Obesity is one of the most significant health challenges in the world. According to the World Health Organization (WHO), the prevalence of obesity has nearly tripled since 1975, with an estimated 1.9 billion adults being overweight, and of these, 650 million were obese in 2016. Obesity is a significant risk factor for numerous chronic diseases, including type 2 diabetes mellitus (T2DM), which is a metabolic disorder characterized by elevated blood glucose levels. There is evidence to suggest that bariatric surgery, a surgical procedure for weight loss, can cure T2DM in most patients. This essay will discuss the impact of weight loss surgery on T2DM.
Background
Obesity is a complex disease that results from an imbalance between energy intake and expenditure. It is characterized by the accumulation of excess body fat, which is associated with numerous health problems, including T2DM. T2DM is a metabolic disorder that occurs when the body cannot produce or use insulin effectively, resulting in elevated blood glucose levels. This condition can lead to severe complications such as cardiovascular disease, kidney disease, blindness, and neuropathy.
The standard treatment for T2DM is lifestyle modifications, including diet and exercise, and medication. While these interventions can be effective in managing T2DM, they may not be sufficient for patients with severe obesity. Bariatric surgery is a surgical procedure for weight loss that can help patients achieve sustained weight loss and improve their metabolic health.
Types of Bariatric Surgery
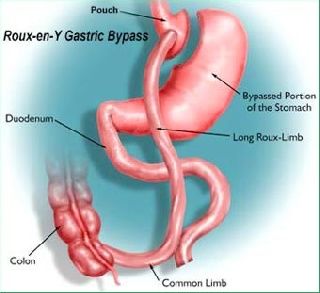
Bariatric surgery is classified into three main categories: restrictive, malabsorptive, and combined. Restrictive procedures reduce the size of the stomach, limiting food intake. Malabsorptive procedures reroute the small intestine, reducing the absorption of nutrients from food. Combined procedures combine both restrictive and malabsorptive techniques. The most commonly performed bariatric surgeries include gastric bypass, sleeve gastrectomy, and adjustable gastric banding.
Gastric Bypass
Gastric bypass surgery is a combined restrictive and malabsorptive procedure that involves creating a small stomach pouch and rerouting the small intestine to bypass the first portion of the intestine. The procedure reduces the amount of food that can be eaten and reduces the absorption of nutrients, leading to weight loss. Gastric bypass surgery has been shown to be effective in improving metabolic health, including T2DM.
Sleeve Gastrectomy
Sleeve gastrectomy is a restrictive procedure that involves removing a portion of the stomach, leaving a narrow, tube-like stomach. The procedure limits the amount of food that can be eaten, leading to weight loss. Sleeve gastrectomy has been shown to be effective in improving metabolic health, including T2DM.
Adjustable Gastric Banding
Adjustable gastric banding is a restrictive procedure that involves placing a band around the upper portion of the stomach, creating a small stomach pouch. The band can be adjusted to control the amount of food that can be eaten, leading to weight loss. Adjustable gastric banding has been shown to be effective in improving metabolic health, including T2DM.
Impact of Bariatric Surgery on T2DM
Bariatric surgery has been shown to have a significant impact on T2DM. A study by Mingrone et al. (2012) found that bariatric surgery can cure T2DM in a significant proportion of patients. The study followed 60 patients with severe obesity and T2DM who underwent either gastric bypass or biliopancreatic diversion surgery. The study found that 75% of patients who underwent gastric bypass and 95% of patients who underwent biliopancreatic diversion surgery achieved remission of T2DM after two years. Remission was defined as achieving normal blood glucose levels withoutthe need for medication. The study also found that weight loss was a significant predictor of T2DM remission, with patients who lost more weight having a higher chance of achieving remission.
Other studies have also shown the effectiveness of bariatric surgery in improving T2DM. A study by Schauer et al. (2017) found that patients who underwent gastric bypass had significantly greater improvement in glycemic control compared to those who received intensive medical therapy. The study followed 150 patients with severe obesity and uncontrolled T2DM who were randomly assigned to receive either gastric bypass or intensive medical therapy. The study found that 29% of patients who underwent gastric bypass achieved normal blood glucose levels without medication, compared to none in the medical therapy group.
A meta-analysis by Li et al. (2016) analyzed data from 11 randomized controlled trials and found that bariatric surgery was associated with significant improvement in glycemic control, including reductions in HbA1c, fasting blood glucose levels, and medication use. The meta-analysis also found that the magnitude of improvement was greater in patients who underwent gastric bypass or biliopancreatic diversion compared to those who underwent sleeve gastrectomy or adjustable gastric banding.
Mechanisms of Action
The mechanisms of action of bariatric surgery in improving T2DM are not fully understood, but several theories have been proposed. One theory is that bariatric surgery leads to weight loss, which improves insulin sensitivity and glucose metabolism. Another theory is that the surgery leads to changes in the gut hormones, which regulate appetite, glucose metabolism, and insulin secretion. Bariatric surgery has been shown to increase the secretion of hormones such as glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), which can improve glycemic control. The surgery may also alter the gut microbiota, which can impact glucose metabolism and inflammation.
Adverse Effects
While bariatric surgery has been shown to be effective in improving T2DM, it is not without risks. Complications can occur during and after surgery, including bleeding, infection, and blood clots. Long-term complications can also occur, such as nutritional deficiencies, bowel obstruction, and gastric dumping syndrome. Patients who undergo bariatric surgery require lifelong monitoring and follow-up care to manage these risks.
Conclusion
Bariatric surgery is an effective treatment option for patients with severe obesity and T2DM. The surgery has been shown to cure T2DM in a significant proportion of patients and improve glycemic control in others. The mechanisms of action are not fully understood, but weight loss and changes in gut hormones are thought to play a role. While bariatric surgery is associated with risks, the benefits may outweigh the risks for some patients. However, bariatric surgery should be considered a last resort after lifestyle modifications and medical therapy have failed. Further research is needed to understand the long-term outcomes and mechanisms of action of bariatric surgery in improving T2DM.