireless capsule may have implication for the future direction of pH monitoring in GERD research.
RESULTS:
The collective analysis of 35 literatures from various surgical and gastroenterology journals revealed a wide spectrum of findings, related to preoperative 24- hour pH monitoring in patients with Gastroesophageal Reflux Disease (GERD). Notably the preoperative pH monitoring results exhibited substantial heterogeneity across the selected studies. Some patients presented with severe acid reflux (pH<4) as demonstrated by extended period of acidic pH, while others displayed milder degree of acid reflux or non -acidic reflux. The variations in preoperative pH monitoring findings highlights the individualized nature of GERD where patients exhibit distinct profiles of acid reflux.
Regarding Preoperative pH monitoring findings, most of the reviewed literatures collectively highlight the pivotal role of 24-hour pH monitoring before laparoscopic fundoplication to confirm the diagnosis of GERD and assess the severity of acid reflux. This information is paramount important to decide whether laparoscopic fundoplication is appropriate, it provides a baseline measurement of acid exposure into the lower esophagus.
According to 35 published articles which were reviewed, most centres performed 24-hour pH monitoring before and after laparoscopic fundoplication.
MII-pH monitoring was performed at 13 centres . One centre Wireless pH monitoring was carried out. At all centres, the results were consistent regarding acid reflux in the preoperative phase, pH below 4(pH<4) and De Meester score was more than 14.7 confirming the diagnosis of GERD.
In contrast, the postoperative pH monitoring outcome consistently demonstrated a reduction in Acid Exposure Time (AET) and the number of reflux episodes, DMS score was less than 14.7 after laparoscopic fundoplication. Most of the selected studies reported a significant decrease in acid reflux parameters (pH<4) after laparoscopic fundoplication. This collective evidence indicates that laparoscopic fundoplication is generally effective in controlling acid reflux, as has been proved by significant improvements in postoperative pH monitoring results (pH>4), DMS less than14.7. Majority of clinicians and surgeons agree patient with GERD symptoms who have esophagitis on endoscopy (OGD)and good response to PPI do not need preoperative pH monitoring. It has been proved abnormal acid exposure for longer time ( >5 mnts)an independent predictor of good outcome following anti reflux surgery. Majority of clinicians recommend, the patients with GERD symptoms but no endoscopic esophagitis and good response to PPI should undergo preoperative 24-hour pH monitoring also patients with symptoms potentially due to acid reflux who fail to respond to high dose of PPI should have 24-hour pH monitoring before laparoscopic fundoplication for GERD. The poor response is an independent predictor of worse outcomes following anti-reflux surgery. There is not a single instrument to precisely diagnose GERD in all its variance but, pH monitoring analyzed at the light of De Meester Score (DMS) is a reliable method for scientific purposes as well as for clinical decision making. Further examination of included studies allowed for a comparative analysis pre vs post -operative pH monitoring metrics. This comparative analysis highlighted the substantial improvements in acid reflux as measured by pH and DMS Score following laparoscopic fundoplication. The degree of reduction in Acid Exposure Time (AET) and the number of reflux episodes varied among studies but consistently demonstrated postoperative improvements. These results support the notion that laparoscopic fundoplication leads to a substantial reduction in acid reflux in majority of GERD patients. Multiple studies demonstrated consistently better outcomes after laparoscopic fundoplication. i.e. symptom control, acid reflux as measured by 24-hour pH monitoring also by endoscopy OGD), which showed improvement in healing of mucosal damage in esophagitis due to acid reflux. Laparoscopic Fundoplication not only reduced acid reflux but it also improved esophageal motility postoperatively. The esophageal motility is impaired by severe acid reflux exposed for prolonged period as detected by esophageal manometry.
There are few examples from 35 reviewed literatures as a comparative analysis:
PPI Vs Laparoscopic Fundoplication for GERD patients:
Laparoscopic fundoplication has better outcomes e.g. symptom control, acid reflux as opposed to PPI. Pessaux et al (2005), followed up 1340 patients for 5 years after fundoplication. He came to the conclusion that laparoscopic fundoplication has a better outcome than PPI. Dallemagne (2006) had similar findings as Pessaux. He followed up 100 patients for 10 years. Other authors like Maine (2006), Zhang (2015) and Isalauri (1997) had similar result. He followed up 105 patients for 10 years after surgery. All these surgeons concluded Laparoscopic fundoplication has a better outcome than PPI. Various authors have published papers on 24-hour pH monitoring device, discussing its usefulness as a diagnostic tool for GERD patients, to detect acid reflux pre and post laparoscopic fundoplication. Most clinicians concluded Ambulatory 24-hour pH monitoring proved to be the most sensitive and specific diagnostic test. 24-hour pH monitoring device measures increased esophageal exposure to gastric juice by detecting concentration of Hydrogen ions (pH<4) in the distal esophagus. 24-hour pH monitoring has utmost clinical value in detecting pathological reflux in symptomatic patients who had negative endoscopy (Masclee et al 1990). Miguel (1999) Erakin (2022) Chin (2008), Gotley (1996) and Kaspidis (1993) all concluded 24-hour pH monitoring is the most effective and cost-effective in detecting acid reflux in pre and post-operative phase in GERD patients.
24-hour pH monitoring can identify a pattern of abnormal reflux in patients who are at risk of esophageal stricture. In one study (using the wireless pH monitoring device for 48 hours) it was concluded that the Wireless system can detect 22% more patients with abnormal esophageal Acid Exposure in comparison to ambulatory 24-hour pH system (Tseng 2005). Mughal (The British Journal of Surgery 1990) followed up 126 patients with GERD for 8 years after Nissen fundoplication. He came to the conclusion that pH monitoring does not predict of the bad result of Nissen fundoplication. pH monitoring is only needed when diagnosis is in doubt, hence pH monitoring has no value in deciding the suitability of patients. It has been demonstrated conclusively patients with GERD symptoms with normal 24-hour pH monitoring test, had significantly worse subjective outcome after laparoscopic fundoplication compared with abnormal preoperative pH monitoring test. It has been recommended to minimize poor symptomatic outcome after laparoscopic ante reflux surgery to perform routine 24-hour pH monitoring testing. Numerous surgeons have compared laparoscopic Nissen fundoplication (360-degree wrap) with laparoscopic Toupet fundoplication (270-degree wrap) and laparoscopic Partial fundoplication. They have reviewed 200 to 820 patients after surgery. Most surgeons have drawn to the
conclusion from their follow up study after surgery the laparoscopic Nissen fundoplication is the most effective anti- reflux surgery in comparison with Toupet or Partial fundoplication in terms of symptom control, reduction of acid reflux was symptom free after surgery Seeras (2022), Marino Murano (2019), Farrell (2000), Booth (2006) and Brumelhof (1990). In one study surgeons followed up patients for 25 years who had laparoscopic fundoplication .They came to the conclusion that the best prediction of having a positive outcome after laparoscopic fundoplication for GERD patients were : male, BMI less than 30,typical reflux symptom responding to PPI or H2 antagonist, ,abnormal acidic reflux (pH<4) as measured by 24 hour pH monitoring and positive symptoms of GERD (Shukla et al 2022). Another study where 155 patients were followed up after anti reflux surgery, the author observed and drawn to conclusion that those patients with suspected GERD, who had no symptoms or atypical symptoms, who had 24-hour pH monitoring performed prior to laparoscopic fundoplication still obtained relatively good results after anti reflux surgery, however these patients’ outcomes were not as good as those patients with typical symptoms during 24-hour pH monitoring. The compiled results indicate the effectiveness of laparoscopic fundoplication in managing GERD by significantly reducing acid reflux, as assessed 24-hour pH monitoring before and after laparoscopic fundoplication. While the pre- operative pH monitoring findings illustrated the heterogeneity of GERD patients’ profiles, the postoperative outcomes consistently demonstrated marked improvements, these results collectively emphasize the role of laparoscopic anti reflux intervention for controlling acid reflux in GERD patients with satisfactory outcome. The variation in pH monitoring protocol suggests the need for standardization. The insights provided contributes to the ongoing dialogue regarding GERD management and offering valuable guidance for clinicians and researchers in the field of gastroesophageal reflux disease.
The results from this comprehensive review, drawn from a wealth of reputable surgical and gastroenterology journals presented holistic view of 24-hour pH monitoring in the context of laparoscopic fundoplication for GERD management. This comprehensive review reinforced the established understanding that laparoscopic fundoplication is effective in controlling acid reflux. The postoperative pH monitoring data consistently demonstrate a significant reduction in acid exposure time and the number of reflux episodes. These findings validate the role of laparoscopic fundoplication as a leading surgical approach for managing GERD. Variability in preoperative pH monitoring findings highlights the individualized nature of GERD. This variability underscores the need for personalized patient selection and tailored approach to GERD management. While most of the literatures reviewed, reported short-term success following laparoscopic fundoplication, the durability and long-term outcome of the procedure remains a subject of interest and requires a broader perspective, encompassing studies with extended follow up periods, to understand the persistence of benefits and potential late complications associated with this procedure.
Variations in methods of pH monitoring across the selected studies can impact data interpretation. Standardization of pH monitoring protocols and the criteria used to define acid reflux should be considered in future research to ensure data consistency. The results of this review underscore the effectiveness of laparoscopic fundoplication in controlling acid reflux in GERD patients. However, the individualized nature of GERD, the variability in preoperative profiles and the need for extended follow up periods are important considerations for future research and clinical practice. Consistency in pH monitoring techniques are essential to enhance the reliability and comparability of results across studies.
DISCUSSION:
The Gastroesophageal Reflux Disease (GERD) is prevalent worldwide, which causes high morbidity and death. The main reason of GERD is the acid reflux (pH<4) into the lower esophagus which can cause severe esophagitis, esophageal ulcer, esophageal stricture, Barrett’s esophagus and adenocarcinoma of the lower esophagus. In addition, GERD can also cause extra esophageal complications e.g. Asthma, chronic cough, laryngopharyngitis and aspiration pneumonia due to abnormal (pathological) acid reflux.
The comprehensive review of 35 relevant literature sources have revealed a multifaceted landscape regarding the impact of laparoscopic fundoplication on 24- hour pH monitoring in Gastroesophageal Reflux Disease (GERD) patients. These findings indicate a wide spectrum of outcomes, ranging from a substantial improvement in pH levels (pH>4) and symptom relief, to less consistent results.
