Telemedicine and Remote Assistance in Laparoscopic Procedures
Introduction:
The evolution of medical technology has ushered in a new era for surgical practices, and one of the most transformative developments is the integration of telemedicine and remote assistance in laparoscopic procedures. This article delves into the multifaceted aspects of this revolutionary approach, exploring its implications, benefits, challenges, and the future it promises for the field of surgery.
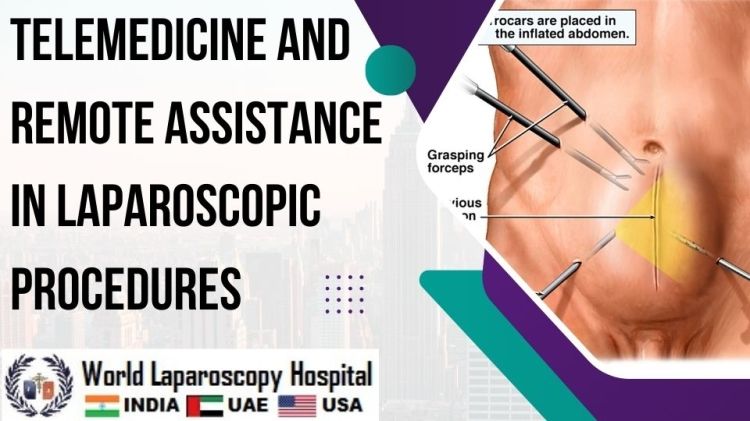
Understanding Laparoscopic Procedures:
Before delving into the role of telemedicine, it's crucial to comprehend the fundamentals of laparoscopic procedures. Laparoscopy, often referred to as minimally invasive surgery, involves making small incisions through which a camera and specialized instruments are inserted, allowing surgeons to visualize and operate inside the body without the need for large incisions. This technique has significantly reduced recovery times, postoperative pain, and hospital stays compared to traditional open surgeries.
The Emergence of Telemedicine in Surgery:
Telemedicine, broadly defined as the remote delivery of healthcare services using technology, has gained prominence across various medical specialties. In the realm of surgery, it has emerged as a powerful tool for enhancing communication, collaboration, and expertise-sharing. Telemedicine in laparoscopic procedures involves real-time video communication, enabling surgeons to provide or receive remote assistance during surgeries.
Real-Time Video Communication in Laparoscopic Procedures:
Advantages of Real-Time Video Communication:
Enhanced Collaboration:
Telemedicine facilitates seamless collaboration between surgeons, regardless of their geographical locations. Experts can virtually participate in surgeries, offering insights and guidance to less-experienced surgeons.
Global Access to Expertise:
Through real-time video communication, surgeons in remote or underserved areas can access the expertise of specialists located in major medical centers. This democratization of knowledge expands the reach of high-quality healthcare.
Training Opportunities:
Telemedicine in laparoscopic procedures opens up new avenues for surgical education and training. Novice surgeons can benefit from real-time guidance from mentors, fostering skill development and knowledge transfer.
Overcoming Challenges:
Technological Hurdles:
While advancements in technology have made real-time video communication more accessible, challenges such as connectivity issues, bandwidth limitations, and compatibility concerns may still impede its widespread adoption.
Security and Privacy Concerns:
Transmitting sensitive medical information over digital networks raises concerns about data security and patient privacy. Ensuring robust encryption and compliance with healthcare data protection standards is essential.
Applications in Laparoscopic Procedures:
Intraoperative Consultations:
Telemedicine allows surgeons to consult with specialists during a procedure, seeking guidance on complex cases or unexpected challenges. This instantaneous exchange of expertise can positively impact patient outcomes.
Telementoring:
Experienced surgeons can remotely mentor and guide less-experienced colleagues, fostering a continuous learning environment. This mentorship model contributes to the professional development of surgeons worldwide.
Remote Assistance in Critical Situations:
In emergency situations, where immediate access to specialized expertise is crucial, telemedicine ensures that help is just a video call away. This is particularly significant for healthcare facilities in remote or rural areas.
Case Studies and Success Stories:
International Collaborations:
Numerous success stories highlight the impact of international collaborations facilitated by telemedicine. Surgeons from different parts of the world have joined forces to perform complex laparoscopic procedures, pushing the boundaries of what was previously possible.
Training Programs:
Institutions have implemented telemedicine-based training programs for laparoscopic surgery, enabling surgeons to refine their skills under the guidance of experts. This has proven effective in addressing disparities in surgical training opportunities.
The Future of Telemedicine in Laparoscopic Procedures:
Technological Advancements:
Ongoing technological advancements, including the integration of augmented reality (AR) and virtual reality (VR) into telemedicine platforms, hold the potential to further enhance the capabilities of remote assistance in laparoscopic procedures.
Standardization and Guidelines:
As telemedicine continues to evolve, establishing standardized protocols and guidelines for its implementation in laparoscopic surgery becomes imperative. This includes addressing issues related to data security, licensure, and regulatory frameworks.
Patient-Centric Approaches:
The integration of telemedicine in laparoscopic procedures should prioritize patient-centric approaches. This involves ensuring that patients are well-informed about the use of remote assistance, obtaining their consent, and maintaining a focus on delivering high-quality, compassionate care.
Conclusion:
The marriage of telemedicine and laparoscopic procedures represents a significant leap forward in the evolution of surgical practices. As technology continues to advance and healthcare systems adapt, the potential to improve patient outcomes, expand access to surgical expertise, and contribute to the global advancement of surgical knowledge is immense. While challenges persist, the ongoing collaboration between surgeons, technologists, and policymakers promises a future where telemedicine plays an integral role in shaping the landscape of minimally invasive surgery.