ASSESSMENT OF KNOWLEDGE AND ATTITUDE OF LAPAROSCOPIC SURGEON TOWARD ENTRY TECHNIQUE AND ITS COMPLICATION IN NIGERIA
“ASSESSMENT OF KNOWLEDGE AND ATTITUDE OF LAPAROSCOPIC SURGEON TOWARD ENTRY TECHNIQUE AND ITS COMPLICATION IN NIGERIA"
A
DISSERTATION SUBMITTED
TO
SINGHANIA UNIVERSITY
FOR THE DEGREE OF MASTER IN MINIMAL ACCESS SURGERY
UNDER THE GUIDANCE OF
PROF. (DR).R. K. MISHRA
SUBMITTED BY:
DR.ADAMU AJI AMSHI
JUNE 2022

World Laparoscopy Hospital
CERTIFICATE
This is cerise to certify the study titled
"ASSESSMENT OF KNOWLEDGE AND ATTITUDE OF LAPAROSCOPIC SURGEON TOWARD ENTRY TECHNIQUE AND ITS COMPLICATION IN NIGERIA"
Has been carried out by
DR. ADAMU AJI AMSHI, under my supervision and to my satisfaction.

DR. R. K. MISHRA ( MBBS, MS, M MAS, MRCS, DMAS, PH.D.)
ACKNOWLEDGMENT
ACKNOWLEDGEMENT Feeling grateful is the most beautiful thing for everyone in the world in laparoscopy hospital, Thanks and gratitude to my honorable teacher PROF. DR. R. K. Mishra
I am also thankful to DR. USMAN MUHD BELLO OF AKTH for his support in this study. Grateful thanks to my colleagues in Yobe State Specialist Hospital and Ayaji Medical And Diagnostic Centre Gashua for their support and help for complete this study.
I am also thankful to my parents, my wives and my children, and my entire family.
Lastly I am thankful to all paramedical staff and technicians for their help in various ways for this study.
ASSESSMENT OF KNOWLEDGE AND ATTITUDE OF LAPAROSCOPIC SURGEON TOWARD ENTRY TECHNIQUE AND ITS COMPLICATION IN NIGERIA

DR. ADAMU AJI AMSHI
BSC, MBBS,FMAS,DMAS,FICRS.
TABLE OF CONTENT
ABSTRACT
Assessment of knowledge or attitude toward laparoscopic surgery formed entry techniques and its complication was conducted using 21 participants survey research design was used for the study. The aim was to determine the benefits and risks of different laparoscopic entry techniques in gynecological and non-gynecological surgery. A questionnaire of 21 items was used for data collection. The data collected was analyzed using descriptive statistics and was presented using pie charts. The result revealed that most of the surgeons are practicing chrome tubular dye and adhesiolysis surgery with different access techniques none of the surgeons encountered death due to complications, however, most of them encountered. Some complications and managed laparoscopically and continue with the procedure.
CHAPTER ONE
INTRODUCTION
1.1BACKGROUND TO THE STUDY
Laparoscopy is a common procedure in many surgical specialties. Complications arising from laparoscopy are often related to initial entry into the abdomen. The technique of first entry inside the human body with a telescope as an instrument, Technique of access in different for different minimal access surgical procedures, it is important to know that approximately 20% of laparoscopic complications are caused at the time of initial access. Developing access skills is one of the important achievements for the surgeon practicing minimal access surgery
This procedure uses a laparoscope ‐ a thin tube with a light and a camera on the end, similar to a telescope that is inserted under general anesthesia through a small cut or incision (0.5 cm to 1 cm) into, or near, the navel. The camera can project images onto external screens, which allow surgeons to directly visualize the pelvic and abdominal organs. This permits the performance of keyhole surgery, which uses much smaller surgical tools without the need for large incisions. When laparoscopy is performed, gas is gently pumped into the abdomen to increase the workspace for the camera and tools. The method by which incisions are made to introduce the laparoscope may influence the likelihood of complications. Although laparoscopy is usually safe, a small minority of patients experience life‐threatening complications, including injury to surrounding blood vessels or the bowel. These complications often occur at the first step of the procedure, when the abdominal wall is pierced with specialized instruments to insert the gas, or during the primary insertion of the trocar. Different doctors use different specialized instruments and techniques.
1.2 STATEMENT OF THE PROBLEM
The most common problem in minimal access surgery is entry techniques which lead to life-threatening complications and lack of advanced instruments is also a contributory factor.
1.3 OBJECTIVES OF THE STUDY
To evaluate the benefits and risks of different laparoscopic entry techniques in gynecological and non-gynecological surgery.
To provide clinical direction, based on the best evidence available, on laparoscopic entry techniques and technologies and their associated complications.
1.4 RESEARCH QUESTIONS
What is the common laparoscopic surgery you perform and what types of entry techniques do you prefer?
How many occasions have you converted to open surgery, due to entry complications?
How do you manage bowel perforation occurring during entry?
If you accidentally injure Inferior Epigastric vessels, what will you do?
1.5 SCOPE AND LIMITATION OF THE STUDY
It requires insertion of a cannula through the abdominal wall, distention of the abdominal cavity with gas or air (pneumoperitoneum), and visualization and examination of the abdomen’s contents with an illuminated telescope. With the advent of video cameras and other ancillary instruments, laparoscopy rapidly advanced from being a diagnostic procedure to one used in fallopian tubal occlusion for sterilization and eventually in the performance of numerous surgical procedures in all surgical disciplines for a variety of indications.
It cannot be used in all cases and even in the most expert hands there is a percentage of cases that will be converted to open surgery. The operation time in the majority of cases is more compared to open surgery. The complication rate is also higher.
1.6 SIGNIFICANCE OF THE STUDY
This study is to assess the knowledge and attitude of the laparoscopic surgeon toward entry techniques and its complication in Nigeria from 6 geopolitical zones. To encourage the use of adverse technology.
CHAPTER TWO
Literature Review
2.0 INTRODUCTION
The introduction of the first trocar, often following the creation of the pneumoperitoneum is considered a crucial, and the most dangerous step of a laparoscopic procedure. Throughout the year individual methods of laparoscopic entry were described. The first person to create the pneumoperitoneum was German surgeon Georg Kelling (1866-1945). He performed this procedure on dogs. Among the methods actually used, arguably the most popular method of the closed laparoscopic entry probably was introduced in 1947 by Raol Palmer (1904-1945) French gynecologist, who was also the inventor of an insufflator, which was adapted from a colposcopy pressure measuring device. He was followed by Kurt Semm (1927-2003) German gynecologist, who invented also an automated electronic insufflation device. They both used in this technique the needle formerly developed in 1938 by a Hungarian, Janos Veres.
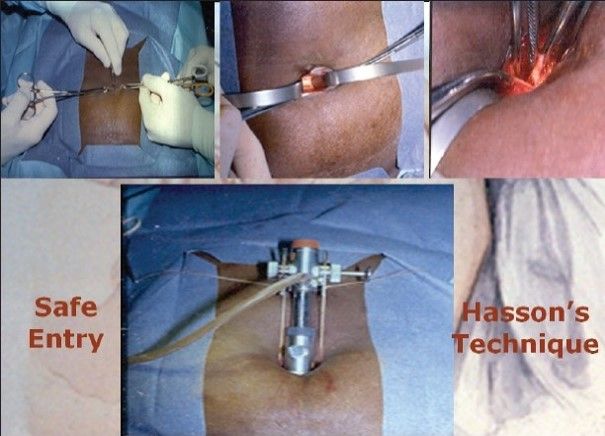
(1903-1979) which had been primarily used for the creation of a pneumothorax. The last two, but not least to mention is Harrith M. Hasson, an American who described the open-access laparoscopy in 1970, arguably considered the safer than the classic closed (blind) method, and JR Dingfelder, who developed the direct laparoscopic trocar insertion technique in 1978.
2.1 CLOSED ACCESS
In the closed access technique, pneumoperitoneum is created by veress needle. This is a blind technique and the most commonly practiced way of access by surgeons and gynecologists worldwide. Closed technique of access merely by veress needle insertion and creation of pneumoperitoneum is an easy way of access but it is not possible in some of the minimal access surgical procedures like axilloscopy, retroperitoneoscopy, and totally extraperitoneal approach of hernia repair. In general, a closed technique by veress needle is possible only if there is a preformed cavity like the abdomen.

2.2 OPEN ACCESS
In this there is a direct entry by open technique with creating pneumoperitoneum and insufflator is connected once blunt trocar is inside the abdominal cavity under direct vision. There are various ways of open access like the Hasson technique, Scandinavia technique, and fielding technique.
Some surgeons and gynecologists practice blind trocar insertion without pneumoperitoneum. The incidence of injury due to this type of access is much higher. This type of direct trocar entry is practiced by gynecologists for sterilization. Sterilization may be performed because In multipara patients the lower abdominal wall is lax; making the fascia thinner and easy elevation by hand is possible.
Bleeding due to accidental damage to a major vessel during this initial stage is one of the dangerous complications of laparoscopic surgery.
2.3 ANATOMY OF ANTERIOR ABDOMINAL WALL
There are three large, flat muscles (External oblique, internal oblique, and transverse abdominal) and one long vertically oriented segmental muscle (rectus abdominis) on each side. Four major arteries on each side are also present which form an anastomotic arcade that supplies the abdominal wall. The superior and inferior epigastric artery and the branches provide the major blood supply to the rectus abdominis muscles and other medial structures.