The integration of preoperative and postoperative laparoscopic fundoplication surgery findings of 24-hour pH monitoring, from comprehensive review of numerous literatures provides valuable insights into the dynamics of acid reflux in patients with GERD undergoing laparoscopic fundoplication, which fundamentally augments the competence of Lower Esophageal Sphincter (LES).
The consistent preoperative identification of acid reflux pattern pH less than 4(pH<4) in lower esophagus, longer acid reflux time (AET), frequency of acid reflux, De Meester Score (DMS) more than 14.7 underscores the severity of acid reflux in this patient population of GERD, reinforcing the need for surgical intervention enabling precise selection of suitable patients. Postoperative analysis reveals a promising shift in Acid reflux parameters with a significant reduction in Exposure Time (AET), rise of pH levels, reduction of De Meester Score (DMS) and frequency of reflux episodes.
Essentially the main indications for ambulatory esophageal pH monitoring in suspected GERD are:
1. Patients with symptoms clinically suggestive of acidic gastroesophageal reflux, who fail to respond during high dose therapeutic trial of Proton Pump Inhibitor (PPI)
2. Patients with symptoms clinically suggestive of acidic gastroesophageal reflux without esophagitis or with unsatisfactory response to a high dose of PPI in whom anti-reflux surgery is contemplated and post surgery to evaluate the effectiveness of anti-reflux surgery.
3. Patients with persistent acidic gastroesophageal reflux symptoms despite anti-reflux surgery.
As mentioned previously, pH means Potential of Hydrogen ions (H+), more H+ ions more acidic is the substance. A drop in pH 4 or below (pH<4) is indicative of severe acid reflux(Pathological Reflux).24-hour pH monitoring detects the acid reflux in the lower esophagus and is proved to be the Gold Standard test. Before laparoscopic fundoplication in suspected GERD, 24 hour -pH monitoring provides precise data on acid reflux events. It helps in selecting suitable candidates for surgery, especially classic acid reflux (pH<4). However, it may miss non-acidic reflux events and weakly acidic reflux, potentially excluding some patients who could benefit from laparoscopic fundoplication. Following fundoplication surgery ,24- hour pH monitoring is the main diagnostic test assessing the surgical outcome. It quantifies acid exposure (pH<4) indicating the success of acid suppression. However, it may not capture non -acidic or weak acidic reflux potentially leading to overestimating the procedure’s efficacy in controlling al reflux events. IMPEDANCE(MII-pH) monitoring is also very effective pH monitoring device which can detect acidic non -acidic also weakly acidic reflux events for 48 hours but it is invasive procedure like typical 24- hour pH monitoring system not comfortable for patients having nasogastric canula for 48 hours.
WIRELESS pH monitoring device (BRAVO) can detect acidic reflux for 96 hours but, it is limited in its ability to detect non-acidic reflux. It may not be the best choice for preoperative patient assessment as it could miss relevant reflux events, potentially leading to surgery being overlooked for some patients. Wireless pH device is not as effective to extract accurate data of acid reflux as 24 pH monitoring or MII-pH device pre or post-operatively after laparoscopic fundoplication. It may not be as comprehensive as accurate as other two systems in evaluating the full spectrum of reflux types after fundoplication. Wireless device is also very expensive device very few hospitals have Wireless pH monitoring system. Traditionally the typical 24-hour pH monitoring is a valuable tool postoperatively following anti-reflux surgery for assessing acid reflux control, cost effective as well but, it may miss non-acidic or weakly acidic reflux whereas MII-pH monitoring can detect acidic and non-acidic reflux. The choice of monitoring method should align with the specific needs of patient and goals of the assessment.
According to reviewed literatures the clinical implications of 24 -hour pH monitoring is enormous, providing valuable insights into the realm of patient’s management and optimum care. The clinical implication includes efficacy of laparoscopic anti-reflux surgery. The 24-hour pH monitoring helps to assess the effectiveness of the laparoscopic fundoplication procedure in controlling acid reflux. A successful surgery should demonstrate a reduction in Acid Exposure Time (AET) in the lower esophagus, indicating that procedure is working to prevent reflux. Anti -reflux surgery has better outcomes than PPI medication. There is a marked improvement of symptoms after surgery in GERD patients due to drastic reduction or complete abolition of acid reflux as measured by 24-hour pH monitoring which often correlates with symptomatic improvement, patient experience, relief of heartburn, regurgitation and other GERD symptoms. The long- term outcome following laparoscopic anti reflux can be assessed by 24- hour pH monitoring over the time, can determine the durability of the procedure’s effects. It can provide insights into long term benefits of laparoscopic fundoplication. According to numerous literatures searched most of surgeons agree laparoscopic Nissen fundoplication provides long lasting benefits for GERD patients in relation to symptom control abolishing acid reflux.
24 -hour pH monitoring results can be used to identify suitable candidates for laparoscopic fundoplication surgery. Patient with significant acid reflux (pH<4) documented through pH monitoring are more likely to benefit from the surgical anti reflux procedure.
A comparative analysis of reviewed literatures regarding 24-hour pH monitoring, the results of pre and postoperative laparoscopic fundoplication to ascertain the successful outcome of surgery, evaluation of any complications or adverse effects of the surgical procedures, also assessing the impact of the chosen type of laparoscopic fundoplication e.g. Nissen (360-degree wrap), Toupet (270-degree wrap) or Partial fundoplication. The majority surgeons concluded there is marked reduction of acid reflux and an improvement in pH level, positive impact on quality of life and other parameters after fundoplication surgery for GERD, indicating the laparoscopic fundoplication is successful in managing the reflux condition in GERD patients.
If postoperatively 24- hour pH monitoring reveals persistent acid reflux (pH<4), may prompt adjustments in patient’s management who suffer from GERD. This could involve medication changes or may need revisional anti reflux surgery which can cause high morbidity and high mortality also technically challenging (Shukla et al 2022). 24- hour pH monitoring can reveal complications such as gas bloating or swallowing difficulty that may result from laparoscopic fundoplication surgery. Early detection allows more timely intervention. In one study the clinician concluded that Ambulatory 24 -hour pH monitoring has proved to be the most sensitive and specific diagnostic investigation. It measures increased esophageal exposure to gastric acidic juice by detecting concentration of Hydrogen ions (pH<4) in lower part of esophagus. The exposure is measured in components e.g. frequency of reflux, duration of reflux episodes and accumulated Acid Exposure Time (AET). It correlates with degree of esophageal mucosal damage demonstrated by histology. The comparative score is the most reliable measurement of acid suppression (PPI) or anti reflux surgery.
Most of the studies searched demonstrated convincingly the laparoscopic Nissen fundoplication (360-degree wrap) has the most effective acid reflux control and has better outcome regarding symptom relief in comparison to Toupet (270-degree wrap) or Partial fundoplication as measured by pre and post 24-hour pH monitoring. Post- operative outcome with Laparoscopic Nissen fundoplication and Toupet fundoplication for GERD with esophagitis much superior than PPI medication subjectively and objectively. The comparative rarity of clinical and endoscopic healing in patients treated conservatively indicates the chronic nature of reflux esophagitis. 10 year follow up after laparoscopic fundoplication outcome was exceedingly better than medical therapy i.e. PPI, H2 antagonists. GERD symptoms were eliminated with anti-reflux surgery also no need for medical treatment (Dallemagne 2006). In another study patients with GERD were followed up for 6 years after Laparoscopic Nissen fundoplication and Toupet fundoplication, the result showed after one year of Laparoscopic Toupet fundoplication, more likely return of heartburn than Laparoscopic Nissen fundoplication.
In comparison with laparoscopic Toupet (270-degree wrap) and partial fundoplication the outcome of laparoscopic Nissen fundoplication was much superior. The relief of heartburn and regurgitation with Nissen fundoplication was 80-90% at 10 years follow up, while Toupet and partial fundoplication postoperatively displayed increased number of recurrence reflux episode as directed by 24-hour pH monitoring when compared with laparoscopic Nissen fundoplication (360-degree wrap). Though postoperatively outcome for acid reflux (pH<4) after Nissen fundoplication or Toupet fundoplication in GERD patients much better than laparoscopic Partial fundoplication but, regarding dysmotility outcome there is marked improvement with laparoscopic partial fundoplication than Nissen or Toupet procedure. It has been proved laparoscopic anti-reflux surgery achieves better outcome in Laryngopharyngeal Reflux due to GERD than PPI medication.
Patients with abnormal impedance and increased acid exposure (pH<4) in GERD had significantly better symptom resolution, less dysphagia and less frequent PPI use after ante-reflux surgery compared to patients of GERD with normal pH. In patients having difficulty in swallowing in GERD patients, Partial fundoplication or Toupet procedures are better choice, but they are not so effective to control acid reflux as laparoscopic Nissen fundoplication. Majority of experienced laparoscopic surgeons believe laparoscopic Nissen fundoplication is the Gold Standard for GERD. Laparoscopic Nissen fundoplication is associated with more comprehensive symptom relief especially for severe Gastroesophageal Reflux Disease (GERD) patients. Toupet or partial fundoplication are preferred when to preserve some physiological function of gastroesophageal junction is a priority.
Esophageal pH monitoring is vital tool to assess the effectiveness of fundoplication procedures. It allows the objective measurement of acid exposure (pH<4) in lower esophagus. 24-hour pH monitoring device can be used to evaluate the impact of different types of fundoplication procedures on pH level, helping to ascertain which procedure is the most effective in controlling acid reflux. pH monitoring is a type of sensor which can measure pH level in lower esophagus continuously for 24 hours, for extended period Impedance MII-pH monitor for 48 hours or Wireless pH monitoring device for 96 hours are preferred.
24-hour pH monitoring along with symptom evaluation of GERD, plays a vital role in guiding clinicians and surgeons the treatment decisions and assessing post -operative outcome. The consistencies and variations in pH monitoring results before and after laparoscopic fundoplication can provide important insights into the effectiveness of anti-reflux surgery. According to reviewed literatures there is consistent theme that most cases of GERD patients there is high acid exposure (pH<4) into lower esophagus.
