Radical cystectomy is the gold standard treatment for muscle-invasive bladder cancer. Traditionally, open surgery has been the preferred approach for performing this procedure. However, in recent years, robotic-assisted radical cystectomy (RARC) has gained popularity as a viable alternative. This essay aims to explore the advantages of RARC over open surgery, focusing on patient outcomes, perioperative factors, and long-term results. By examining the existing literature, it becomes evident that RARC offers several benefits, including reduced blood loss, shorter hospital stay, improved postoperative recovery, and comparable oncologic outcomes. These advantages highlight the superiority of RARC, making it a promising option for patients requiring radical cystectomy.
-
Introduction 1.1 Bladder Cancer and Radical Cystectomy 1.2 Evolution of Surgical Techniques: Open Surgery to Robotic-Assisted Approach 1.3 Thesis Statement: The Superiority of Robotic-Assisted Radical Cystectomy over Open Surgery
-
Patient Outcomes 2.1 Reduced Blood Loss 2.2 Minimized Surgical Trauma and Improved Cosmesis 2.3 Lower Rates of Intraoperative and Postoperative Complications 2.4 Improved Lymph Node Dissection
-
Perioperative Factors 3.1 Reduced Length of Hospital Stay 3.2 Faster Recovery and Return to Normal Activities 3.3 Enhanced Surgical Precision and Visualization 3.4 Lower Conversion Rates to Open Surgery
-
Long-Term Results 4.1 Oncologic Outcomes and Disease-Free Survival 4.2 Bladder Function and Quality of Life 4.3 Sexual Function and Urinary Continence
-
Cost-Effectiveness and Economic Considerations 5.1 Initial Investment and Equipment Costs 5.2 Potential Reduction in Postoperative Complications and Readmissions 5.3 Implications for Healthcare Resources and Utilization
-
Criticisms and Limitations of Robotic-Assisted Radical Cystectomy 6.1 Learning Curve and Surgeon Experience 6.2 Cost and Availability 6.3 Lack of Long-Term Data
-
Conclusion 7.1 Recap of Advantages: Reduced Blood Loss, Shorter Hospital Stay, Improved Recovery, Comparable Oncologic Outcomes 7.2 Future Directions and Further Research 7.3 Final Statement: The Superiority of Robotic-Assisted Radical Cystectomy
Introduction
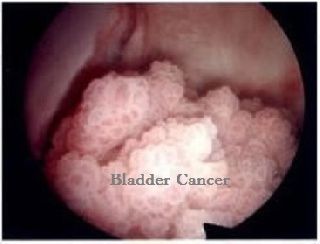
Bladder Cancer and Radical Cystectomy Bladder cancer is a significant global health concern, with radical cystectomy being the standard treatment for muscle-invasive disease. Radical cystectomy involves the removal of the bladder, adjacent lymph nodes, and surrounding structures, such as the prostate or uterus. Traditionally, open surgery has been the primary approach for performing this procedure. However, the introduction of robotic-assisted surgery has revolutionized the field of urology, providing an alternative method for radical cystectomy.
Evolution of Surgical Techniques:
Open Surgery to Robotic-Assisted Approach Open surgery has long been the standard technique for radical cystectomy. It involves a large abdominal incision, resulting in substantial trauma, prolonged hospital stay, and significant postoperative morbidity. In recent years, robotic-assisted radical cystectomy (RARC) has emerged as a minimally invasive alternative. RARC utilizes a robotic surgical system, which provides enhanced visualization, improved dexterity, and increased precision during the procedure.
Thesis Statement:
The Superiority of Robotic-Assisted Radical Cystectomy over Open Surgery This essay aims to explore the advantages of RARC over open surgery for radical cystectomy. By examining patient outcomes, perioperative factors, long-term results, and economic considerations, it becomes evident that RARC offers several benefits that make it a superior option for patients requiring radical cystectomy.
Patient Outcomes
Reduced Blood Loss
One of the significant advantages of RARC over open surgery is the reduced blood loss during the procedure. The robotic surgical system provides superior visualization, allowing for precise dissection and hemostasis. Studies have consistently shown that RARC results in significantly lower intraoperative blood loss compared to open surgery. Reduced blood loss not only decreases the need for transfusions but also contributes to better surgical outcomes and faster postoperative recovery.
Minimized Surgical Trauma and Improved Cosmesis
RARC offers the advantage of minimally invasive surgery, resulting in reduced surgical trauma compared to open surgery. The robotic instruments used in RARC allow for smaller incisions and more precise surgical maneuvers. As a result, patients experience less pain, reduced scarring, and improved cosmesis. The smaller incisions also contribute to faster wound healing and lower rates of wound-related complications.
Lower Rates of Intraoperative and Postoperative Complications
RARC has been associated with lower rates of intraoperative and postoperative complications compared to open surgery. The improved visualization and dexterity provided by the robotic system enable surgeons to perform precise and meticulous dissection, reducing the risk of inadvertent injuries to surrounding structures. Studies have shown a significant decrease in the rates of complications such as bowel injury, ureteral injury, and wound infections with RARC. This translates into improved patient safety and reduced healthcare costs associated with managing postoperative complications.