Among all those arteries, the most important for a laparoscopic surgeon is the inferior epigastric artery and vein.
2.4 VERESS NEEDLE INSERTION
The standard method of insufflation of the abdominal cavity is via a veress needle inserted through a small skin incision in the infra umbilical region. The veress needle consists of a sharp needle with an internal spring-loaded trocar. The trocar is blunt-ended with the lumen and a side hole. Before using veress needle, it should be checked for its patency and spring action. the spring action of veress needle can be checked by pulling the head out. The disposable veress needle spring action can be checked by pressing the sharp end against any sterilized draping.
Insufflation via the veress needle creates a cushion of gas over the bowel for insertion of the first trocar. Insufflation then retracts the anterior abdominal wall, exposing the operative field.
2.5 PREPARATION OF PATIENT
The patient should be nil orally from the morning of surgery. In some procedures like LAVH or colorectal surgery where distended bowel may interfere, it is good to prepare the bowel prior to the night of surgery by giving some mild purgative. Bowel preparation can minimize the need for an accessory port to retract the bowel.
Before coming to the operation theater, the patient should always void urine. The full urinary bladder may gat perforation at the time of insertion of veress needle or trocar. If gynecology operative surgery or any general surgical lower abdominal procedure has to be performed (like hernia or adhesiolysis) it is wise to insert a Foley catheter.
A distended stomach will not allow proper visualization of the clots triangle and then the surgeon has applied more traction over the fundus or Hartman pouch and this may cause tending of CBD followed by accidental injury. In a gynecological or lower abdominal laparoscopic procedure, it is necessary to put a nasogastric tube. In minimal access surgery, shaving off skin is not a must and if necessary, it should be done on the operation table itself by the surgeon.
2.6 Patient Position
Initially, at the time of pneumoperitoneum by veress needle, the patient should be replaced supine with 10 to20 degrees head down. The benefit of this steep Trendelenburg position is that bowel will be pulled up and there will be more room in the pelvic cavity for safe entry of veress needle. It’s important to remember that patient is placed in a head-down position only if a surgeon is planning to insert a verse needle pointing toward the pelvic cavity. if the surgeon is planning to insert a verses needle perpendicular to the abdominal wall as in the case of a very obese patient or diagnostic laparoscopy in local anesthesia, they should be placed in a supine position otherwise all the bowel will come just below the umbilicus and there is increased risk of bowel injury.
In gynecological laparoscopy procedures or if laparoscopy is planned to be performed together with hysteroscopy, the patient should be positioned in a lithotomy position and one assistant should be positioned between the leg of the patient. The patient leg should be comfortable and supported by a padded obstetric leg holder or Allen stir ups which minimizes the risk of venous thrombosis. In these procedures, the surgeon needs to use a uterine manipulator for proper visualization of female reproductive organs. The assistant seating between the legs of the patient will keep on watching the hand movement of the surgeon on the monitor and he should give with the handle of the uterine monitor inappropriate. If thoracoscopy or retroperitoneoscopy is planned then the patient is placed in a lateral position.
2.7 PREPARATION FOR ACCESS
Before starting access, the abdomen should be examined for any palpable lump. It is wise to tell the patient to avoid urine before coming to the operating room but if the bladder is found full at the time of palpation. Foleys should be applied. Remember that the full bladder may be injured very easily by veress needle or trocar Once the patient is cleaned painted and draped, all the connections should be attached, Followed by focusing and white balancing of the camera. At the time of focusing, the distance between the gauge piece and the tip of the telescope should be 6 to 8 cm.
2.8 CHOICE OF GAS FOR PNEUMOPERITONEUM
Carbon dioxide and nitrous oxide are now preferred gas because of the increased risk of air embolism with room air. carbon dioxide is used for insufflation as it is 200 hundred times more diffusible than oxygen, it is rapidly cleared from the body by the lungs and will not support combustion. N2O is only 68 percent as rapidly absorbed in blood as CO2.N2O has one advantage over co2 that it has a mild analgesic effect, and hence no pain if diagnostic laparoscopy is performed under local anesthesia. Co2 has the advantage of being non-combustible and allows concomitant use of electrocoagulation laser irradiation.
2.9 SITE OF VERESS NEEDLE ENTRY
There are many sites of veress needle entry tried for veress needle insertion but the central location of the umbilicus and ability of the umbilicus to hide scar make it the most attractive site for the primary port. Umbilical is a good site for access because it is:
• Thinnest abdominal wall ( easy access)
• Cosmetically better
• No significant blood vessel
• Ergonomically better (the center point of the abdomen).
Initially, there was controversy regarding the use of umbilicus for first port access. The first concern was regarding infection. The umbilicus is a natural dirty area and many surgeons were having this impression.
The second fear of using the umbilicus was a ventral hernia.
• Umbilicus should be cleaned meticulously before incision.
• Rectus sheath of the 10mm port should be repaired.
If an umbilical route is used for tissue retrieval, infected tissue should be removed after putting in an endo bag; it should not contaminate the port wound.
2.10 INTRODUCTION OF VERESS NEEDLE
Veress needle should help like a dart. At the time of insertion, there should be 45 degrees of elevation angle. The elevation angle is the angle between the instrument and the body of the patient. To get an elevation of 45 degrees the distal end of the veress needle should be pointed toward the anus.
To prevent the creation of a preperitoneal slip of the tip of veress needle, it is necessary that veress needle should be perpendicular to the abdominal wall. However, there is a fear of injury to great vessels or bowel if veress needle is inserted perpendicular to the abdominal wall. To avoid both the difficulty (creation of preperitoneal space and injury to a bowel to great vessels), the lower abdominal wall should be lifted in such a way that it should lie 90-degree angle in relation to the veress needle will be at an angle of 45 degrees Pointed towards the anus. Lifting of the abdominal wall should be adequate so that the distance of the abdominal wall from the viscera should increase if less than the required dose of muscle relaxant is given in a muscular patient, lifting of the abdominal wall may be difficult.in multipara patients, lifting the lower abdominal wall is very easy, Increases the distance of skin from the rest of the abdominal wall more than the distance of the abdominal wall from the viscera.
2.11 INDICATORS OF SAFE VERESS NEEDLE INSERTION
Needle movement test
Once the veress needle is inside the abdominal cavity, the tip of veress needle should be free and if the surgeon will gently move the tip of the needle there should not be the feel of any resistance. It is very important to remember that veress needle should not be moved inside the abdominal cavity much, otherwise there is a risk of laceration of the bowel to be punctured.
2.12 IRRIGATION TEST
A 10ml syringe should be taken in one hand and surgeon should try to inject at least 5ml of normal saline through veress needle. if the tip of veress needle is inside the abdominal cavity there will be a free flow of saline otherwise some resistance is felt in injecting saline.
2.13 ASPIRATION TEST
After injecting saline, the surgeon should try to aspirate that saline back through veress needle. If the tip of veress needle is in the abdominal cavity, the irrigated water cannot be sucked. But if it is in pre-peritoneal space in muscle fiber or above; the rectus the injected water can be aspirated back. In an aspiration test, if more irrigated fluid is coming, then the surgeon should suspect ascites, some cysts, or perforation of the urinary bladder. If fecal matter is seen then perforation of the bowel may be the reason and if blood is coming then the vessel injury is the cause. If any fresh blood or fecal fluid is aspirated in the syringe surgeon should not remove the veress needle and urgent laparotomy is required. Leaving veress needle in position is helpful in two ways. First, it is easy to find the punctured area after laparotomy and secondly, the further bleeding will be less.
2.13 HANGING DROP TEST
A few drops of saline should be poured over the veress needle and the abdominal wall should be lifted slightly. If the tip of the veress needle is inside the abdominal cavity the hanging drop should be sucked inside because inside the abdominal, there is negative pressure. If the tip of veress needle is anywhere else the hanging drop test will be negative. 0nce it is confirmed that veress needle is inside the abdominal cavity the tubing of the insufflator is attached and flow is started. It is important to keep a nice hold on veress needle throughout while gas is flowing; otherwise, veress needle can slip out and may create a preperitoneal insufflator.
.
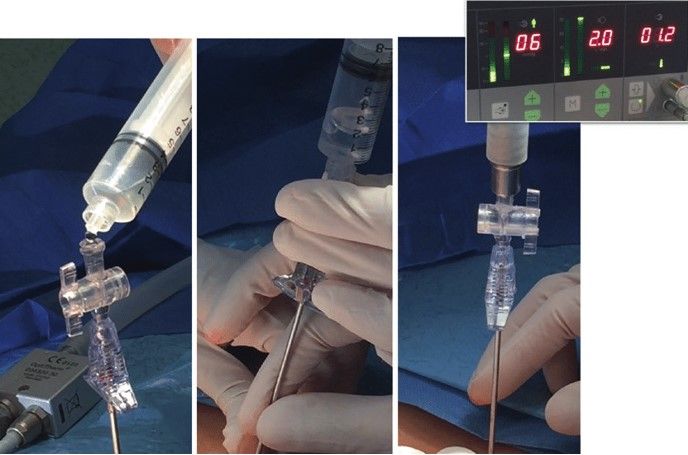
2.14 INSUFFLATOR OF GAS TEST, QUADRO-MANOMETRIC TEST
For safe access, the surgeon should always see carefully all four indicators of insufflator at the time of the creation of pneumoperitoneum. If the gas is flowing inside the abdominal cavity there should be a proportionate rise in actual pressure with the total gas used. Suppose only with the entry of 400 to 500 ml of gas, lf actual pressure is equal to preset pressure of 12 mm Hg, that means gas is not in the free abdominal cavity, it may be in pre-peritoneal space or inside omentum or maybe in the bowel. lf gas is flown more than 5 litter without any distension of abdomen that may be due to leakage or gas may be going the vessels.