The key objective of laparoscopic fundoplication surgery is to prevent acid exposure (pH<4) Into the lower esophagus by reinforcing the Lower Esophageal Sphincter (LES). It has been proved beyond doubt by expert in laparoscopic fundoplication surgeons that there definite, substantial decrease in frequency and duration of acid exposure episodes (pH<4) after reflux surgery, indicating the procedure is effectively preventing acid from stomach flowing into lower esophagus by augmenting Lower Esophageal Sphincter (LES). According to literature published the majority of surgeons believe the laparoscopic Nissen fundoplication achieves more profound reduction of acid (pH<4) reflux compared to Toupet or partial fundoplication Seeras( 2022), Mario Murano(2019), Farrel (2000) ,Booth (2006),Grande (1994), Campos (1919).They followed up patients after surgery for long time ,the duration ranging from 5 to 25 years and number of patients followed up ranging from 30 to 1000. There is variation in reduction of acid reflux in three commonly performed laparoscopic anti-reflux surgery e.g. Nissen, Toupet, Partial fundoplication.
It has been observed patients having GERD symptoms with normal pH monitoring result before surgery have significantly worse subjective outcomes after laparoscopic Nissen fundoplication compared with an abnormal pH test preoperatively. It is recommended to minimize poor symptomatic outcome after anti-reflux surgery to perform routine preoperative 24-hour pH testing.
Patients who have atypical symptom in suspected GERD,24-hour pH monitoring may still obtain good result after laparoscopic fundoplication. These patients with atypical symptom outcome after surgery is not as good as patients who experience typical GERD symptoms e.g. heartburn regurgitation during pH study after surgery (Chin et al 2008). Patients with typical symptoms of GERD with endoscopic positive result of esophagitis may not need 24-hour pH monitoring except for accurate diagnosis. These patients had long term follow up after surgery for 8 years. One study demonstrated Wireless pH monitoring device can detect more than 22 % acid reflux (pH<4) before surgery than typical 24-hour pH monitoring system (Tseng 2005).
24-hour pH monitoring can detect mucosal damage histologically also endoscopic severity of reflux esophagitis. Acid reflux can impair the motility of the esophagus due to prolonged acid exposure as detected by 24- hour pH monitoring. Variations in postoperative symptoms can happen while 24-hour pH monitoring may show residual acid exposure. This variation can exist in the level of symptom relief. Some patients may experience complete symptom free, while others may still have mild symptoms depending on the severity of their condition and type of fundoplication surgery performed.
According to reviewed literatures, those patients who have minimum symptoms or atypical symptoms of GERD, weak acid reflux before surgery, female gender, obese patients BMI more than 35, their outcome after surgery in relation to symptom relief, pH level is not good as patient who had typical GERD symptoms and abnormal acid reflux (pH<4), DMS more than 14.7. Gas related symptoms can vary postoperatively among different types of fundoplication surgery. The laparoscopic Nissen fundoplication can lead to more gas related side effects due to complete 360 degree wrap than Partial fundoplication which may result in fewer gas related symptoms. Most of the studies claim gas related symptoms after laparoscopic Nissen fundoplication is transient lasts 4 to 6 weeks, despite this problem it has been proved beyond doubt the laparoscopic Nissen fundoplication is the most effective in preventing acid reflux than other anti -reflux surgical procedures. pH monitoring reading can vary on types of pH monitoring devices used .24 - hour pH monitoring may not detect acid reflux within 24 hours in some cases as MII- pH and Wireless pH monitoring device. but typical 24 -hour pH monitoring is still the most effective tool to diagnose acid reflux also cost effective.
The wireless pH monitor is non -invasive device can detect acid reflux for up to 96 hours but it is very expensive. The main benefit of Wireless pH monitoring apart from non -invasive can overcome the limitations of De Meester score (DMS). Occasionally pH monitoring on suspected GERD patients can show false positive if they are on PPI or bile reflux, swallowing disorder esophageal achalasia or gastric emptying issues. pH monitoring could be false negative in case of intermittent reflux or weak acidic reflux, stress induced reflux, incomplete testing (short monitoring time) or patient taking PPI during pH monitoring. Positional if patient on upright position while pH monitoring conducted, improper electrode placement. It is important for healthcare provider to be aware of these factors and take them into consideration when interpreting pH monitoring results. Additionally, combining pH monitoring with Impedance device (MII-pH) can help to improve accuracy by detecting non -acidic reflux events and differentiating between liquid and gas reflux. It is of paramount important to interpret pH monitoring results in the context of specific laparoscopic fundoplication surgery. Patient’s pre- operative condition and their individual response to surgery should be considered. Variations can occur due to these factors highlighting the importance of individualized patient’s care and follow up assessment. In one study the multivariate analysis the factors predicting outcomes after laparoscopic Nissen fundoplication surgery were performed.
Data from 199 consecutive patients undergoing laparoscopic Nissen fundoplication. Variables include age, gender, BMI, primary symptoms, clinical response to acid suppression therapy, erosive esophagitis,24-hour esophageal pH score and the percentage of time acidic pH was less than 4(pH<4) on 24-hour pH monitoring, lower esophageal sphincter competence, status of esophageal body motility, hiatal hernia, gastric carditis, intestinal metaplasia of cardiac epithelium limited to gastroesophageal junction and Barrett’s esophagus of any length. Patients were followed up to 15 months post operatively. It was concluded that 24-hour pH monitoring provides the strongest outcome predictor of laparoscopic Nissen fundoplication and the outcome is based more on the correct identification of the disease than its severity. Though endoscopy (OGD)is an essential investigation in GERD but, in many cases, endoscopy may be negative but pathological acid reflux(pH<4) may be detected in lower esophagus.
Following 24-hour pH monitoring before and after laparoscopic fundoplication it is recommended that interpretation should be done by specialist either surgeon with expertise in gastroesophageal reflux disease or experienced gastroenterologist regarding result of 24 pH monitoring test. They can provide a detailed analysis and recommendation based on these findings.
Treatment decisions should be individualized based on the patient’s specific condition, symptoms and 24-hour pH monitoring results, the type of laparoscopic fundoplication i.e., Nissen, Toupet or Partial fundoplication. Clinicians should provide patients with clear explanation of 24-hour pH monitoring results including the improvements gained after surgery and variations also discuss realistic expectations for symptom relief. Depending on the postoperative 24-hour pH monitoring result, medication management may be modified, some patients may need ongoing acid suppressive medication e.g. PPI or H2antagonist even after surgery for GERD.
Symptom relief can be correlated with pH monitoring results, higher the pH level (pH>4) better the symptom relief. If there is disassociation between pH outcome and symptom then further evaluation is necessary. Clinicians should engage in shared decision making with patients regarding their ongoing care, to ensure they are actively involved in treatment choices and fully understand the implications of pH monitoring.
Ultimately 24hour pH monitoring is available diagnostic tool for evaluating the success of laparoscopic fundoplication. Future research in the areas of 24-hour pH monitoring and laparoscopic fundoplication can contribute to enhance the diagnosis and treatment of Gastroesophageal Reflux Disease (GERD) and related conditions. Hopefully potential research in future may comprise of, enhancing surgical techniques, individualized treatment options e.g. research on anatomical variation or genetic predispositions may influence the choice of laparoscopic fundoplication and predictive outcome, long-term results to assess the durability of laparoscopic fundoplication, long-lasting symptom relief and acid control. To develop patient selection criteria for laparoscopic fundoplication considering factors such as pH monitoring results, symptom severity and response to medication.
Future research should include the role of ancillary testing to explore the value of combining pH monitoring with other diagnostic test such as high-resolution manometry, Impedance pH testing or novel biomarkers to augment GERD diagnosis and treatment planning.
For children with GERD, use of pH monitoring and laparoscopic fundoplication newer approach should be considered. Scientists should explore potential new technologies for example Wireless pH testing device or smart implants to enhance the accuracy and patient’s experience of pH monitoring. Research should also include the role of monitoring in early detection and prevention of complications associated with long term acid exposure (pH<4) such as Barrett’s esophagus or esophageal adenocarcinoma. Future research will lead to advancement of diagnosis, treatment and management of GERD and related conditions ensuring that patients receive the most appropriate treatment with minimal risk.
New alternative techniques such as Incisionless Transoral Endoscopic Fundoplication have been tried but long-term outcome is not validated. The main advantage of this procedure is no external incision, shorter recovery time, reduced risk of complications e.g., infection and incision related issues also less impact on swallowing function. This technique is contraindicated in Barrett’s esophagus, Scleroderma or extraesophageal or atypical symptoms of GERD. It is not suitable for all patients, may not be as effective for severe GERD cases.
In few centers Magnetic Sphincter Augmentation (LINX) device have been tried. This device enhances the pressure of lower esophageal sphincter (LES) with made of chain of earth magnets. This device exerts ample pressure on lower esophageal sphincter (LES) but, does not obstruct passage of food with swallowing. It does not alter anatomy of the stomach. This procedure is useful for some patients with mild to moderate GERD. There is limited data on long term efficacy. It is not suitable for severe cases of GERD. It may cause dysphagia and gas bloating in some cases.
Robotic assisted fundoplication has been performed in some centers. It is precise and dexterous, good for complex cases especially complicated anatomy or severe GERD, but it is expensive, longer operative time not available in all hospitals. This technique is still in early phase, hence long-term efficacy is not substantiated.
Personalized care for GERD patient involving 24-hour pH monitoring and laparoscopic fundoplication is of paramount importance to optimize treatment outcomes i.e. preoperative evaluation of pH monitoring, symptom assessment, medical history, choosing the right anti-reflux surgical procedures e.g. Laparoscopic Nissen fundoplication, Toupet or Partial fundoplication.
The most important step is shared decision making with patients of GERD.
In summary, the findings from this review underscores the vital role of 24-hour pH monitoring in pre and post laparoscopic fundoplication for GERD. These findings not only reaffirm its significance in clinical practice but also the highlights the evolving field of pH monitoring technique. The findings from reviewed literatures will undoubtedly contribute to informed decision making and improved patient’s care in the realm of laparoscopic fundoplication of Gastroesophageal Reflux Disease (GERD).
