Oesophageal adenocarcinoma (OAC) is a type of cancer that affects the oesophagus, the muscular tube that connects the throat to the stomach. OAC is a relatively rare cancer, but its incidence has been increasing rapidly in recent decades. Risk factors for OAC include obesity, smoking, and gastro-oesophageal reflux disease (GERD). Cholecystectomy, the surgical removal of the gallbladder, has also been identified as a potential risk factor for OAC. In this essay, we will explore the relationship between cholecystectomy and OAC, including the possible mechanisms behind this association and the implications for clinical practice.
Background
Cholecystectomy is one of the most common surgical procedures performed worldwide. It is typically done to treat gallbladder disease, such as gallstones or inflammation of the gallbladder. Cholecystectomy can be done using an open or laparoscopic approach, with the laparoscopic approach being the most common.
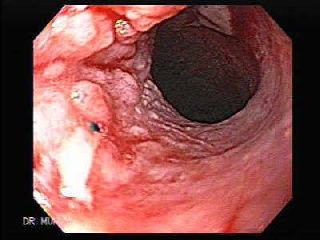
OAC is a relatively rare cancer, but its incidence has been increasing rapidly in recent decades. OAC is more common in men than in women, and it is more common in older individuals. Risk factors for OAC include obesity, smoking, and GERD. OAC is usually diagnosed at an advanced stage, and the prognosis is poor.
Mechanisms of the Association
The exact mechanisms behind the association between cholecystectomy and OAC are not fully understood. However, several possible mechanisms have been proposed, including:
-
Reflux of bile: Cholecystectomy can lead to an increase in the reflux of bile into the stomach and oesophagus. Bile is a digestive fluid that is produced in the liver and stored in the gallbladder. When the gallbladder is removed, bile flows directly into the small intestine, bypassing the storage and concentration that normally occurs in the gallbladder. This can result in an increase in the reflux of bile into the stomach and oesophagus, which may contribute to the development of OAC.
-
Alterations in gut microbiota: Cholecystectomy can alter the composition of the gut microbiota, the trillions of bacteria that live in the gastrointestinal tract. The gut microbiota play a key role in the regulation of the immune system and the maintenance of the gut barrier. Alterations in the gut microbiota have been associated with an increased risk of several gastrointestinal cancers, including OAC.
-
Chronic inflammation: Cholecystectomy can lead to chronic inflammation in the gastrointestinal tract. Chronic inflammation is a well-established risk factor for several types of cancer, including OAC. Chronic inflammation can lead to the formation of DNA damage, which can promote the development of cancer.
Clinical Implications
The association between cholecystectomy and OAC has important implications for clinical practice. Patients who have undergone cholecystectomy should be advised about the potential increased risk of OAC, and they should be monitored for symptoms of GERD and OAC. Patients with a history of cholecystectomy who develop symptoms of GERD, such as heartburn or regurgitation, should be evaluated for the presence of OAC.
Prevention strategies for OAC should also be considered in patients who have undergone cholecystectomy. These strategies may include lifestyle modifications, such as weight loss and smoking cessation, and the use of medications to treat GERD, such as proton pump inhibitors (PPIs) or histamine receptor antagonists (H2RAs).urther research is needed to fully understand the association between cholecystectomy and OAC and to determine the best strategies for preventing OAC in patients who have undergone cholecystectomy. Future studies should focus on identifying the underlying mechanisms behind this association and on developing targeted prevention and treatment strategies.
In conclusion, cholecystectomy has been identified as a potential risk factor for OAC. Patients who have undergone cholecystectomy should be advised about the potential increased risk of OAC and monitored for symptoms of GERD and OAC. Prevention strategies for OAC should be considered in patients who have undergone cholecystectomy, including lifestyle modifications and the use of medications to treat GERD. Further research is needed to fully understand the association between cholecystectomy and OAC and to develop effective prevention and treatment strategies.