2.15 QUADRO-MANOMETRIC INDICATOR OF INSUFFLATOR

Quadro-manometric indicators are the four important readings for insufflators.
The insufflator is used for monitor;
• Preset insufflation pressure.
• Actual pressure
• Gas flow rate
• Volume of gas consumed.
2.16 ACTUAL PRESSURE
This is the actual intra-abdominal pressure sense by the insufflator. When veress needle is attached, there are some errors in the actual pressure reading because of resistance of the flow of gas through the small caliber of the veress needle. Since continuous flow of insufflating gas through veress needle usually gives an extra 4 to 8 mm Hg of measured pressure by the insufflator, the true intra-abdominal pressure can actually be determined by switching the flow from the insufflator off for a moment. Many microprocessor-controlled good quality insufflators deliver a pulsatile flow of gas when the veress needle is connected, in which the low reading of actual pressure measures the true intra-abdominal pressure. If there is any major gas leak, the actual pressure will be less and the insufflator will try to maintain the pressure by ejecting gas through its full capacity.
Actual pressure of more than 20 to 25mm Hg has the following disadvantage over the hemodynamic status of the patient.
• Decrease venous return due to vena cava compression leading to;
- Increased chance of DVT (deep vein thrombosis of calf)
- Hidden cardiac ischemia can precipitate due to decreased cardiac output
• Decrease tidal volume due to diaphragmatic excursion
• Increase risk of air embolism due to venous intravasation
• Increase risk of surgical emphysema.
2.17 FLOW RATE
This reflects the rate of flow of CO2 through the tubing insufflator. When veress is attached the flow rate should be adjusted to 1 liter per minute. Studies performed on animals in which direct IV CO2 was administered and was found that the risk of air embolism is less if the rate is within 1 liter /minute. At the time of access using the veress needle technique, some time veress needle may inadvertently enter inside a vessel if the flow rate is 1 liter /minute there is less chance of serious complication when initial pneumoperitoneum is achieved and cannula. If inside the abdominal cavity, the insufflator flow rate may be set at maximum, to compensate for the loss of CO2 due to the use of a suction irrigation instrument. This should be remembered that if the insufflator is set to its maximum flow rate then also it will allow flow only if the actual pressure is less than the preset pressure otherwise it will not pump any gas.
2.18 TOTAL GAS USED
As soon as 100 or 200 ml of gas is inside the abdominal cavity, the surgeon should do percussion of the right hypochondrium and liver dullness should obliterate with tympanic sound. This is the fourth indicator of insufflator. Normal size human abdominal cavity needs 1.5 liter CO2 to achieve intra-abdominal actual pressure of 12mm Hg. In some big-size abdominal cavities and in multipara patient some time we need 3liter CO2 (rarely 5 to 6 liters ) to get desired pressure of 12mm Hg. When less or more gas is used to inflate a normal abdominal cavity, the surgeon should suspect some errors in pneumoperitoneum techniques. These errors may be leakage or maybe preperitoneal space creation or extravasation of gas.
2.19 PRIMARY TROCAR INSERTION
Technical errors in the insertion of trocars after the creation of pneumoperitoneum are the most common causes of injury, resulting from inadequate stabilization of the abdominal wall, excessive resistance to trocar insertion, and excessive, misdirected, or controlling force applied by the surgeon along the axis of the trocar.
It is important to stabilize the abdominal wall by full insufflation, and complete muscle relaxation, to increase the distance between the anterior abdominal wall and the retroperitoneal vessels, and the abdominal organs. It is important to insure that the skin incision is of sufficient length and that the reusable trocar tip is sharp so that no resistance is offered. Trocar and cannula designs correctly available have a number of basic pictures in common. They come in a variety of sides and the central trocar may have a pyramidal, conical or rounded tip. They have a valve system and a gas input with a tap.
The dispensable cannula has a flap valve care should be taken when a person instruments through the port. Some disposable cannulas have a safety system. A cylinder jumps forward after penetration of the abdominal wall and forms a shield over a sharp trocar tip. This is not foolproof due to shield lag. In the most reset disposable cannula, the trocar itself is spring-loaded. New designs of the cannula, some quite minimalist are correctly under investigation. The first trocar and cannula inserted is an 11mm disposable trocar. This will accommodate a 10 mm telescope and leave sufficient space in the cannula for rapid gas insufflation if required.

2.20 STEPS OF PRIMARY TROCAR INSERTION
Patient position
As for veress needle insertion, patient should be placed supine with 10 to 20 degrees head-down. The cephalocaudal relationship between the aortic bifurcation and the umbilicus has been studied radiologically. The umbilicus is often located directly above or cephalad to the aortic bifurcation and is constantly located cephalad to where the left common iliac vein Crosse the midline. The aortic bifurcation is located more caudal to the umbilicus in the trend-Ellenburg position than in the supine position.
2.21 SIT
The same side of veress needle entry should be used for primary trocar insertion. The inferior or superior crease of the umbilicus can be used in average-built patients and transumbilical insertion can be used in obese patients. Before introducing the trocar, the surgeon should confirm pneumoperitoneum. After distension of the abdominal cavity, the actual pressure should be equal to the preset pressure and gas flow should be stopped.
Before the introduction of the trocar, the initial 1 mm stab puncture wound of skin for veress needle should be extended to 11 mm. it should be remembered that the most common cause of forceful entry inside the abdominal cavity with primary trocar is small skin incision. To avoid inadvertent injury of the bowel due to forceful uncontrolled entry, the incision of the skin should not be less than 11 mm in size. The skin incision for trocar should be smiling in shape (u-shaped) along the crease of the umbilicus to get a better cosmetic value.
After giving an 11 mm incision with 11 number blades, the surgeon should spread fatty tissues with a Kelly clamp.
2.22 INTRODUCTION OF PRIMARY TROCAR
The surgeon should hold the trocar in a proper way. The Head of a trocar should rest on the thenar eminence, the middle finger should encircle the air inlet and the index finger should point toward the sharp end After holding the trocar properly in hand, the full thickness of abdominal wall should be lifted by the fingers thenar and hypothenar muscles. After the creation of pneumoperitoneum lifting the abdominal wall is difficult because it slips. To overcome this, it should be grasped to counter the pressure exerted by the tip of the trocar.
Angle of Insertion
Initially, the angle of insertion for the primary trocar is perpendicular to the abdominal wall both once surgeon feels a giving sensation, the trocar should be tilted to 60 to 700 angles.
2.23 CONFIRMATION FOR ENTRY OF PRIMARY TROCAR
• Audible click if dispensable trocar or safety trocar is used.
• Whooshing sound if the reusable trocar is used (gas passes from the hole at the tip of the pyramidal sharp trocar to the head of the trocar).
• Loss of resistance felt both in disposable as well as a reusable trocar.
Once the cannula is in place tubing of the insufflator is attached again and flow is restarted to refill the CO2 at a preset pressure.
The telescope is introduced slowly keeping the oblique cut edge down in case of the 30-degree telescope.
Once the telescope is inside, the elevation angle of the telescope should be 90 degrees with panoramic vision. the side just below the entry of the primary port is examined for any vessel or just below the side of entry but these few drops of blood are trickled blood through the umbilical wound. If the surgeon has any doubt about perforation of bowel or injury to the vessel, he should evaluate this area again after putting other posts.
Working Ports
To select the site for the secondary port, transillumination with an illuminated telescope tip should be done first to locate an avascular area to avoid injury to subcutaneous vessels.
2.23 SUBSEQUENT PORTS
Subsequent trocar are inserted under direct vision at locations appropriate for the procedure and to the anatomy of the individual. if the port is on the opposite side of patient, it can be introduced same way but if surgeon is not able to bend enough to opposite side, his right index finger can be placed over the head of the trocar and his left head should guard the shaft of cannula. With slow rotatory movement of right hand, first the tip of the trocar should be perpendicular to the skin but as soon as tip of trocar is seen direction of trocar should changed towards the anterior abdominal wall. Alternatively, the surgeon can go another side of the patient and he introduce the trocar in conventional
2.24 ADVANTAGE OF OPEN TECHNIQUE
• Definite, small risk of injury with blind veress needle technique irrespective of experience
• Particularly useful in previous abdominal surgery or underlying adhesions.
• The incidence in of injury to adhesions although not eliminate is significantly reduced by entry into the peritoneal cavity under direct vision.
• There is a decreased risk of injury to the retroperitoneal vessels.
• The risk of extraperitoneal insufflator is eliminate.
• Increasing number of surgeon performing laparoscopy without experience and in these group open technique may be easy.
The Hasson trocar system was initially developed for laparoscopy in patient who has had a previous laparotomy. After seeing benefit of open access technique, many surgeons started using open access technique routinely in their entire patient. An access wound was made using traditional open technique and the Hasson trocar and cannula designed to both fix the port and seal this larger wound round the port. It requires the use of sutures to prevent slippage of port. This involved making the small entry wound directly through the scar tissue of the umbilicus and then dilating this up by passage of a blunt preferable conically tipped trocar and cannula.