CONCLUSION:
The Gastroesophageal Reflux Disease (GERD) affecting people worldwide can cause considerable morbidity and mortality due to acid reflux (pH<4) into the esophagus from stomach (Montreal Consensus 2006). This comprehensive review of 24
World Laparoscopic Hospital Delhi INDIA
ABSTRACT:
Gastroesophageal Reflux Disease (GERD) remains a prevalent and challenging condition affecting millions of people worldwide. This review article offers a comprehensive synthesis of numerous literature sources. The existing body of research published regarding the role of 24- hour pH monitoring in the assessment of pre and post Laparoscopic Fundoplication, a commonly employed surgical approach for GERD management.
Basically, Laparoscopic fundoplication reinforces the Lower Esophageal Sphincter (LES) which gets impaired in GERD.
Basically, pH means Potential of Hydrogen ions (H+). More H+ ions, more acidic is the substance.
The main objective of this review article delves into the role of 24 - hour pH monitoring in evaluating the efficacy of laparoscopic Fundoplication both pre and post -surgery for GERD patients through extensive analysis of 35 relevant studies. The literature search encompassed diverse databases, inclusions/exclusions criteria and methodological rigor. The methodological review highlights several critical findings. Pre- fundoplication 24- hour pH monitoring not only establishes a baseline for Acid Exposure (pH <4) in GERD, it also helps patient’s selection, ensuring tailored surgical intervention. The comprehensive examination of these studies revealed significant trends in pH monitoring outcomes. The post-fundoplication 24-hour pH monitoring serves as an invaluable tool for evaluating the effectiveness of the procedure, providing insights into changes in Acid Exposure Time (AET), De Meester Score (DMS) and amelioration of symptoms of GERD. Preoperatively GERD patient exhibited abnormal acid (pH<4) reflux parameters and high DMS (>14.7) that often normalized following laparoscopic fundoplication. Post – fundoplication surgery this procedure demonstrated substantial reduction in esophageal acid exposure time (AET)and reduction of De Meester Score (DMS) and better symptom relief. After searching through various relevant. literatures e.g. Pub Med, Google Scholar, Google Search, Laparoscopic and Gastroenterology Journals, SAGE publications, The British Journal of Surgery and The American Journal of surgery, there were significant facts that came to light i.e. variations in pH level, the impact of pH monitoring, a treatment decision or comparative effectiveness of different methods. These findings have major clinical implications, throwing light on the best approach to pH monitoring in pre and post -operative fundoplication of GERD patients.
These findings underline the importance of pH monitoring in patient selection and surgical decision making i.e. whether to opt for laparoscopic Nissen fundoplication, Toupet or Partial fundoplication and post-operative assessment. They contribute to the ongoing conversation surrounding the optimal utilization of laparoscopic fundoplication as a viable treatment for GERD.
This review enhances our understanding of the usefulness of 24 -hour pH monitoring in the management of GERD and offers valuable insights for clinicians, researchers and patients.
It has been established among surgical and gastroenterologist professionals, that 24 -hour pH monitoring is the Gold Standard as a diagnostic tool to detect abnormal pathological acid reflux (pH <4). In GERD the clinical presentation may constitute a myriad of symptoms which may mimic other esophageal and extra esophageal diseases. Therefore, GERD diagnosis by symptoms only may be inaccurate. Endoscopy and Barium meal may be misleading. As there is not a single tool to precisely diagnose GERD in all its variances, the 24-hour pH monitoring analyzed in conjunction with the De MEESTER Score (DMS), is still a reliable method for scientific purposes as well as for clinical decision making.
The implications of this review after searching various relevant literatures are profound, emphasizing the pivotal role of 24- hour pH monitoring in the personalized management of GERD patients. The findings of this review article underpin the optimization of clinical practice, offering insights that improves outcomes and enhances quality of life for GERD patients. This review article also identifies gaps in various unanswered facts in searched literatures, emphasizing the need for further research regarding diagnosis, investigation and optimal treatment for patients.
24-hour pH monitoring and esophageal manometry are the most reliable methods for revealing the level of functional modification established by anti- reflux surgery and makes clinical decision objectively to select appropriate patients of GERD. There are another two types of devices for pH monitoring i.e. Multichannel Intra luminal Impedance pH (MII-pH) and wireless pH monitoring (Bravo) technology however, they are extremely expensive. Typical 24-hour pH monitoring is the most effective and cost-effective tool to diagnose acid reflux and at present.
According to the searched articles it has been accepted by laparoscopic surgeons and gastroenterologists who have vast experience in treating GERD patients that laparoscopic Fundoplication is the most effective treatment to cure GERD when medical therapy fails. It is a widely held belief by majority of laparoscopic surgeons who have wealth of experience after following patients for 22 years Nissen fundoplication is the Gold Standard as an anti- reflux surgery for GERD. These surgeons have followed substantial numbers of patients of GERD after laparoscopic fundoplication. There is consistent improvement of pH level and symptom relief (Visick score 1 or 2). There are gaps and variations which are discussed in subsequent section of this review article.
There is need for further research in non - invasive and cost- effective Wireless pH monitoring also laparoscopic or robotic anti reflux surgery for GERD. In Conclusion, the integration of 24-hour pH monitoring as an adjunct essential to laparoscopic fundoplication illustrates a promising avenue for improving patient outcomes and optimizing the surgical approach. Future research should explore innovative technologies and procedure to further refine this approach. This Abstract provides a clear and succinct summary of this review highlighting the key findings and their relevance. This review article not only consolidates the current understanding of 24-hour pH monitoring in the context of laparoscopic fundoplication also recommends areas requiring further investigation and methodological refinements to advance this crucial aspect of Gastro Esophageal Reflux Disease (GERD) management.
INTRODUCTION:
Gastroesophageal Reflux Disease (GERD) is a global problem, stands as one of the most prevalent and challenging upper gastrointestinal disorders affecting millions of individuals worldwide. The incidence of GERD in the worldwide population is about 14%. In the USA between 25-30% of population suffer from GERD. It can cause considerable morbidity and mortality. The Gastroesophageal reflux disease (GERD)is a chronic backflow of stomach acid into the esophagus leading to range of distressing symptoms and complications (MONTREAL CONSENSUS 2006). In the pursuit of effective therapeutic interventions, the laparoscopic fundoplication has emerged as a prominent surgical solution for GERD aiming to alleviate symptoms and halt the progression of this chronic condition.
The success of laparoscopic fundoplication hinges significantly on the accurate evaluation of GERD not only before the procedure but, also in the critical post-operative phase. It is in this realm that 24 hour- pH monitoring ,a diagnostic modality that quantifies esophageal acid exposure plays an indispensable role .By providing a quantitative assessment of acid reflux (pH<4),this monitoring method enables clinicians to establish an objective diagnosis and patient selection ,ensuring that right candidates are chosen for the surgery.24 hour pH monitoring has emerged as the main pillar , the Gold Standard in the evaluation of the GERD.
By providing a detailed analysis of esophageal pH levels for 24 hours, this diagnostic technique offers critical insights into the frequency and duration of acid exposure time (AET) enabling both accurate diagnosis and informed treatment decisions. The pH level in lower esophagus less than 4(pH<4) is indicative of pathological acid reflux.
To gain a comprehensive understanding of the intricate interplay between 24- hour pH monitoring and laparoscopic fundoplication this review article rigorously and meticulously analyzed selected literature sources. The objective of this review is to gather findings from the existing body of knowledge and to provide an up to date and comprehensive evaluation of the role of 24 -hour pH monitoring in the context of pre and post laparoscopic fundoplication of GERD. This review strives to provide comprehensive understanding of the utility and effectiveness of laparoscopic fundoplication in ameliorating GERD symptoms.
The objective of this review article is to comprehensibly assess the role of 24 -hour pH monitoring in the context of pre and post laparoscopic fundoplication for GERD.
This review aspires to bridge the present knowledge gap by critically evaluating the existing literatures on 24- hour pH monitoring pre and post laparoscopic fundoplication. The present review will traverse the essential phases of GERD management, scrutinizing the diagnostic significance of preoperative 24- hour pH monitoring, the effectiveness of laparoscopic fundoplication and the evolving fields of pH monitoring techniques. For this reason, it aims to furnish clinicians and researchers with a nuanced perspective on the evaluation and management of GERD and the evolving techniques rendered to enhance the diagnostic capabilities. The laparoscopic fundoplication (LFP) is a minimally invasive surgical procedure seeking to alleviate symptoms and reduce the reliance on long term medication i.e. Proton Pump Inhibitor (PPI), H2 antagonist. While the laparoscopic fundoplication has become popular, a comprehensive review of its outcomes, remain unfulfilled need in this review. This review article embarks on a comprehensive exploration of a multifaceted role of 24 -hour pH monitoring in the assessment of GERD, before and after laparoscopic fundoplication. The foundation of this analysis lies in the meticulous scrutiny of an extensive corpus of literature, comprising 35 pertinent studies chosen for their diverse methodological approaches and diverse profiles of the patients they encompass.
The rationale approach in an era where evidence-based medicine is paramount and comprehensive understanding of preoperative and postoperative 24-hour pH monitoring is pivotal. The selection of the most suitable candidate for this intervention and the evaluation of its efficiency postoperatively represent key challenges in clinical practice. Within the arsenal of the therapeutic interventions the laparoscopic fundoplication has emerged as the cornerstone in the management of GERD, offering respite to patients grappling with debilitating symptoms and complications. The procedure’s ability to restore normalcy to esophageal function, underscores its significance in the realm of surgical intervention. The optimization of patients’ care in Gastroesophageal Reflux Disease (GERD) and continued refinement of surgical interventions and the ability to identify the most suitable candidate for these procedures. The use of 24 -hour pH monitoring a diagnostic modality that allows for the precise quantification of acid reflux episodes forms as indispensable component in this intricate riddle. It is an established fact in laparoscopic surgical field, the 24 -hour pH monitoring has become the invaluable tool for objectively evaluating the success of the procedure, often heralding the normalization of acid reflux parameters. The choice of fundoplication technique, the anticipation of complications and the predictability of outcomes are intricately linked to nuanced insights that 24-hour pH monitoring provides.
