Enhanced Recovery Protocols for Laparoscopic Surgery Patients
Introduction:
In the realm of modern surgical techniques, laparoscopic surgery has become increasingly prevalent due to its minimally invasive nature and faster recovery times. To further optimize the postoperative experience, Enhanced Recovery Protocols (ERPs) have emerged as a revolutionary approach. This article delves into the intricacies of ERPs tailored specifically for laparoscopic surgery patients, exploring the key components that contribute to improved outcomes.
Understanding Laparoscopic Surgery:
Laparoscopic surgery, also known as minimally invasive surgery, involves small incisions through which a camera and specialized instruments are inserted. This technique offers several advantages, including reduced scarring, less pain, and quicker recovery compared to traditional open surgery.
The Need for Enhanced Recovery:
While laparoscopic surgery inherently promotes quicker recovery, ERPs aim to further enhance patient outcomes. Traditional postoperative care often involved prolonged fasting, bed rest, and opioid-based pain management, contributing to complications and delayed recovery. ERPs represent a paradigm shift by adopting a multidisciplinary and patient-centered approach.
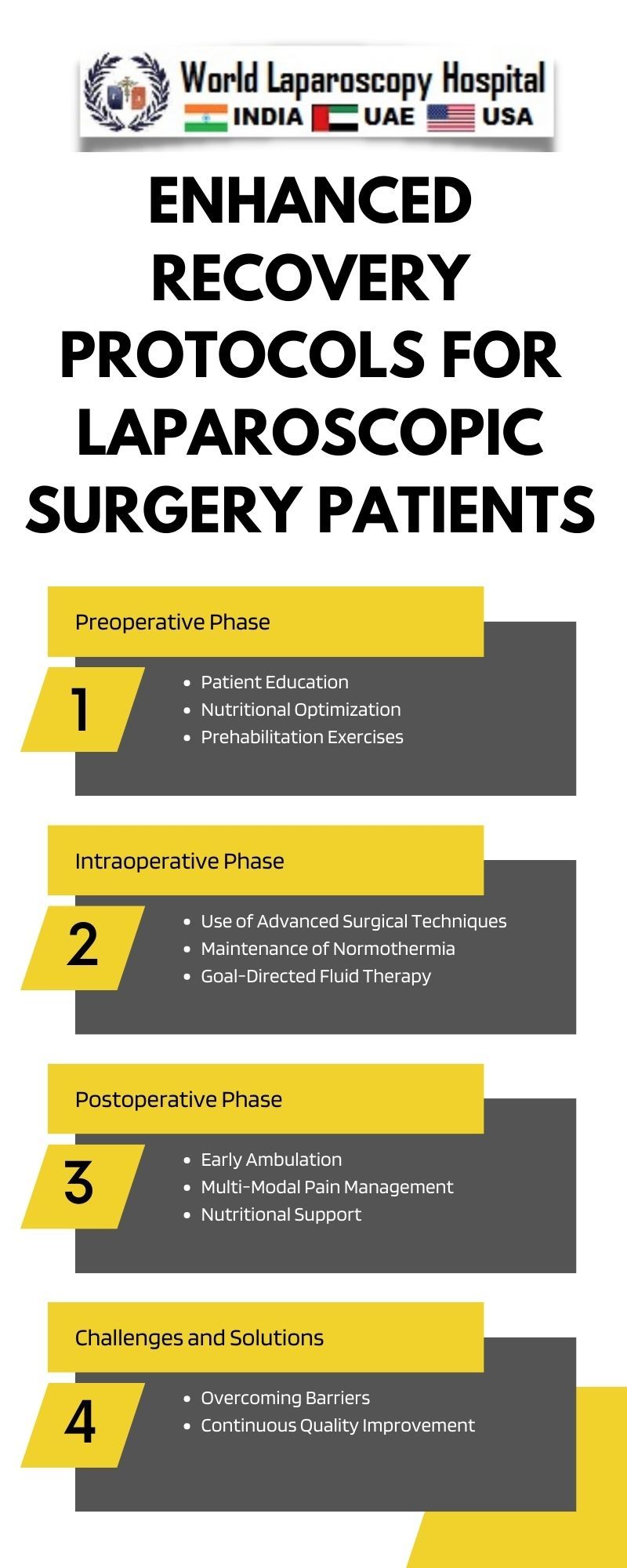
Key Components of Enhanced Recovery Protocols:
Preoperative Optimization:
Successful ERPs commence with thorough preoperative optimization. Patients are educated about the upcoming procedure, expected recovery milestones, and the importance of active participation in their rehabilitation. This preemptive approach fosters a sense of empowerment and reduces anxiety.
Multimodal Pain Management:
Gone are the days of heavy reliance on opioids for pain control. ERPs advocate for multimodal pain management strategies, combining analgesics, anti-inflammatory agents, and nerve blocks. This not only minimizes opioid-related side effects but also accelerates recovery by allowing patients to ambulate and engage in respiratory exercises sooner.
Minimized Fasting:
Conventional preoperative fasting practices have been reevaluated in ERPs. Shortened fasting periods contribute to improved postoperative outcomes by preventing dehydration and malnutrition. Clear liquids are often permitted up to a few hours before surgery, ensuring patients enter the operating room in a well-hydrated and nourished state.
Early Ambulation and Oral Intake:
ERPs prioritize early mobilization and oral intake, acknowledging the benefits of maintaining physiological functions. Prompt ambulation reduces the risk of complications such as deep vein thrombosis and aids in restoring bowel function. Similarly, early oral intake promotes gut motility, expediting the return to normal dietary habits.
Continuous Monitoring and Adaptation:
Flexibility is a cornerstone of ERPs. Continuous monitoring of patient progress allows healthcare providers to adapt the protocol based on individual responses. Personalized care plans ensure that each patient receives optimal support throughout their recovery journey.
Patient Education and Empowerment:
Empowering patients through education is a fundamental aspect of ERPs. Informed patients are more likely to actively participate in their recovery, adhere to postoperative instructions, and communicate effectively with their healthcare team. This collaborative approach fosters a sense of responsibility and facilitates a smoother recovery trajectory.
Evidence-Based Benefits of Enhanced Recovery Protocols:
The adoption of ERPs has demonstrated significant benefits in numerous studies. Reduced lengths of hospital stay, decreased postoperative complications, and faster return to normal activities are among the documented advantages. These outcomes not only benefit patients but also contribute to the efficient utilization of healthcare resources.
Overcoming Challenges and Barriers:
Despite the evident benefits, the implementation of ERPs faces challenges. Resistance to change, institutional barriers, and varying patient populations may pose obstacles. Comprehensive training for healthcare professionals, robust institutional support, and ongoing quality improvement initiatives are essential in overcoming these challenges.
Future Directions:
As technology and medical knowledge advance, ERPs for laparoscopic surgery will likely continue evolving. Incorporating innovations such as telehealth for preoperative education, personalized recovery apps, and artificial intelligence-driven monitoring systems could further enhance the effectiveness of ERPs.
Conclusion:
Enhanced Recovery Protocols represent a groundbreaking approach to optimizing the postoperative experience for laparoscopic surgery patients. By embracing a holistic and patient-centered methodology, ERPs contribute to faster recovery, reduced complications, and improved overall well-being. As healthcare continues to evolve, the integration of ERPs into standard practice holds the promise of transforming the landscape of surgical care.