2.25 STEPS OF OPEN ACCESS TECHNIQUE
A transverse incision is made in the subumbilical region the upper skin flap is retracted using a small right-angled retractor. Subcutaneous tissue is dissected till the linea alba and the rectus sheath are visualized. Stay sutures are taken on either side of the midline.
The transverse incision for open access
• Stay suture is giving both the ends of transverse incision.
• Both the stays are pulled up to make s bridge like elevation of rectus
• Rectus sheath is incised in the midline along the line of linear alba pointing upward. Incision should not penetrate the peritoneum; otherwise any adhesion with the peritoneum may be punctured.
• A hemostat is stabbed into the peritoneum while holding the stay up
• The give-way of the peritoneum can be felt as peritoneum is perforate and then the hemostat is opened to widen the opening.
• Surgeon should insert his finger to feel all around inside the abdominal cavity to feel any possible adhesion.
• Small tiny adhesion felt can be broken with a gently sweeping movement of the finger. Blunt trocar-cannula should be inserted for the first port after visualizing the intraperitoneal viscera.
• Care is taken not to make a big incision; cannula dilates the smaller incision to give an airtight fit.
• If an incision is big, a purse-string suture should be applied to hold the port in the proper position.
2.26 OPEN FIELDING TECHNIQUE
This technique develop by fielding in 1992 involve a small incision over the everted umbilicus at a point where the skin and peritoneum are adjacent. The Fielding technique is useful in patients with abdominal incisions from previous surgery provide there is no midline incision, portal hypertension and recanalyzed umbilical vein, and umbilical abnormalities, such as urachal cyst, sinus, or umbilical hernia. Through skin preparation of the umbilicus is carried out and the everted umbilicus is incised from the apex in a caudal direction, two small retractors are inserted to expose the cylindrical umbilicus tube running from the undersurface of the umbilical skin down to the linea alba.
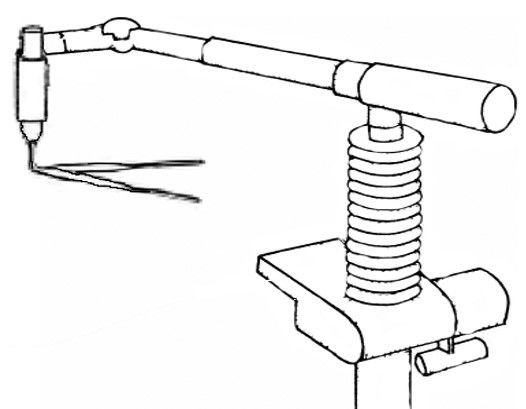
2.27 Laparolift Technique
Laparolift (Autosuture) device consists of a hydropneumatic elevator and specific interchangeable body hooks in V or C shape. It enables the achievement of laparoscopic entry completely without the creation of a pneumoperitoneum, with relatively low invasiveness (however incomparably greater than in other methods of laparoscopic entry described above).
2.28 THE SINGLE PORT LAPAROSCOPY
It appears obvious, that the future belongs to these even less invasive procedures. Both NOTES and single port laparoscopy, without exception also demand laparoscopic entry. These are mainly based on the access methods with the use of a pneumoperitoneum, like in the single port laparoscopic surgery, where the paraumbilical mini-laparotomy is performed, to insert a larger port. Also in NOTES, the need for the creation of a pneumoperitoneum is achieved through the closed entry-like access, with the use of a needle introduced to the abdominal cavity through the vaginal fornix.

2.28 COMPLICATIONS DURING ENTRY STAGE INTO THE ABDOMEN IN LAPAROSCOPIC SURGERY
To review laparoscopic access systems, insertion techniques, and the risks of complications associated with their use. Access devices usually comprised an external cannula and a removable sharp pyramidal trocar for penetration of the abdominal wall, and were nearly universally positioned following the establishment of a pneumoperitoneum. However, it is apparent that such devices and techniques contribute to patient morbidity through visceral and vascular injury, as well as incision-related complications such as dehiscence and hernia. There exist alternative approaches to positioning insufflation needles and the initial cannula, which may reduce the incidence of vascular and visceral injury, particularly in the face of previous abdominal surgery. Inserting the initial cannula after mini-laparotomy is associated with a reduced risk of vascular injury, but visceral complications still occur.
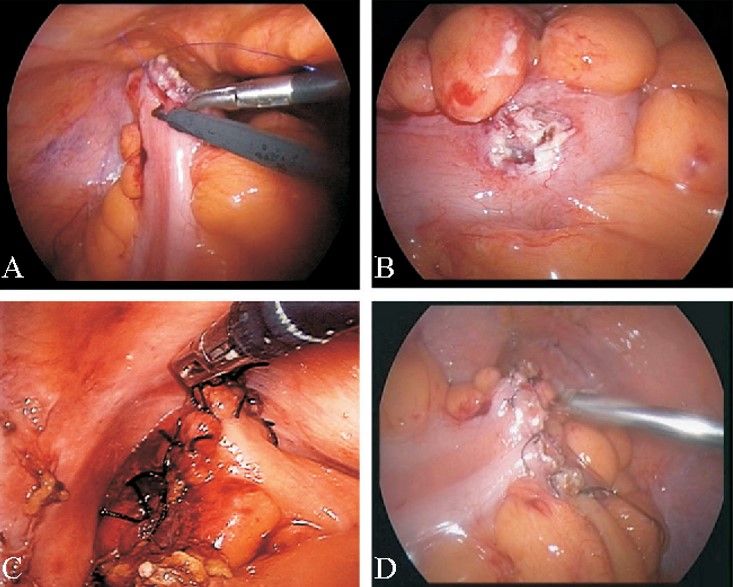
2.29 VASCULAR INJURY AND ITS MANAGEMENT
Vascular injury is a major cause of death from laparoscopy, major vascular injury can occur when the Veress needle is inserted prior to insufflation or when a trocar is inserted after insufflation. Some new access instruments may reduce the risk of some complications associated with 'blind entry', and although not all seem to be effective in this regard, a set of blunt-tipped devices now exist, which are surprisingly easy to position and may limit the risk of injury while significantly reducing the size of the myofascial defect in the abdominal wall. Port site metastasis is a relatively newly recognized complication of oncological surgery and is a concern, but further investigation is required to determine whether such metastasis is related to a change in clinical outcome. The incidence and spectrum of access-related complications is greater than previously perceived.
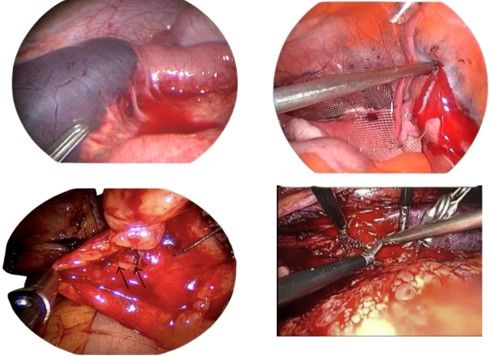
2.30 BOWEL INJURY AND ITS MANAGEMENT
CHAPTER THREE
MATERIALS AND METHODS
3.1 STUDY DESIGN
Survey research design is defined as “the collection of information from a sample of individuals through their responses to questions (Check & Schutt,2012, P. 160). This type of research allows for a variety of methods to recruit participants, collect data and use various methods of instrumentation.
3.2 STUDY AREA
The study area is Nigeria with 36 state and federal capital Abuja were some tertiary hospital are selected from 6 geopolitical zones. Aminu Kano Teaching Hospital, National Hospital Abuja, Yobe State Teaching Hospital Damaturu, Lagos University Teaching Hospital and University of Maiduguri Teaching Hospital.
3.3 STUDY SAMPLE
Twenty-one (21) respondents were used as the sample. A simple random sampling technique was used to select the sample, For the use of this research work.
3.4 METHOD OF DATA COLLECTION
A questionnaire containing 23 items was used for data collection. They were requested not to write their names on the questionnaire.
3.5 METHOD OF DESCRIPTIVE STATISTICAL ANALYSIS
The method was performed for the responses using percentages, Bar charts, and Pie charts.
CHAPTER FOUR
DATA PRESENTATION, ANALYSIS, AND DISCUSSION
4.1 INTRODUCTION
This chapter presents an analysis and discussion of the study findings. The results are presented in a bar chart, pie chart, and content delivery to highlight the major findings. The results have also been presented sequentially according to the research questions of the study. Simple descriptive statistics such as simple frequency percentages were used to analyze the data collected. The findings were discussed and interpreted in relation to the objectives of the study.