As such this review aspires to equip healthcare practitioners, researchers and patients with profound understanding of the indispensable role of 24 -hour pH monitoring holds within the context of laparoscopic fundoplication. Drawing from a pool of 35 literature sources, main objective is to synthesize the available evidence and insights, providing a comprehensive analysis of the current state of knowledge in this dynamic field. In the subsequent sections, extensive data extracted from 35 chosen studies will be analyzed exploring the distinct tapestry of preoperative and postoperative pH monitoring in GERD management. By dissecting the trends, drawing parallels and highlighting disparities in the existing literature, the aim is to illuminate various dimensions of this crucial diagnostic tool. The review article also strives to explore and identify areas where further research is warranted.
The comprehensive review article aims to serve as an invaluable resource in the relentless quest to elevate the quality of care dispensed to GERD patients. It offers clinicians a multidimensional perspective, researchers fresh avenues for exploration, a holistic view of the diagnostic perplexity in GERD management. As we traverse the terrain of pre and post laparoscopic fundoplication, the main objective is to deliver an in-depth analysis that underscores the evolving and indispensable role of pH monitoring, fostering a profound appreciation for its clinical significance. Nonetheless, the field of 24-hour pH monitoring in GERD management is not without nuances and complexity. The advent of Impedance multichannel intraluminal pH monitoring (MII-pH monitoring) has introduced new diagnostic dimensions and choice of pH monitoring techniques.
Though laparoscopic fundoplication is an accepted treatment for GERD. However, few articles published reveal failure rate from laparoscopic fundoplication ranges from 10 to 20 % of which 3-6% patients will require revisional surgery, carries greater technical challenges also results in higher complications rate ranging from o to 44 % also higher mortality. Knowing the risk associated with laparoscopic revisional fundoplication, it is imperative to select the right candidate for a primary laparoscopic fundoplication. The 24 -hour pH monitoring device in the lower esophagus, can record continuously, pH for a 24-hour period before and after laparoscopic fundoplication, also analyzed Acid Exposure.
Time (AET), DeMeester score (DMS) and effectiveness of surgical intervention. The 24-hour pH monitoring can provide comprehensive report of recorded data including any improvement or complications observed. Based on the results healthcare team can make a clinical decision on post- operative management including any additional intervention if necessary.
This review not only aims to synthesize the collective evidence from diverse studies but also strives to offer insights into methodological disparities across the literature, thereby elucidating potential sources of variations in reported outcomes. By critically appraising the strength, limitations and clinical implications of the existing body of research, this review attempts to contribute to the refinement of clinical decision making in managing GERD.
This introduction aspires to provide the importance of 24 -hour pH monitoring and laparoscopic fundoplication.
MATERIALS:
This review compiled data from a diverse set of studies extracted from a diverse set of literature extracted from 35 surgical and gastroenterology journals last 32 years. These sources encompassed articles published in various well-known peer review journals representing the collective knowledge derived from multiple clinical and academic settings. Most of the studies reveal pH monitoring were performed in hospital setting.
The inclusion of studies in this review was guided by predefined criteria. Articles were considered eligible which are focused on the role of 24-hour pH monitoring in GERD patients both before and after undergoing laparoscopic fundoplication. These criteria were carefully chosen to ensure inclusion of studies that provided suitable for clinical application also for laparoscopic fundoplication for GERD management.
These selected 35 articles featured diverse characteristics reflecting the breath of research in the field of GERD management. These characteristics included publication year, study design, ranging from case reports to randomized control trials, sample sizes that vary from small cohorts to large scale studies and demographics of patient population all age group under investigation.
Furthermore, the selective studies represent a range of geographical regions, adding to the breadth and diversity of the data reviewed. GERD patients were followed up from 6 weeks to 20 years after laparoscopic fundoplication. Preoperatively all patients had 24 -hour pH monitoring and DMS Score, results were noted, postoperative outcomes were assessed by pH monitoring, DM Score for symptom control. There are mainly three types of pH monitoring devices to measure acid (pH) in lower esophagus. Most commonly used is Ambulatory pH monitoring which provides continuous pH monitoring over a period of 24 hours. allowing for a comprehensive assessment of acid reflux patterns. It can monitor data during various daily activities, meals and sleep. It is an invasive procedure involving insertion of nasogastric tube which can be uncomfortable for the patient and may impact daily activities. Despite a few drawbacks, this device for pH monitoring is mostly used and it is also cost effective. In few cases multichannel intraluminal pH monitor (MII-pH) devices were used, which is also an invasive procedure, inserting a nasogastric tube. It can detect acid reflux and non- acid reflux both in lower esophagus for 48 hours. In one case study Wireless esophageal pH monitoring (Bravo pH system) was used, which is non-invasive. It provides an accurate data of acid (pH) in lower esophagus without the discomfort of a patient not having a nasal catheter. The capsule contains a tiny battery with acid (pH)sensor and transmitter.
The data extracted from these selected studies included the methods employed for 24 -hour pH monitoring, the specifics metrics used for the assessment of acid reflux e.g. De Meester Score (DMS), Acid Exposure Time (AET)and key findings from both the pre and postoperative phases. The data extraction process was systematic, focused on to obtain the essential information that contributed to a comprehensive understanding of the role of laparoscopic fundoplication in GERD management. By collecting data from a vast array of surgical and gastroenterology journals, this review was able to provide a comprehensive spectrum of characteristic findings, offering clinicians and surgeons a representative overview of the literatures in this field.
METHODS:
An archive of systematic and comprehensive literature review was conducted across a range of surgical and gastroenterological journals and database including PubMed, MEDLINE, Google scholar, Surgical journals and gastroenterology journals. The search strategy incorporated a set of targeted keywords such as ‘24 -hour pH monitoring ‘Laparoscopic Fundoplication’ ‘GERD’ and relevant synonyms. No data restrictions were applied during this search to ensure the inclusion of relevant studies from different times.
In accordance with the objective of this review. specific inclusion and exclusion criteria were established. Articles mainly focused on 24-hour pH monitoring before and after fundoplication for GERD management, though few articles were reviewed about other devices for pH monitoring e.g. Multichannel Intraluminal Impedance pH monitor (MII-pH), Wireless pH monitor (Bravo) The exclusion criteria consisted of studies lacking relevant data, non -peer reviewed sources and those not published in English. The search process aimed to retrieve articles reflecting wide spectrum of patient population, all age group from children to adults, all gender male female, variable BMI group normal weight, overweight, obese, study designs and pH monitoring protocols to offer comprehensive perspective.
The initial search yielded a substantial number of articles. Duplicates were first removed and titles, abstracts were reviewed to assess the relevance. The full text of the remaining articles was scrutinized to ensure they met the predefined inclusion criteria. Though this process a total of 35 articles from surgical and gastrointestinal journals were selected for detail analysis. Data extraction has been meticulous and systematic procedure. Information from the selected articles were recorded. Information from the selected articles were recorded including publication details e.g. title, author, journal, publication year, study characteristic e.g. study design, sample size, patient demographics and specifics related to methods and findings of 24-hour pH monitoring. The extracted data was compiled in a structured format to facilitate subsequent analysis.
According to published literatures 35 reviewed approximately, there are three types of known pH monitoring devices available in the market e.g. Firstly, there is the Ambulatory 24-hour pH monitoring device which is the most common and is cost effective. Secondly the Multi channel Intraluminal Impedance pH monitor (MII-Ph). And thirdly, Wireless capsule technology (Bravo). In ambulatory 24-hour pH monitoring and MII-pH system, a nasogastric catheter is inserted 5 cm above the lower esophageal sphincter. MII-pH is inserted into the lower esophagus for 48 hours. This device can detect acidic and non- acidic reflux. Both are invasive procedures.
Wireless capsule technology is non- invasive. The wireless capsule adheres to the esophageal mucosal wall and transmits data to a recorder worn by the patient. The Wireless device can monitor acidic reflux for 96 hours. Fasting is recommended for the patient undergoing pH monitoring before and after laparoscopic fundoplication. Ambulatory 24 -hour pH monitoring is widely used, the most reliable, and cost effective. It provides quantitative data on esophageal Acid Exposure episodes and on temporal correlate between patient’s symptoms and a reflux event. To analyze the results of pH monitoring correctly, it is recommended to interpret in order i.e. Firstly, visual inspection, then computer calculation and then symptom correlation.
4-6 hours of fasting is recommended before pH monitoring to ensure the accuracy of the results because the presence of food in the stomach can affect the acidity of gastric contents.
After laparoscopic fundoplication, the fasting requirement still applicable for pH monitoring particularly if the procedure aims to assess the effectiveness of the surgery. A fasting period allows for the assessment of acid reflux in a controlled and consistent manner.
It is vitally important for patients to follow the specific fasting instructions provided by health care provider where pH monitoring is being performed. Patient should also communicate any concerns or question about fasting requirements to their health care team to ensure that the pH monitoring is conducted accurately and effectively.
Proton Pump Inhibitor (PPI), H2 antagonist antacids should be stopped week before pH monitoring procedure.
The data has been extracted after searching through 35 articles. There are commonly three types of Laparoscopic Fundoplication presently performed for GERD i.e. Laparoscopic Nissen fundoplication (360-degree wrap), Laparoscopic Toupet fundoplication (270-degree wrap) and Laparoscopic Partial fundoplication. Nissen fundoplication is the most commonly performed surgical procedure worldwide for GERD patients.
The main objective of Laparoscopic Fundoplication is to reinforce Lower Esophageal Sphincter (LES) which becomes impaired in Gastroesophageal Reflux Disease (GERD).
By following this methodology, the review sought to encompass a diverse and representative set of articles from surgical and gastroenterology journals, ensuring a comprehensive examination of the role of24-hour pH monitoring in context of laparoscopic fundoplication for GERD management.
In summary, while the reviewed literatures collectively provide valuable insights into the use of 24-hour pH monitoring in GERD management, a comprehensive quality assessment of the methods reveal variations in pH monitoring protocols, adherence to criteria e.g. DeMeester Score (DMS) which quantifies acid exposure, incorporated contemporary pH monitoring i.e. Wireless capsule pH monitoring (Bravo), Patients’ experiences and demographic considerations.
These findings underscore the need for standardization, patient centric approaches and greater attention to validation in future research with aim of enhancing the accuracy and clinical applicability of pH monitoring in the context of GERD and laparoscopic fundoplication. The inclusion of contemporary pH monitoring technology such as Wireless capsule may have implication for the future direction of pH monitoring in GERD research.