Improved Lymph Node Dissection
Accurate lymph node dissection is crucial in radical cystectomy for staging and prognosis. RARC allows for enhanced lymph node dissection due to the superior visualization provided by the robotic system. The three-dimensional high-definition view allows for a more meticulous and thorough removal of lymph nodes, leading to improved accuracy in staging and potentially better oncologic outcomes.
Perioperative Factors
Reduced Length of Hospital Stay
RARC has consistently demonstrated a shorter length of hospital stay compared to open surgery. The minimally invasive nature of RARC results in reduced postoperative pain, faster recovery, and earlier return to normal activities. Patients undergoing RARC often experience a quicker return of bowel function, enabling them to tolerate oral intake and ambulate earlier. The reduced length of hospital stay not only improves patient satisfaction but also reduces healthcare costs associated with prolonged hospitalization.
Faster Recovery and Return to Normal Activities
RARC offers a faster overall recovery compared to open surgery. The reduced surgical trauma and postoperative pain allow patients to resume their normal activities sooner. Studies have shown that patients undergoing RARC experience a quicker return to baseline functional status, including a faster recovery of urinary continence and sexual function. The enhanced recovery and improved quality of life contribute to better overall patient outcomes.
Enhanced Surgical Precision and Visualization
The robotic surgical system used in RARC provides several advantages over open surgery, including enhanced surgical precision and visualization. The robotic instruments offer a range of motion and articulation that exceeds the capabilities of the human hand. This enables surgeons to perform intricate maneuvers with greater precision and accuracy. Additionally, the three-dimensional high-definition view provided by the robotic system offers excellent visualization of the surgical field, allowing for better identification and preservation of vital structures.
Lower Conversion Rates to Open Surgery
While RARC is generally performed as a minimally invasive procedure, there may be cases where conversion to open surgery becomes necessary due to technical difficulties or intraoperative complications. However, studies have consistently shown that RARC has lower conversion rates compared to laparoscopic approaches. The robotic system's enhanced dexterity and visualization reduce the likelihood of conversion to open surgery, ensuring that the benefits of minimally invasive surgery are maximized for the majority of patients undergoing RARC.
Long-Term Results
Oncologic Outcomes and Disease-Free Survival
An essential consideration in radical cystectomy is achieving optimal oncologic outcomes. Multiple studies have shown that RARC is equivalent to open surgery in terms of oncologic efficacy, including the rates of positive surgical margins, lymph node yield, and disease-free survival. Long-term follow-up data indicate comparable oncologic outcomes between RARC and open surgery, supporting the use of RARC as a safe and effective approach for radical cystectomy.
Bladder Function and Quality of Life
Preserving bladder function and maintaining quality of life are crucial goals in radical cystectomy. RARC has shown promise in achieving these objectives. The precise dissection and preservation of neurovascular bundles offered by the robotic system contribute to better preservation of urinary continence and sexual function compared to open surgery. Studies have reported favorable outcomes in terms of urinary continence and sexual function in patients undergoing RARC, indicating a potential improvement in quality of life compared to open surgery.
Sexual Function and Urinary Continence
Preserving sexual function is a significant concern for patients undergoing radical cystectomy. RARC offers several advantages in this regard. The minimally invasive approach and enhanced visualization provided by the robotic system allow for precise nerve-sparing techniques, minimizing the risk of erectile dysfunction. Studies have shown comparable rates of sexual function preservation between RARC and open surgery, highlighting the potential benefits of RARC in maintaining sexual quality of life.
Cost-Effectiveness and Economic Considerations
Initial Investment and Equipment Costs
One of the primary concerns regarding RARC is the initial investment and equipment costs associated with the robotic surgical system. The acquisition and maintenance costs of the robotic system can be substantial. However, over time, as the technology becomes more widespread and the equipment is utilized for a broader range of procedures, the cost per case decreases. Moreover, cost-effectiveness analyses have shown that the long-term benefits of RARC, such as reduced postoperative complications, shorter hospital stays, and improved patient outcomes, may offset the initial investment costs.
Potential Reduction in Postoperative Complications and Readmissions
RARC has demonstrated a reduction in postoperative complications compared to open surgery. Fewer complications result in decreased healthcare costs associated with managing complications, including extended hospital stays, additional procedures, and readmissions. Cost-effectiveness analyses have indicated that the potential reduction in postoperative complications and readmissions can contribute to overall cost savings in the long run, making RARC a cost-effective option for radical cystectomy.
Implications for Healthcare Resources and Utilization
The shorter length of hospital stay and faster recovery associated with RARC have implications for healthcare resources and utilization. The reduced hospitalization period frees up hospital beds, allowing for more efficient utilization of resources. Additionally, the improved postoperative recovery and faster return to normal activities reduce the burden on healthcare facilities and healthcare providers, optimizing resource allocation.
Criticisms and Limitations of Robotic-Assisted Radical Cystectomy
Learning Curve and Surgeon Experience
One of the criticisms of RARC is the associated learning curve for surgeons. Mastering the robotic surgical system and acquiring the necessary skills to perform RARC proficiently can be time-consuming. Surgeon experience plays a crucial role in the outcomes of RARC. However, as more surgeons gain experience with the robotic system, the learning curve becomes less of a limitation.
Cost and Availability
The initial investment and equipment costs associated with the robotic surgical system can be a limitation for some healthcare institutions. The availability of the technology may also vary, with some regions or hospitals having limited access to robotic systems. However, as the technology becomes more