TABLE 4
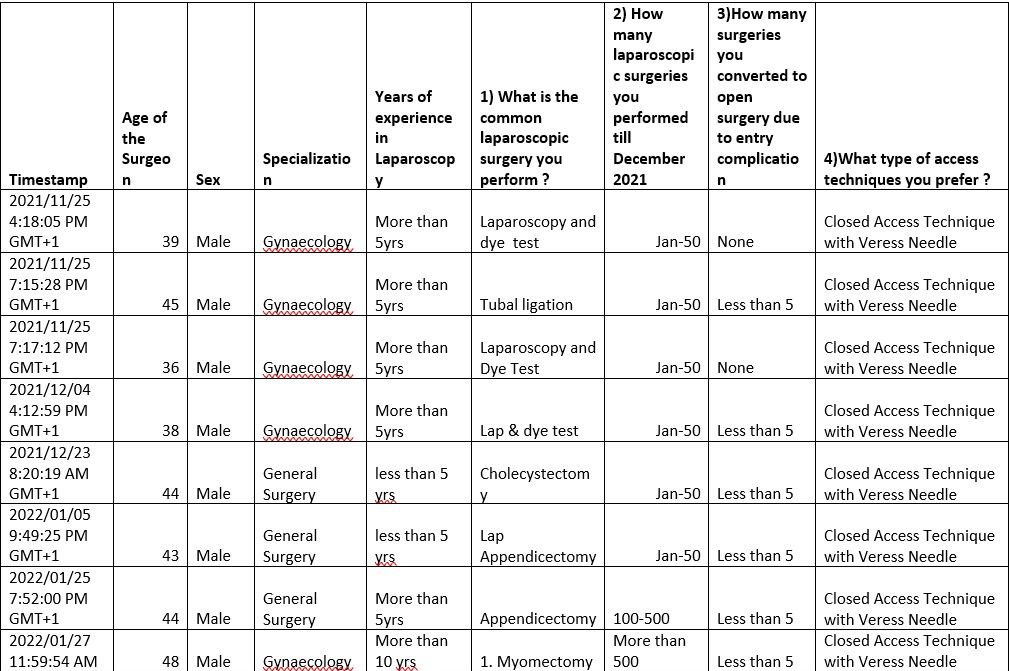
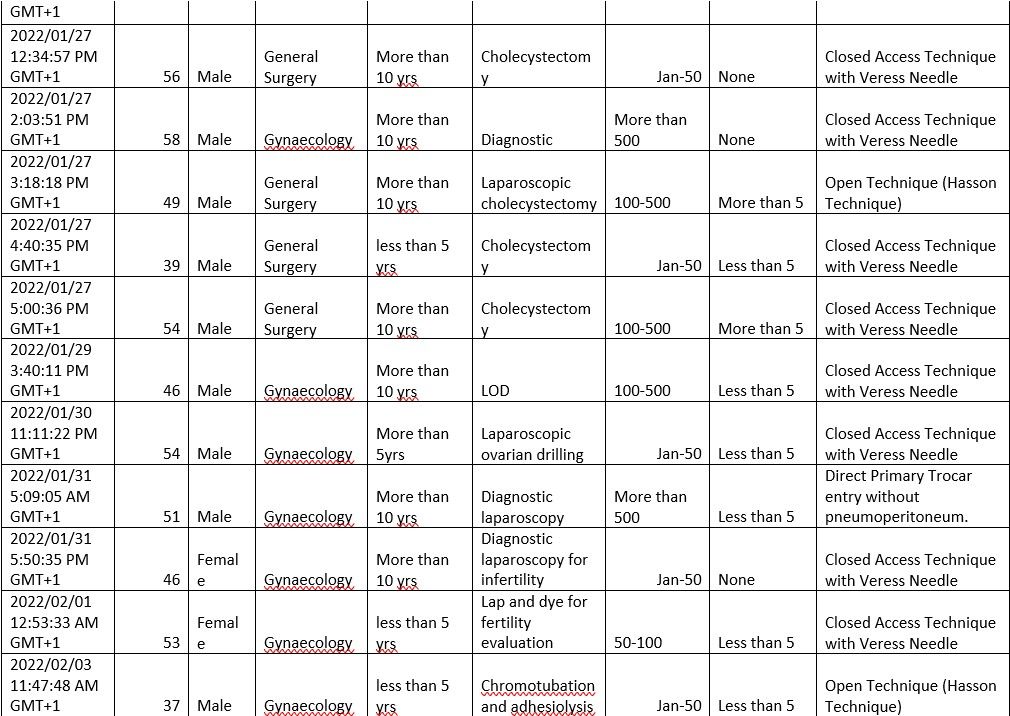
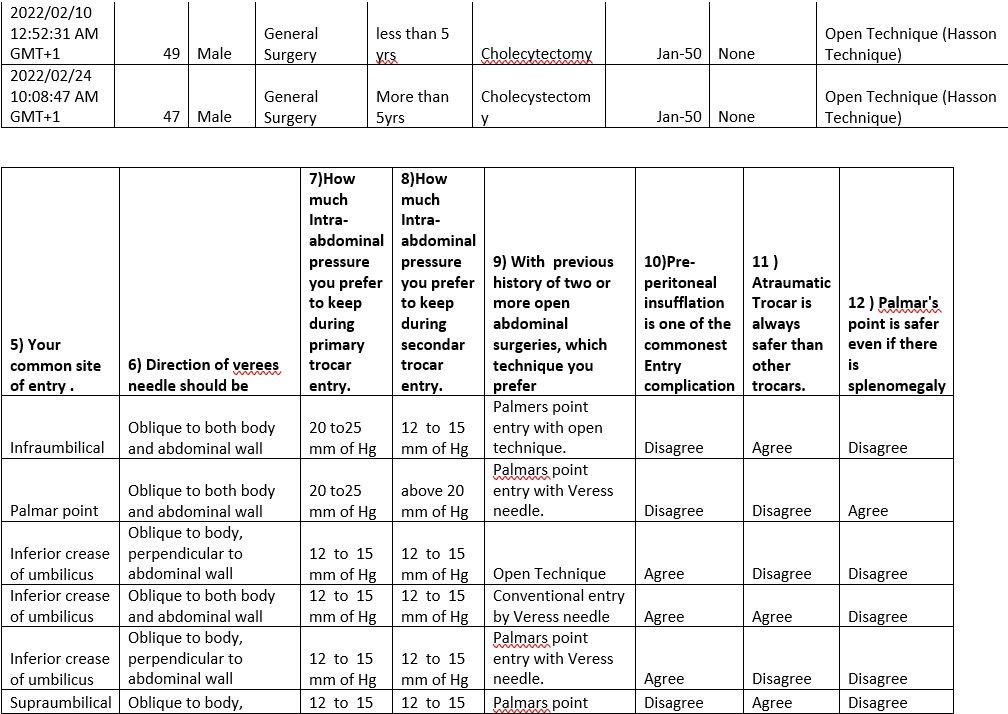
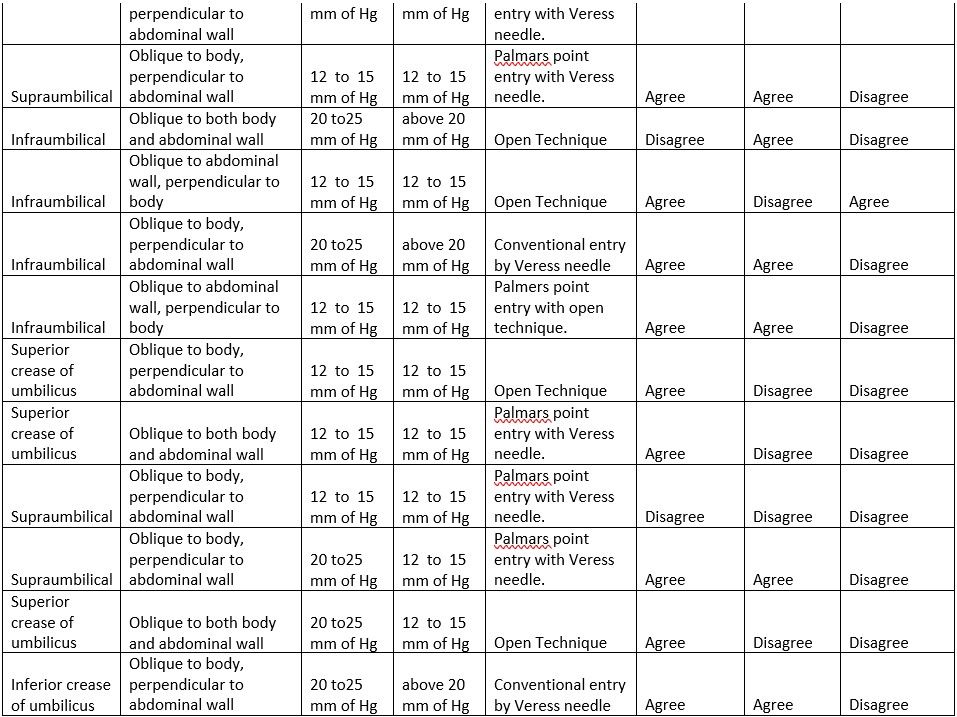
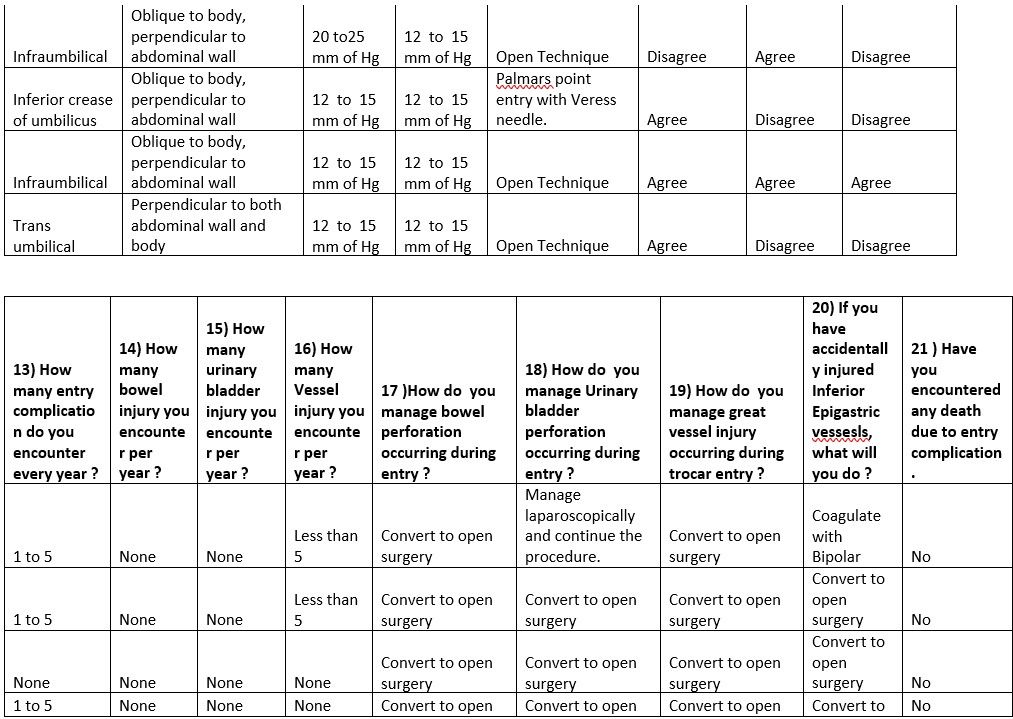
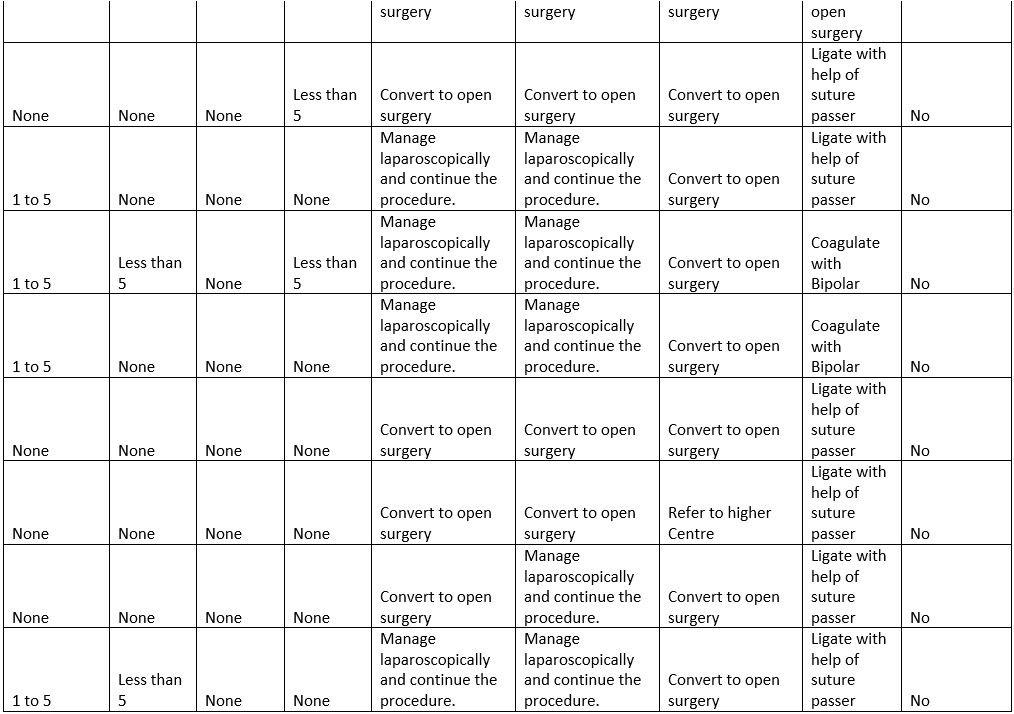
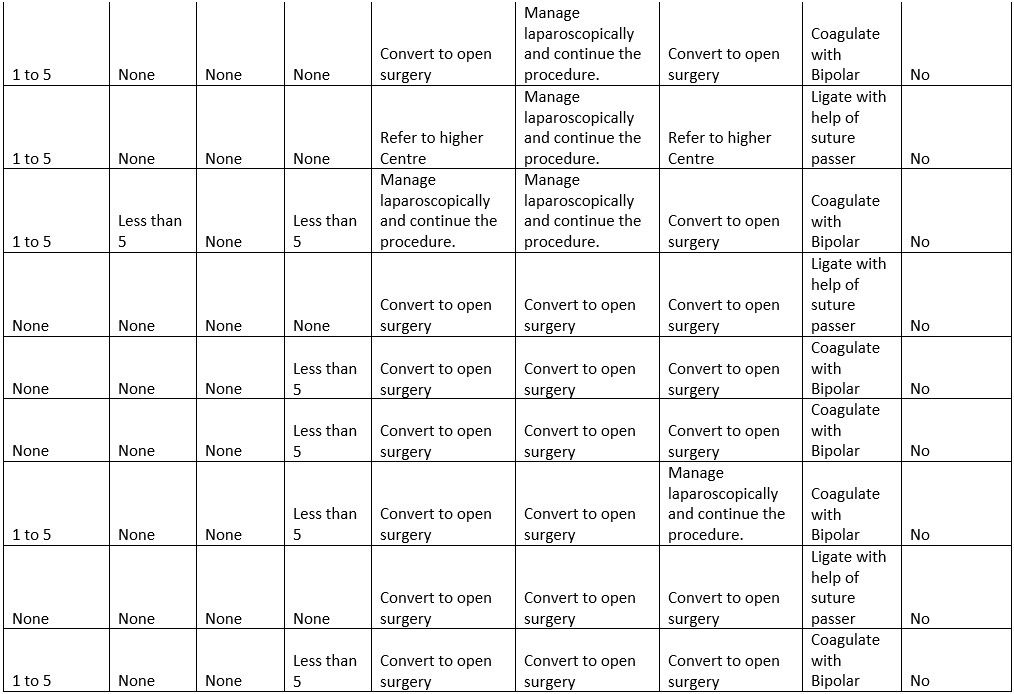
Table Sex 4.1 The Surgeon Particulars
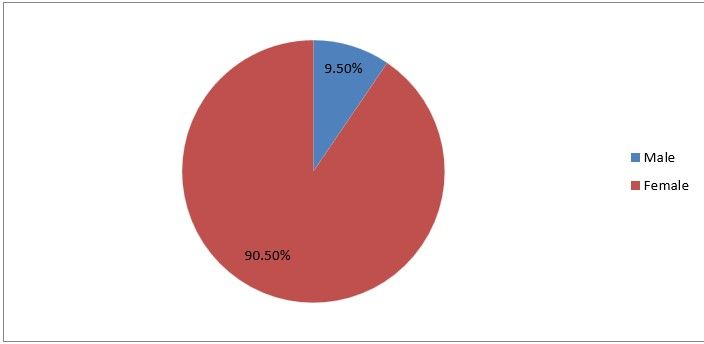
Figure1
Interpretation: This means that out of the total responses of 21, 90.5% are Males, and 