RESULTS:
The collective analysis of 35 literatures from various surgical and gastroenterology journals revealed a wide spectrum of findings, related to preoperative 24- hour pH monitoring in patients with Gastroesophageal Reflux Disease (GERD). Notably the preoperative pH monitoring results exhibited substantial heterogeneity across the selected studies. Some patients presented with severe acid reflux (pH<4) as demonstrated by extended period of acidic pH, while others displayed milder degree of acid reflux or non -acidic reflux. The variations in preoperative pH monitoring findings highlights the individualized nature of GERD where patients exhibit distinct profiles of acid reflux.
Regarding Preoperative pH monitoring findings, most of the reviewed literatures collectively highlight the pivotal role of 24-hour pH monitoring before laparoscopic fundoplication to confirm the diagnosis of GERD and assess the severity of acid reflux. This information is paramount important to decide whether laparoscopic fundoplication is appropriate, it provides a baseline measurement of acid exposure into the lower esophagus.
According to 35 published articles which were reviewed, most centres performed 24-hour pH monitoring before and after laparoscopic fundoplication.
MII-pH monitoring was performed at 13 centres . One centre Wireless pH monitoring was carried out. At all centres, the results were consistent regarding acid reflux in the preoperative phase, pH below 4(pH<4) and De Meester score was more than 14.7 confirming the diagnosis of GERD.
In contrast, the postoperative pH monitoring outcome consistently demonstrated a reduction in Acid Exposure Time (AET) and the number of reflux episodes, DMS score was less than 14.7 after laparoscopic fundoplication. Most of the selected studies reported a significant decrease in acid reflux parameters (pH<4) after laparoscopic fundoplication. This collective evidence indicates that laparoscopic fundoplication is generally effective in controlling acid reflux, as has been proved by significant improvements in postoperative pH monitoring results (pH>4), DMS less than14.7. Majority of clinicians and surgeons agree patient with GERD symptoms who have esophagitis on endoscopy (OGD)and good response to PPI do not need preoperative pH monitoring. It has been proved abnormal acid exposure for longer time ( >5 mnts)an independent predictor of good outcome following anti reflux surgery. Majority of clinicians recommend, the patients with GERD symptoms but no endoscopic esophagitis and good response to PPI should undergo preoperative 24-hour pH monitoring also patients with symptoms potentially due to acid reflux who fail to respond to high dose of PPI should have 24-hour pH monitoring before laparoscopic fundoplication for GERD. The poor response is an independent predictor of worse outcomes following anti-reflux surgery. There is not a single instrument to precisely diagnose GERD in all its variance but, pH monitoring analyzed at the light of De Meester Score (DMS) is a reliable method for scientific purposes as well as for clinical decision making. Further examination of included studies allowed for a comparative analysis pre vs post -operative pH monitoring metrics. This comparative analysis highlighted the substantial improvements in acid reflux as measured by pH and DMS Score following laparoscopic fundoplication. The degree of reduction in Acid Exposure Time (AET) and the number of reflux episodes varied among studies but consistently demonstrated postoperative improvements. These results support the notion that laparoscopic fundoplication leads to a substantial reduction in acid reflux in majority of GERD patients. Multiple studies demonstrated consistently better outcomes after laparoscopic fundoplication. i.e. symptom control, acid reflux as measured by 24-hour pH monitoring also by endoscopy OGD), which showed improvement in healing of mucosal damage in esophagitis due to acid reflux. Laparoscopic Fundoplication not only reduced acid reflux but it also improved esophageal motility postoperatively. The esophageal motility is impaired by severe acid reflux exposed for prolonged period as detected by esophageal manometry.
There are few examples from 35 reviewed literatures as a comparative analysis:
PPI Vs Laparoscopic Fundoplication for GERD patients:
Laparoscopic fundoplication has better outcomes e.g. symptom control, acid reflux as opposed to PPI. Pessaux et al (2005), followed up 1340 patients for 5 years after fundoplication. He came to the conclusion that laparoscopic fundoplication has a better outcome than PPI. Dallemagne (2006) had similar findings as Pessaux. He followed up 100 patients for 10 years. Other authors like Maine (2006), Zhang (2015) and Isalauri (1997) had similar result. He followed up 105 patients for 10 years after surgery. All these surgeons concluded Laparoscopic fundoplication has a better outcome than PPI. Various authors have published papers on 24-hour pH monitoring device, discussing its usefulness as a diagnostic tool for GERD patients, to detect acid reflux pre and post laparoscopic fundoplication. Most clinicians concluded Ambulatory 24-hour pH monitoring proved to be the most sensitive and specific diagnostic test. 24-hour pH monitoring device measures increased esophageal exposure to gastric juice by detecting concentration of Hydrogen ions (pH<4) in the distal esophagus. 24-hour pH monitoring has utmost clinical value in detecting pathological reflux in symptomatic patients who had negative endoscopy (Masclee et al 1990). Miguel (1999) Erakin (2022) Chin (2008), Gotley (1996) and Kaspidis (1993) all concluded 24-hour pH monitoring is the most effective and cost-effective in detecting acid reflux in pre and post-operative phase in GERD patients.
24-hour pH monitoring can identify a pattern of abnormal reflux in patients who are at risk of esophageal stricture. In one study (using the wireless pH monitoring device for 48 hours) it was concluded that the Wireless system can detect 22% more patients with abnormal esophageal Acid Exposure in comparison to ambulatory 24-hour pH system (Tseng 2005). Mughal (The British Journal of Surgery 1990) followed up 126 patients with GERD for 8 years after Nissen fundoplication. He came to the conclusion that pH monitoring does not predict of the bad result of Nissen fundoplication. pH monitoring is only needed when diagnosis is in doubt, hence pH monitoring has no value in deciding the suitability of patients. It has been demonstrated conclusively patients with GERD symptoms with normal 24-hour pH monitoring test, had significantly worse subjective outcome after laparoscopic fundoplication compared with abnormal preoperative pH monitoring test. It has been recommended to minimize poor symptomatic outcome after laparoscopic ante reflux surgery to perform routine 24-hour pH monitoring testing. Numerous surgeons have compared laparoscopic Nissen fundoplication (360-degree wrap) with laparoscopic Toupet fundoplication (270-degree wrap) and laparoscopic Partial fundoplication. They have reviewed 200 to 820 patients after surgery. Most surgeons have drawn to the
conclusion from their follow up study after surgery the laparoscopic Nissen fundoplication is the most effective anti- reflux surgery in comparison with Toupet or Partial fundoplication in terms of symptom control, reduction of acid reflux was symptom free after surgery Seeras (2022), Marino Murano (2019), Farrell (2000), Booth (2006) and Brumelhof (1990). In one study surgeons followed up patients for 25 years who had laparoscopic fundoplication .They came to the conclusion that the best prediction of having a positive outcome after laparoscopic fundoplication for GERD patients were : male, BMI less than 30,typical reflux symptom responding to PPI or H2 antagonist, ,abnormal acidic reflux (pH<4) as measured by 24 hour pH monitoring and positive symptoms of GERD (Shukla et al 2022). Another study where 155 patients were followed up after anti reflux surgery, the author observed and drawn to conclusion that those patients with suspected GERD, who had no symptoms or atypical symptoms, who had 24-hour pH monitoring performed prior to laparoscopic fundoplication still obtained relatively good results after anti reflux surgery, however these patients’ outcomes were not as good as those patients with typical symptoms during 24-hour pH monitoring. The compiled results indicate the effectiveness of laparoscopic fundoplication in managing GERD by significantly reducing acid reflux, as assessed 24-hour pH monitoring before and after laparoscopic fundoplication. While the pre- operative pH monitoring findings illustrated the heterogeneity of GERD patients’ profiles, the postoperative outcomes consistently demonstrated marked improvements, these results collectively emphasize the role of laparoscopic anti reflux intervention for controlling acid reflux in GERD patients with satisfactory outcome. The variation in pH monitoring protocol suggests the need for standardization. The insights provided contributes to the ongoing dialogue regarding GERD management and offering valuable guidance for clinicians and researchers in the field of gastroesophageal reflux disease.
The results from this comprehensive review, drawn from a wealth of reputable surgical and gastroenterology journals presented holistic view of 24-hour pH monitoring in the context of laparoscopic fundoplication for GERD management. This comprehensive review reinforced the established understanding that laparoscopic fundoplication is effective in controlling acid reflux. The postoperative pH monitoring data consistently demonstrate a significant reduction in acid exposure time and the number of reflux episodes. These findings validate the role of laparoscopic fundoplication as a leading surgical approach for managing GERD. Variability in preoperative pH monitoring findings highlights the individualized nature of GERD. This variability underscores the need for personalized patient selection and tailored approach to GERD management. While most of the literatures reviewed, reported short-term success following laparoscopic fundoplication, the durability and long-term outcome of the procedure remains a subject of interest and requires a broader perspective, encompassing studies with extended follow up periods, to understand the persistence of benefits and potential late complications associated with this procedure.
Variations in methods of pH monitoring across the selected studies can impact data interpretation. Standardization of pH monitoring protocols and the criteria used to define acid reflux should be considered in future research to ensure data consistency. The results of this review underscore the effectiveness of laparoscopic fundoplication in controlling acid reflux in GERD patients. However, the individualized nature of GERD, the variability in preoperative profiles and the need for extended follow up periods are important considerations for future research and clinical practice. Consistency in pH monitoring techniques are essential to enhance the reliability and comparability of results across studies.
DISCUSSION:
The Gastroesophageal Reflux Disease (GERD) is prevalent worldwide, which causes high morbidity and death. The main reason of GERD is the acid reflux (pH<4) into the lower esophagus which can cause severe esophagitis, esophageal ulcer, esophageal stricture, Barrett’s esophagus and adenocarcinoma of the lower esophagus. In addition, GERD can also cause extra esophageal complications e.g. Asthma, chronic cough, laryngopharyngitis and aspiration pneumonia due to abnormal (pathological) acid reflux.
The comprehensive review of 35 relevant literature sources have revealed a multifaceted landscape regarding the impact of laparoscopic fundoplication on 24- hour pH monitoring in Gastroesophageal Reflux Disease (GERD) patients. These findings indicate a wide spectrum of outcomes, ranging from a substantial improvement in pH levels (pH>4) and symptom relief, to less consistent results.
