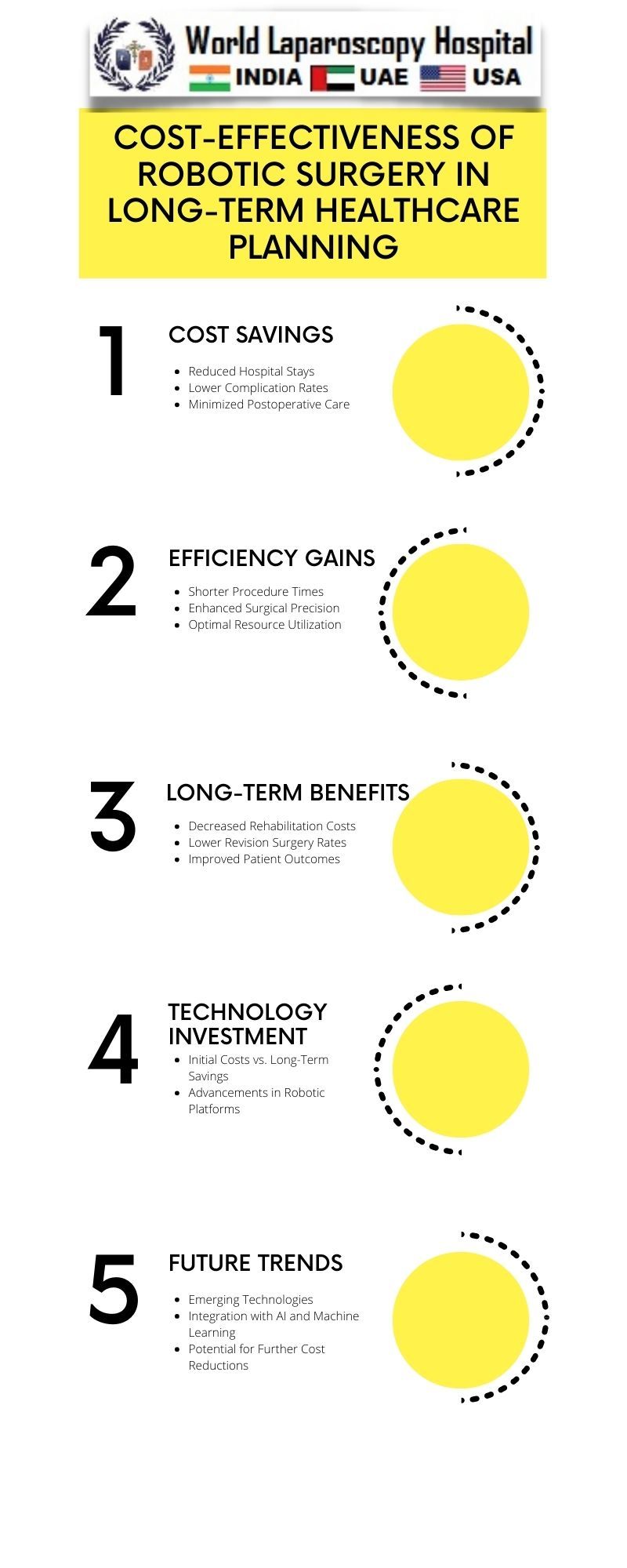
Cost-Effectiveness of Robotic Surgery in Long-Term Healthcare Planning
Introduction:
In the ever-evolving landscape of healthcare, the integration of cutting-edge technologies is crucial for improving patient outcomes and optimizing resource allocation. One such advancement that has garnered significant attention is robotic surgery. This article delves into the comprehensive analysis of the cost-effectiveness of robotic surgery in the context of long-term healthcare planning, exploring its potential benefits, challenges, and implications for the future of healthcare delivery.
 The Evolution of Robotic Surgery:
The Evolution of Robotic Surgery:
To understand the cost-effectiveness of robotic surgery, it's essential to trace the evolution of this technology. Robotic surgical systems, such as the da Vinci Surgical System, have rapidly advanced over the past two decades, offering enhanced precision, dexterity, and minimally invasive capabilities. Originally developed to assist surgeons in complex procedures, these systems have evolved into primary tools for various surgeries, ranging from urology and gynecology to general and colorectal surgery.
The Initial Investment: Balancing Innovation and Cost:
One of the primary barriers to the widespread adoption of robotic surgery is the substantial initial investment required for acquiring and maintaining robotic systems. Hospitals and healthcare institutions must weigh this cost against the potential long-term benefits, considering factors such as reduced complications, shorter hospital stays, and quicker patient recovery. While the upfront expenses can be daunting, proponents argue that the long-term gains may justify the investment.
Efficiency in Surgical Procedures:
Robotic surgery has demonstrated unparalleled efficiency in various surgical procedures. The precision and maneuverability offered by robotic systems allow surgeons to navigate complex anatomical structures with greater ease, leading to reduced blood loss, minimized tissue damage, and improved overall surgical outcomes. This increased efficiency contributes to shorter surgical durations, potentially allowing for more surgeries to be performed within a given timeframe.
Reduced Hospitalization and Recovery Time:
A significant factor influencing the cost-effectiveness of robotic surgery lies in the potential for reduced hospitalization and quicker patient recovery. Studies have suggested that patients undergoing robotic-assisted procedures may experience shorter hospital stays compared to traditional surgeries. The quicker recovery time not only translates to improved patient satisfaction but also reduces the strain on healthcare resources, contributing to potential cost savings in the long run.
Economic Impact of Complication Reduction:
Complications during and after surgery can significantly impact healthcare costs. Robotic surgery's precision and minimally invasive nature have been associated with lower complication rates in certain procedures. The economic implications of avoiding complications, such as infections, readmissions, and additional surgeries, can be substantial. While data on complication rates continues to evolve, the potential for long-term cost savings remains a compelling aspect of robotic surgery.
Workforce Considerations: Training and Staffing:
Integrating robotic surgery into healthcare practices necessitates investment in training for surgeons and support staff. As the technology becomes more prevalent, addressing workforce considerations becomes crucial for maximizing its benefits. Adequate training ensures proficiency and competence in utilizing robotic systems, minimizing the risk of errors and complications. Balancing the initial investment in training with the long-term gains in surgical efficiency is pivotal for successful adoption.
Patient-Centric Outcomes: Quality of Life and Satisfaction:
Beyond the quantitative metrics of cost-effectiveness, the impact of robotic surgery on patient-centric outcomes cannot be overlooked. Improved quality of life and patient satisfaction are inherent benefits of quicker recovery times and reduced postoperative complications. As healthcare systems increasingly prioritize patient-centered care, the positive impact of robotic surgery on these outcomes becomes a significant consideration in the overall cost-effectiveness analysis.
Future Trends and Innovations:
The field of robotic surgery is dynamic, with ongoing research and development aimed at further enhancing its capabilities. Future innovations may address current limitations, such as cost, training requirements, and accessibility. Advancements in artificial intelligence, telemedicine, and remote robotic surgery hold the potential to reshape the landscape of healthcare delivery, presenting new opportunities and challenges for long-term planning.
Conclusion:
The cost-effectiveness of robotic surgery in long-term healthcare planning is a multifaceted and evolving topic. While the initial investment is a notable barrier, the potential benefits in terms of surgical efficiency, reduced hospitalization, and improved patient outcomes cannot be ignored. As healthcare systems navigate the delicate balance between innovation and cost, a thorough understanding of the evolving landscape of robotic surgery is imperative. The future of healthcare delivery may well be shaped by the successful integration of this transformative technology into long-term strategic planning.