9.5% are Females. The implication of the ratio to the study is showing that most laparoscopic surgeons are men.
Table 4.2 Specialization
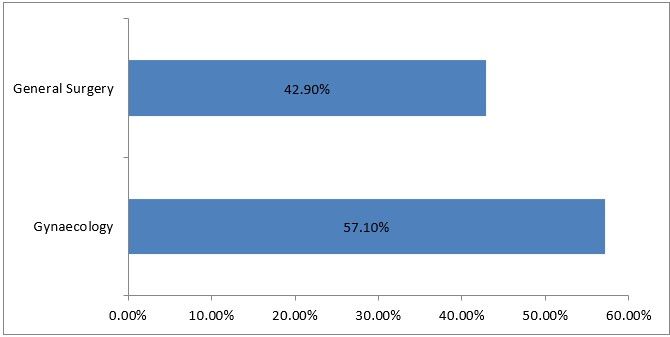
Figure 2
Interpretation: Most of the respondents are gynecologies.
Years of experience in Laparoscopy, the more years of experience the better outcome. 21 Responses
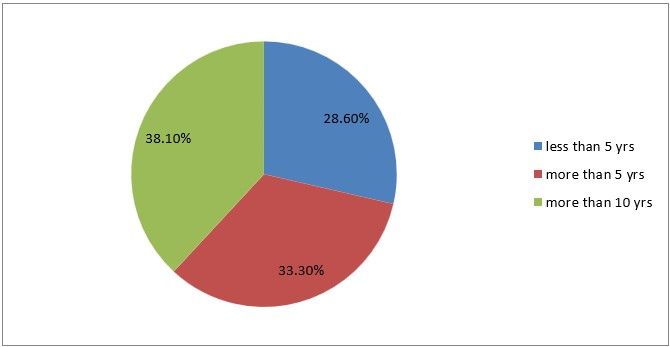
Figure 3
4.3 Questionnaire
1) What is the common laparoscopic surgery you perform?