The integration of preoperative and postoperative laparoscopic fundoplication surgery findings of 24-hour pH monitoring, from comprehensive review of numerous literatures provides valuable insights into the dynamics of acid reflux in patients with GERD undergoing laparoscopic fundoplication, which fundamentally augments the competence of Lower Esophageal Sphincter (LES).
The consistent preoperative identification of acid reflux pattern pH less than 4(pH<4) in lower esophagus, longer acid reflux time (AET), frequency of acid reflux, De Meester Score (DMS) more than 14.7 underscores the severity of acid reflux in this patient population of GERD, reinforcing the need for surgical intervention enabling precise selection of suitable patients. Postoperative analysis reveals a promising shift in Acid reflux parameters with a significant reduction in Exposure Time (AET), rise of pH levels, reduction of De Meester Score (DMS) and frequency of reflux episodes.
Essentially the main indications for ambulatory esophageal pH monitoring in suspected GERD are:
1. Patients with symptoms clinically suggestive of acidic gastroesophageal reflux, who fail to respond during high dose therapeutic trial of Proton Pump Inhibitor (PPI)
2. Patients with symptoms clinically suggestive of acidic gastroesophageal reflux without esophagitis or with unsatisfactory response to a high dose of PPI in whom anti-reflux surgery is contemplated and post surgery to evaluate the effectiveness of anti-reflux surgery.
3. Patients with persistent acidic gastroesophageal reflux symptoms despite anti-reflux surgery.
As mentioned previously, pH means Potential of Hydrogen ions (H+), more H+ ions more acidic is the substance. A drop in pH 4 or below (pH<4) is indicative of severe acid reflux(Pathological Reflux).24-hour pH monitoring detects the acid reflux in the lower esophagus and is proved to be the Gold Standard test. Before laparoscopic fundoplication in suspected GERD, 24 hour -pH monitoring provides precise data on acid reflux events. It helps in selecting suitable candidates for surgery, especially classic acid reflux (pH<4). However, it may miss non-acidic reflux events and weakly acidic reflux, potentially excluding some patients who could benefit from laparoscopic fundoplication. Following fundoplication surgery ,24- hour pH monitoring is the main diagnostic test assessing the surgical outcome. It quantifies acid exposure (pH<4) indicating the success of acid suppression. However, it may not capture non -acidic or weak acidic reflux potentially leading to overestimating the procedure’s efficacy in controlling al reflux events. IMPEDANCE(MII-pH) monitoring is also very effective pH monitoring device which can detect acidic non -acidic also weakly acidic reflux events for 48 hours but it is invasive procedure like typical 24- hour pH monitoring system not comfortable for patients having nasogastric canula for 48 hours.
WIRELESS pH monitoring device (BRAVO) can detect acidic reflux for 96 hours but, it is limited in its ability to detect non-acidic reflux. It may not be the best choice for preoperative patient assessment as it could miss relevant reflux events, potentially leading to surgery being overlooked for some patients. Wireless pH device is not as effective to extract accurate data of acid reflux as 24 pH monitoring or MII-pH device pre or post-operatively after laparoscopic fundoplication. It may not be as comprehensive as accurate as other two systems in evaluating the full spectrum of reflux types after fundoplication. Wireless device is also very expensive device very few hospitals have Wireless pH monitoring system. Traditionally the typical 24-hour pH monitoring is a valuable tool postoperatively following anti-reflux surgery for assessing acid reflux control, cost effective as well but, it may miss non-acidic or weakly acidic reflux whereas MII-pH monitoring can detect acidic and non-acidic reflux. The choice of monitoring method should align with the specific needs of patient and goals of the assessment.
According to reviewed literatures the clinical implications of 24 -hour pH monitoring is enormous, providing valuable insights into the realm of patient’s management and optimum care. The clinical implication includes efficacy of laparoscopic anti-reflux surgery. The 24-hour pH monitoring helps to assess the effectiveness of the laparoscopic fundoplication procedure in controlling acid reflux. A successful surgery should demonstrate a reduction in Acid Exposure Time (AET) in the lower esophagus, indicating that procedure is working to prevent reflux. Anti -reflux surgery has better outcomes than PPI medication. There is a marked improvement of symptoms after surgery in GERD patients due to drastic reduction or complete abolition of acid reflux as measured by 24-hour pH monitoring which often correlates with symptomatic improvement, patient experience, relief of heartburn, regurgitation and other GERD symptoms. The long- term outcome following laparoscopic anti reflux can be assessed by 24- hour pH monitoring over the time, can determine the durability of the procedure’s effects. It can provide insights into long term benefits of laparoscopic fundoplication. According to numerous literatures searched most of surgeons agree laparoscopic Nissen fundoplication provides long lasting benefits for GERD patients in relation to symptom control abolishing acid reflux.
24 -hour pH monitoring results can be used to identify suitable candidates for laparoscopic fundoplication surgery. Patient with significant acid reflux (pH<4) documented through pH monitoring are more likely to benefit from the surgical anti reflux procedure.
A comparative analysis of reviewed literatures regarding 24-hour pH monitoring, the results of pre and postoperative laparoscopic fundoplication to ascertain the successful outcome of surgery, evaluation of any complications or adverse effects of the surgical procedures, also assessing the impact of the chosen type of laparoscopic fundoplication e.g. Nissen (360-degree wrap), Toupet (270-degree wrap) or Partial fundoplication. The majority surgeons concluded there is marked reduction of acid reflux and an improvement in pH level, positive impact on quality of life and other parameters after fundoplication surgery for GERD, indicating the laparoscopic fundoplication is successful in managing the reflux condition in GERD patients.
If postoperatively 24- hour pH monitoring reveals persistent acid reflux (pH<4), may prompt adjustments in patient’s management who suffer from GERD. This could involve medication changes or may need revisional anti reflux surgery which can cause high morbidity and high mortality also technically challenging (Shukla et al 2022). 24- hour pH monitoring can reveal complications such as gas bloating or swallowing difficulty that may result from laparoscopic fundoplication surgery. Early detection allows more timely intervention. In one study the clinician concluded that Ambulatory 24 -hour pH monitoring has proved to be the most sensitive and specific diagnostic investigation. It measures increased esophageal exposure to gastric acidic juice by detecting concentration of Hydrogen ions (pH<4) in lower part of esophagus. The exposure is measured in components e.g. frequency of reflux, duration of reflux episodes and accumulated Acid Exposure Time (AET). It correlates with degree of esophageal mucosal damage demonstrated by histology. The comparative score is the most reliable measurement of acid suppression (PPI) or anti reflux surgery.
Most of the studies searched demonstrated convincingly the laparoscopic Nissen fundoplication (360-degree wrap) has the most effective acid reflux control and has better outcome regarding symptom relief in comparison to Toupet (270-degree wrap) or Partial fundoplication as measured by pre and post 24-hour pH monitoring. Post- operative outcome with Laparoscopic Nissen fundoplication and Toupet fundoplication for GERD with esophagitis much superior than PPI medication subjectively and objectively. The comparative rarity of clinical and endoscopic healing in patients treated conservatively indicates the chronic nature of reflux esophagitis. 10 year follow up after laparoscopic fundoplication outcome was exceedingly better than medical therapy i.e. PPI, H2 antagonists. GERD symptoms were eliminated with anti-reflux surgery also no need for medical treatment (Dallemagne 2006). In another study patients with GERD were followed up for 6 years after Laparoscopic Nissen fundoplication and Toupet fundoplication, the result showed after one year of Laparoscopic Toupet fundoplication, more likely return of heartburn than Laparoscopic Nissen fundoplication.
In comparison with laparoscopic Toupet (270-degree wrap) and partial fundoplication the outcome of laparoscopic Nissen fundoplication was much superior. The relief of heartburn and regurgitation with Nissen fundoplication was 80-90% at 10 years follow up, while Toupet and partial fundoplication postoperatively displayed increased number of recurrence reflux episode as directed by 24-hour pH monitoring when compared with laparoscopic Nissen fundoplication (360-degree wrap). Though postoperatively outcome for acid reflux (pH<4) after Nissen fundoplication or Toupet fundoplication in GERD patients much better than laparoscopic Partial fundoplication but, regarding dysmotility outcome there is marked improvement with laparoscopic partial fundoplication than Nissen or Toupet procedure. It has been proved laparoscopic anti-reflux surgery achieves better outcome in Laryngopharyngeal Reflux due to GERD than PPI medication.
Patients with abnormal impedance and increased acid exposure (pH<4) in GERD had significantly better symptom resolution, less dysphagia and less frequent PPI use after ante-reflux surgery compared to patients of GERD with normal pH. In patients having difficulty in swallowing in GERD patients, Partial fundoplication or Toupet procedures are better choice, but they are not so effective to control acid reflux as laparoscopic Nissen fundoplication. Majority of experienced laparoscopic surgeons believe laparoscopic Nissen fundoplication is the Gold Standard for GERD. Laparoscopic Nissen fundoplication is associated with more comprehensive symptom relief especially for severe Gastroesophageal Reflux Disease (GERD) patients. Toupet or partial fundoplication are preferred when to preserve some physiological function of gastroesophageal junction is a priority.
Esophageal pH monitoring is vital tool to assess the effectiveness of fundoplication procedures. It allows the objective measurement of acid exposure (pH<4) in lower esophagus. 24-hour pH monitoring device can be used to evaluate the impact of different types of fundoplication procedures on pH level, helping to ascertain which procedure is the most effective in controlling acid reflux. pH monitoring is a type of sensor which can measure pH level in lower esophagus continuously for 24 hours, for extended period Impedance MII-pH monitor for 48 hours or Wireless pH monitoring device for 96 hours are preferred.
24-hour pH monitoring along with symptom evaluation of GERD, plays a vital role in guiding clinicians and surgeons the treatment decisions and assessing post -operative outcome. The consistencies and variations in pH monitoring results before and after laparoscopic fundoplication can provide important insights into the effectiveness of anti-reflux surgery. According to reviewed literatures there is consistent theme that most cases of GERD patients there is high acid exposure (pH<4) into lower esophagus.
The key objective of laparoscopic fundoplication surgery is to prevent acid exposure (pH<4) Into the lower esophagus by reinforcing the Lower Esophageal Sphincter (LES). It has been proved beyond doubt by expert in laparoscopic fundoplication surgeons that there definite, substantial decrease in frequency and duration of acid exposure episodes (pH<4) after reflux surgery, indicating the procedure is effectively preventing acid from stomach flowing into lower esophagus by augmenting Lower Esophageal Sphincter (LES). According to literature published the majority of surgeons believe the laparoscopic Nissen fundoplication achieves more profound reduction of acid (pH<4) reflux compared to Toupet or partial fundoplication Seeras( 2022), Mario Murano(2019), Farrel (2000) ,Booth (2006),Grande (1994), Campos (1919).They followed up patients after surgery for long time ,the duration ranging from 5 to 25 years and number of patients followed up ranging from 30 to 1000. There is variation in reduction of acid reflux in three commonly performed laparoscopic anti-reflux surgery e.g. Nissen, Toupet, Partial fundoplication.
It has been observed patients having GERD symptoms with normal pH monitoring result before surgery have significantly worse subjective outcomes after laparoscopic Nissen fundoplication compared with an abnormal pH test preoperatively. It is recommended to minimize poor symptomatic outcome after anti-reflux surgery to perform routine preoperative 24-hour pH testing.
Patients who have atypical symptom in suspected GERD,24-hour pH monitoring may still obtain good result after laparoscopic fundoplication. These patients with atypical symptom outcome after surgery is not as good as patients who experience typical GERD symptoms e.g. heartburn regurgitation during pH study after surgery (Chin et al 2008). Patients with typical symptoms of GERD with endoscopic positive result of esophagitis may not need 24-hour pH monitoring except for accurate diagnosis. These patients had long term follow up after surgery for 8 years. One study demonstrated Wireless pH monitoring device can detect more than 22 % acid reflux (pH<4) before surgery than typical 24-hour pH monitoring system (Tseng 2005).
24-hour pH monitoring can detect mucosal damage histologically also endoscopic severity of reflux esophagitis. Acid reflux can impair the motility of the esophagus due to prolonged acid exposure as detected by 24- hour pH monitoring. Variations in postoperative symptoms can happen while 24-hour pH monitoring may show residual acid exposure. This variation can exist in the level of symptom relief. Some patients may experience complete symptom free, while others may still have mild symptoms depending on the severity of their condition and type of fundoplication surgery performed.
According to reviewed literatures, those patients who have minimum symptoms or atypical symptoms of GERD, weak acid reflux before surgery, female gender, obese patients BMI more than 35, their outcome after surgery in relation to symptom relief, pH level is not good as patient who had typical GERD symptoms and abnormal acid reflux (pH<4), DMS more than 14.7. Gas related symptoms can vary postoperatively among different types of fundoplication surgery. The laparoscopic Nissen fundoplication can lead to more gas related side effects due to complete 360 degree wrap than Partial fundoplication which may result in fewer gas related symptoms. Most of the studies claim gas related symptoms after laparoscopic Nissen fundoplication is transient lasts 4 to 6 weeks, despite this problem it has been proved beyond doubt the laparoscopic Nissen fundoplication is the most effective in preventing acid reflux than other anti -reflux surgical procedures. pH monitoring reading can vary on types of pH monitoring devices used .24 - hour pH monitoring may not detect acid reflux within 24 hours in some cases as MII- pH and Wireless pH monitoring device. but typical 24 -hour pH monitoring is still the most effective tool to diagnose acid reflux also cost effective.
The wireless pH monitor is non -invasive device can detect acid reflux for up to 96 hours but it is very expensive. The main benefit of Wireless pH monitoring apart from non -invasive can overcome the limitations of De Meester score (DMS). Occasionally pH monitoring on suspected GERD patients can show false positive if they are on PPI or bile reflux, swallowing disorder esophageal achalasia or gastric emptying issues. pH monitoring could be false negative in case of intermittent reflux or weak acidic reflux, stress induced reflux, incomplete testing (short monitoring time) or patient taking PPI during pH monitoring. Positional if patient on upright position while pH monitoring conducted, improper electrode placement. It is important for healthcare provider to be aware of these factors and take them into consideration when interpreting pH monitoring results. Additionally, combining pH monitoring with Impedance device (MII-pH) can help to improve accuracy by detecting non -acidic reflux events and differentiating between liquid and gas reflux. It is of paramount important to interpret pH monitoring results in the context of specific laparoscopic fundoplication surgery. Patient’s pre- operative condition and their individual response to surgery should be considered. Variations can occur due to these factors highlighting the importance of individualized patient’s care and follow up assessment. In one study the multivariate analysis the factors predicting outcomes after laparoscopic Nissen fundoplication surgery were performed.
Data from 199 consecutive patients undergoing laparoscopic Nissen fundoplication. Variables include age, gender, BMI, primary symptoms, clinical response to acid suppression therapy, erosive esophagitis,24-hour esophageal pH score and the percentage of time acidic pH was less than 4(pH<4) on 24-hour pH monitoring, lower esophageal sphincter competence, status of esophageal body motility, hiatal hernia, gastric carditis, intestinal metaplasia of cardiac epithelium limited to gastroesophageal junction and Barrett’s esophagus of any length. Patients were followed up to 15 months post operatively. It was concluded that 24-hour pH monitoring provides the strongest outcome predictor of laparoscopic Nissen fundoplication and the outcome is based more on the correct identification of the disease than its severity. Though endoscopy (OGD)is an essential investigation in GERD but, in many cases, endoscopy may be negative but pathological acid reflux(pH<4) may be detected in lower esophagus.
Following 24-hour pH monitoring before and after laparoscopic fundoplication it is recommended that interpretation should be done by specialist either surgeon with expertise in gastroesophageal reflux disease or experienced gastroenterologist regarding result of 24 pH monitoring test. They can provide a detailed analysis and recommendation based on these findings.
Treatment decisions should be individualized based on the patient’s specific condition, symptoms and 24-hour pH monitoring results, the type of laparoscopic fundoplication i.e., Nissen, Toupet or Partial fundoplication. Clinicians should provide patients with clear explanation of 24-hour pH monitoring results including the improvements gained after surgery and variations also discuss realistic expectations for symptom relief. Depending on the postoperative 24-hour pH monitoring result, medication management may be modified, some patients may need ongoing acid suppressive medication e.g. PPI or H2antagonist even after surgery for GERD.
Symptom relief can be correlated with pH monitoring results, higher the pH level (pH>4) better the symptom relief. If there is disassociation between pH outcome and symptom then further evaluation is necessary. Clinicians should engage in shared decision making with patients regarding their ongoing care, to ensure they are actively involved in treatment choices and fully understand the implications of pH monitoring.
Ultimately 24hour pH monitoring is available diagnostic tool for evaluating the success of laparoscopic fundoplication. Future research in the areas of 24-hour pH monitoring and laparoscopic fundoplication can contribute to enhance the diagnosis and treatment of Gastroesophageal Reflux Disease (GERD) and related conditions. Hopefully potential research in future may comprise of, enhancing surgical techniques, individualized treatment options e.g. research on anatomical variation or genetic predispositions may influence the choice of laparoscopic fundoplication and predictive outcome, long-term results to assess the durability of laparoscopic fundoplication, long-lasting symptom relief and acid control. To develop patient selection criteria for laparoscopic fundoplication considering factors such as pH monitoring results, symptom severity and response to medication.
Future research should include the role of ancillary testing to explore the value of combining pH monitoring with other diagnostic test such as high-resolution manometry, Impedance pH testing or novel biomarkers to augment GERD diagnosis and treatment planning.
For children with GERD, use of pH monitoring and laparoscopic fundoplication newer approach should be considered. Scientists should explore potential new technologies for example Wireless pH testing device or smart implants to enhance the accuracy and patient’s experience of pH monitoring. Research should also include the role of monitoring in early detection and prevention of complications associated with long term acid exposure (pH<4) such as Barrett’s esophagus or esophageal adenocarcinoma. Future research will lead to advancement of diagnosis, treatment and management of GERD and related conditions ensuring that patients receive the most appropriate treatment with minimal risk.
New alternative techniques such as Incisionless Transoral Endoscopic Fundoplication have been tried but long-term outcome is not validated. The main advantage of this procedure is no external incision, shorter recovery time, reduced risk of complications e.g., infection and incision related issues also less impact on swallowing function. This technique is contraindicated in Barrett’s esophagus, Scleroderma or extraesophageal or atypical symptoms of GERD. It is not suitable for all patients, may not be as effective for severe GERD cases.
In few centers Magnetic Sphincter Augmentation (LINX) device have been tried. This device enhances the pressure of lower esophageal sphincter (LES) with made of chain of earth magnets. This device exerts ample pressure on lower esophageal sphincter (LES) but, does not obstruct passage of food with swallowing. It does not alter anatomy of the stomach. This procedure is useful for some patients with mild to moderate GERD. There is limited data on long term efficacy. It is not suitable for severe cases of GERD. It may cause dysphagia and gas bloating in some cases.
Robotic assisted fundoplication has been performed in some centers. It is precise and dexterous, good for complex cases especially complicated anatomy or severe GERD, but it is expensive, longer operative time not available in all hospitals. This technique is still in early phase, hence long-term efficacy is not substantiated.
Personalized care for GERD patient involving 24-hour pH monitoring and laparoscopic fundoplication is of paramount importance to optimize treatment outcomes i.e. preoperative evaluation of pH monitoring, symptom assessment, medical history, choosing the right anti-reflux surgical procedures e.g. Laparoscopic Nissen fundoplication, Toupet or Partial fundoplication.
The most important step is shared decision making with patients of GERD.
In summary, the findings from this review underscores the vital role of 24-hour pH monitoring in pre and post laparoscopic fundoplication for GERD. These findings not only reaffirm its significance in clinical practice but also the highlights the evolving field of pH monitoring technique. The findings from reviewed literatures will undoubtedly contribute to informed decision making and improved patient’s care in the realm of laparoscopic fundoplication of Gastroesophageal Reflux Disease (GERD).
CONCLUSION:
The Gastroesophageal Reflux Disease (GERD) affecting people worldwide can cause considerable morbidity and mortality due to acid reflux (pH<4) into the esophagus from stomach (Montreal Consensus 2006). This comprehensive review of 24