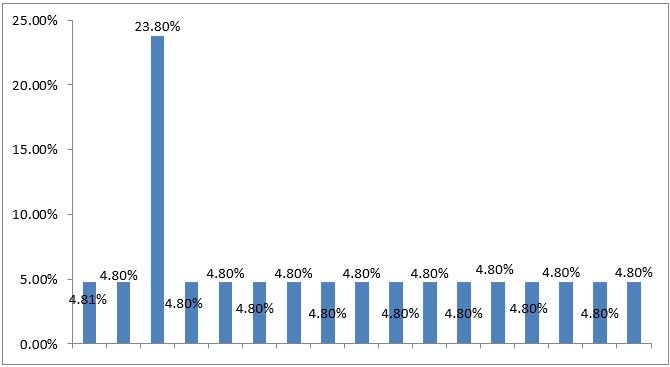
Figure 4
Interpretation: The commonest laparoscopic surgery that is frequently done by the mostly the respondence by chromo tubular and adhescologist with 23%, Others have to save persutry across the procedure
2) How many laparoscopic surgeries have you performed till March 2022
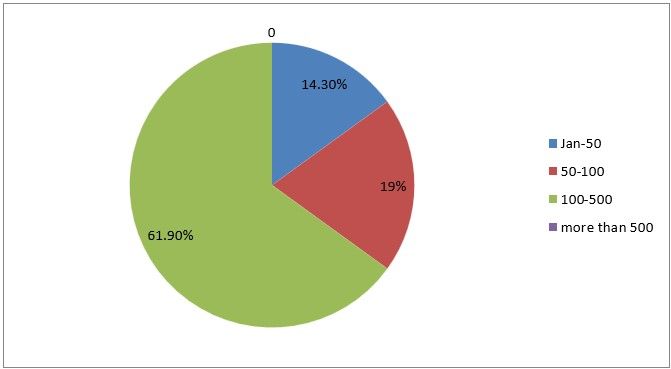
Figure 5
Interpretation: Only 14% of the respondents had less than 50 surgeries, 19% had 50 to 100 surgeries,61% between 100 to 500 and none of the respondents had more than 500 cases.
3) How many surgeries have you converted to open surgery due to entry complication
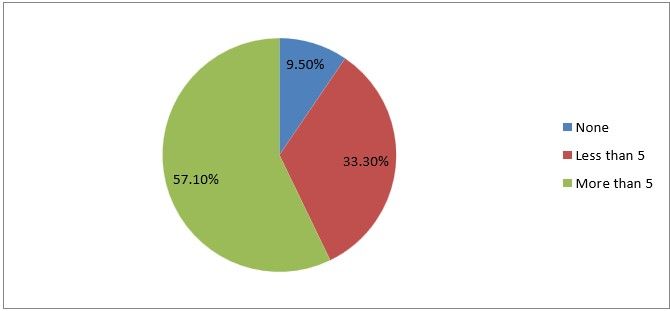
Figure 6
Interpretation: This result from the study shows that none of the respondents 57% of the respondents converted to laparotomy due to complications more than 5 times, 33% converted less than 5 cases to open surgeries and only 9% of a total number of respondents does not convert their cases to laparotomy.
4) What type of access techniques do you prefer?
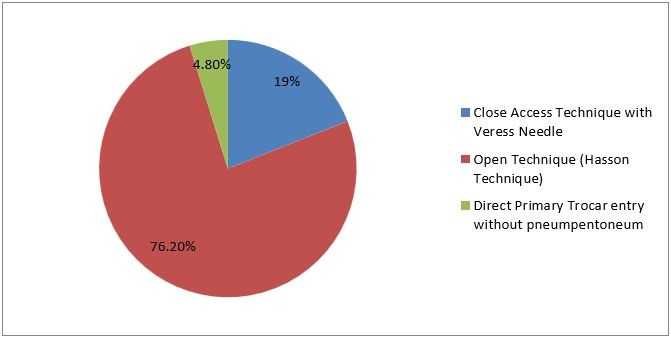
Figure 7
Interpretation: The result revealed that out of the 21 responses, 76.2% prefer the closed access technique with verses needle, 19% prefer the open technique (Hasson Technique) and 4.8% prefer direct primary trocar entry without preumpentoneum.
5) Your common site of entry
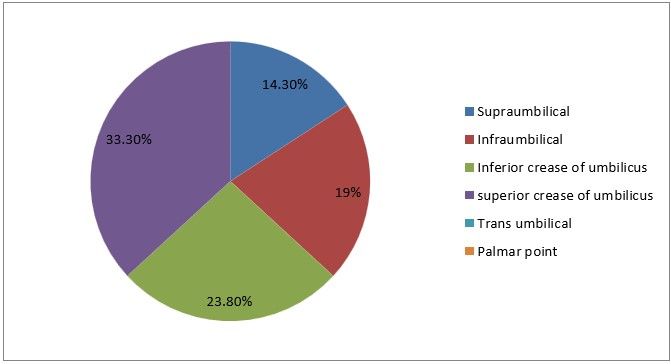
Figure 8
6) Direction of verses needle should be
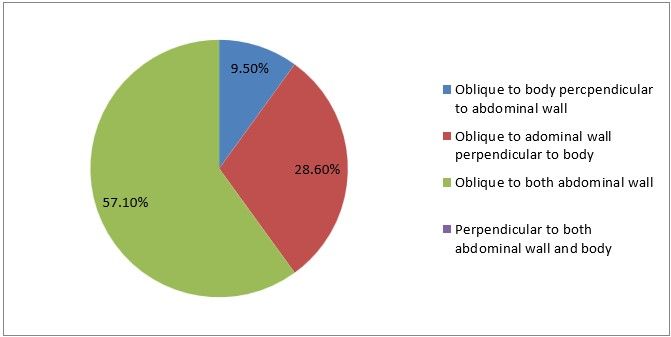
Figure 9
Interpretation: Only 9% of the respondents are correct in order to prevent visceral or vascular injury.
7) How much intra-abdominal pressure do you prefer to keep during primary trocar entry
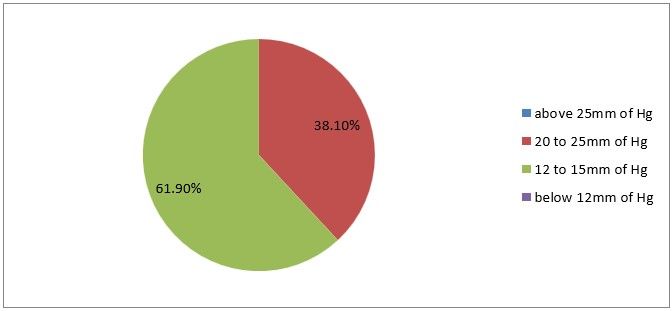
Figure 10
Interpretation: 38% are correct, you maintain intra-abdominal pressure between 20 to 25 mm of Hg.
8) How much intra-abdominal pressure do you prefer to keep during secondary trocar entry
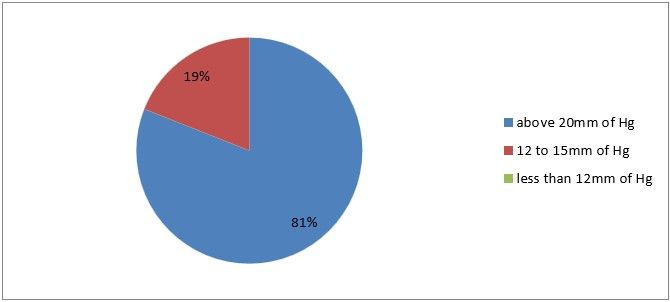
Figure 11
Interpretation: Here majority of respondents got it right at 81%, due to fact that the pressure most above 20 to 25 mmHg in other to prevent visceral injury.
9) With a previous history of two or more open abdominal surgeries, which technique do you prefer.
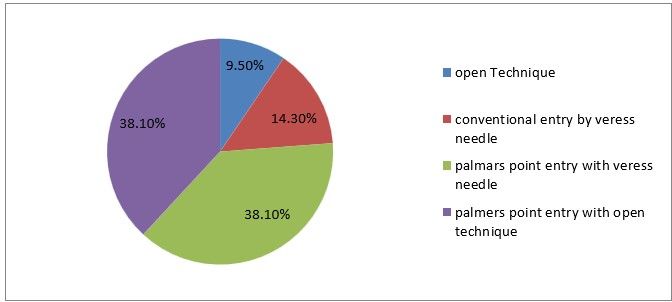
Figure 12
Interpretation: From the response of participants 9% prefer open techniques 14 % prefer convention entry by veress needle. 38% prefer palmer point entry with veress needle and 38% prefer palmer point entry with the open technique.
10) Pre-peritoneal insufflation is one of the commonest entry complications.
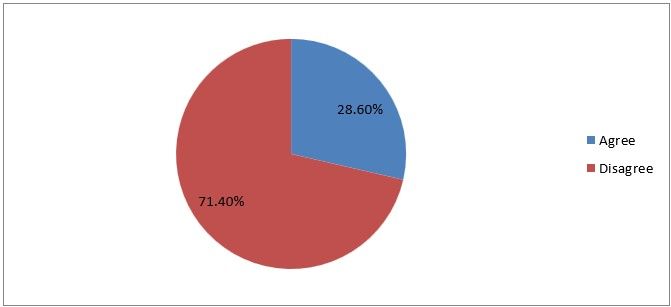
Figure 13
Interpretation: 28% of the respondents agree that pre peritoneal insufflation is one of the commonest entry complications seen in laparoscopy and 71% of them disagree which is right, this is not the commonest type of entry complication.
11) Atraumatic trocar is always safer than other trocars
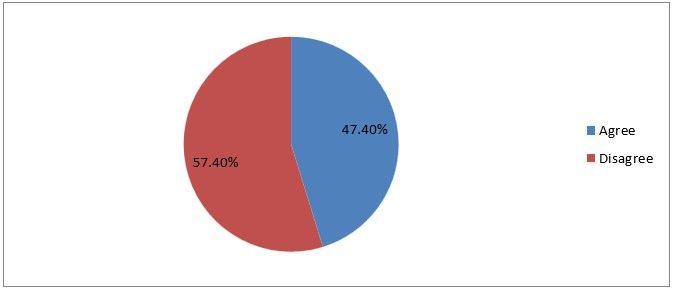
Figure 14
Interpretation: 47% of the respondents agree that an atraumatic trocar is always safer than another traumatic trocar while 57 % disagree with this statement, which is right the traumatic trocar is safer.
12) Palmar’s point is safer even if there is splenomegaly
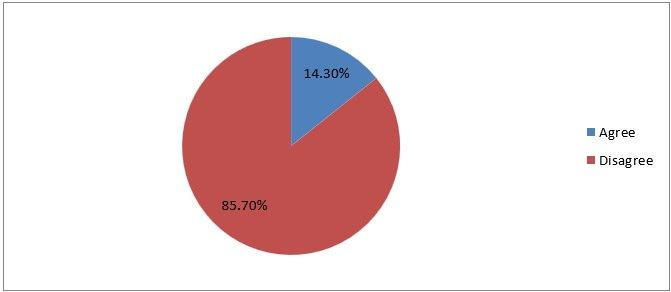
Figure 15
Interpretation: 14% agree that palmers point is even if there is splenomegaly and 86% disagree with this statement which is their right. Splenomegaly is a contraindication of palmers point.
13) How many entry complications do you encounter every year?
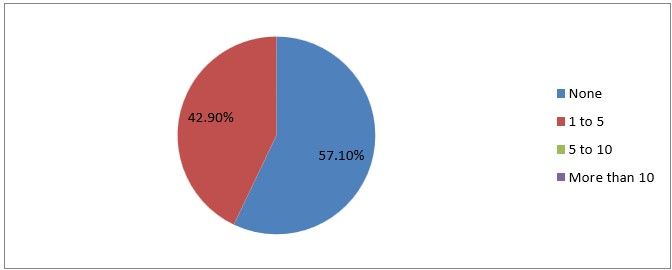
Figure 16
Interpretation: Only 42% of the respondents encountered 1 to 5 complications every year and others did none.
14) How many bowel injuries do you encounter per year?
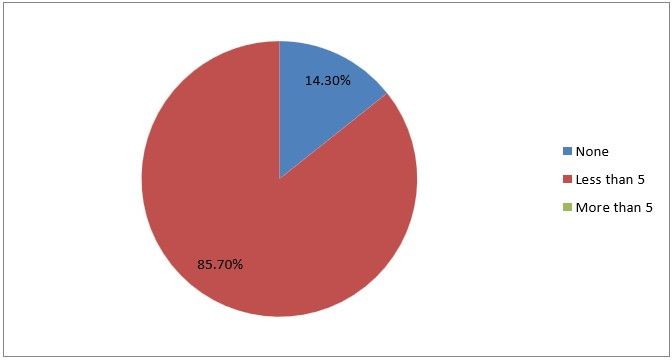
Figure 17
Interpretation: Out of the 21 responses to the question: how many bowel injuries do you encounter per year? The result revealed that 85.7% did not encounter bowel injury over the years, and less than 5 which represent 14.3% reported that they encounter bowel injury over the years. The implication is that.
15) How many urinary bladder injuries do you encounter per year?
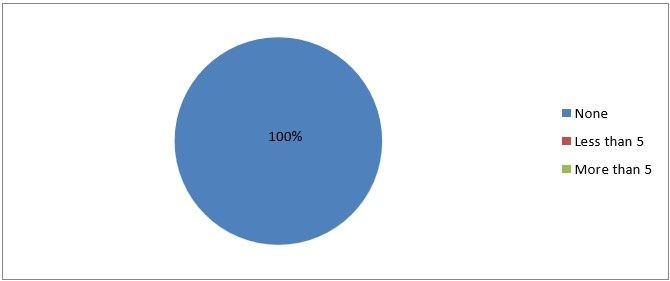
Figure 18
Interpretation: None of the respondents encountered urinary bladder injury through their procedure.
This place bladder injury during laparoscopy is rare.
16) How many vascular injuries do you encounter per year?
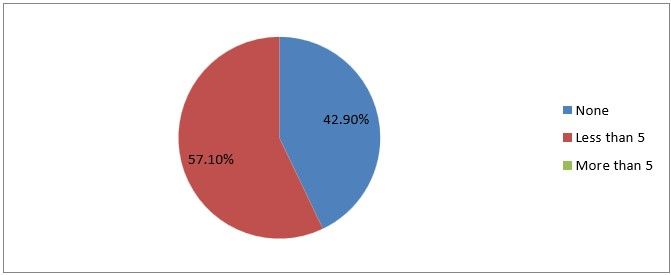
Figure 19
Interpretation: Among the respondents, 57% of encounters with less than 5 cases were as 42% don’t encounter vascular injuries.
17) How do you manage bowel perforation occurring during entry?
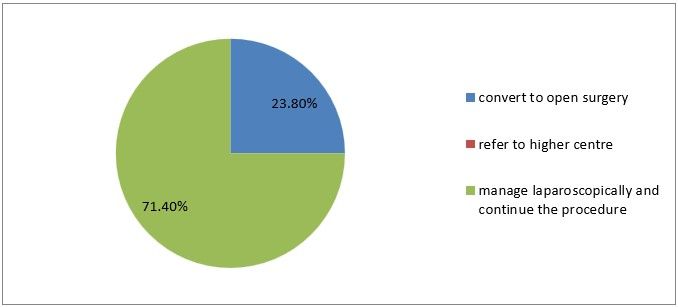
Figure 20
Interpretation: Among 21 respondents only 23% converted to open surgery when bowel perforation occurs and 71% managed laparoscopically and continue with the procedure.
18) How do you manage Urinary bladder perforation occurring during entry
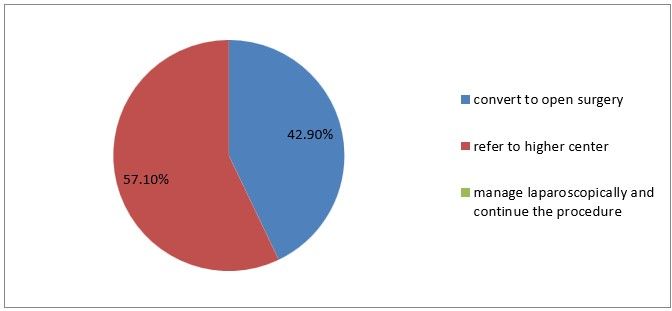
Figure 21
Interpretation: 42% of the respondents prefer to convert to open surgery when the urinary bladder is perforated while 57% refer to a higher center.
19) How do you manage great vessel injury occurring during trocar entry?
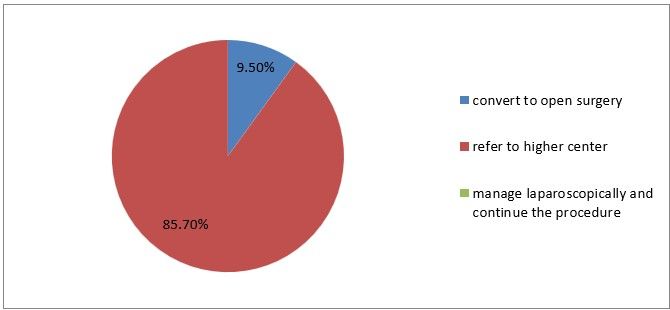
Figure 22
Interpretation: Only 9% out of the respondents can convert to open surgery when there are great vessels injury during trocar entry but others prefer to manage laparoscopic.
Interpretation: Only 9% out of the respondents can convert to open surgery when there is great vessel injury during trocar entry but others prefer to manage laparoscopically and continue with the procedure.
20) If you have accidentally injured inferior epigastric vessels, what will you do?
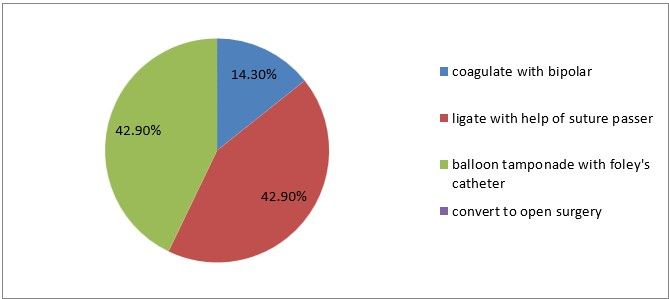
Figure 23
Interpretation: 14% prefer to coagulate with bipolar, 42% prefer ligation and another 42% prefer balloon tamponade with foleys catheter, when there are injuries to inferior epigastric vessels.
21) Have you encountered any death due to entry complication
Figure 24
Interpretation: This shows that all the respondents don’t encountered any death.
23 the following are some recommendations of respondents for safe abdominal entry and minimal entry complications.
Proper patient selection.
Palmer's point entry in previous surgery patient Open entry in a less experienced surgeon.
Elevation of abdominal wall, use automatic trocar, sufficient intraabdominal insufflation for trocar entry, using appropriate instruments, Use the technique you are trained with. When using the veress needle. Ensure the abdominal wall is lifted .