40% of Laparoscopic Gastric Banding Patients Have Complications
Laparoscopic gastric banding (LGB) has emerged as a popular surgical intervention for the management of obesity. However, despite its success in facilitating weight loss and improving metabolic parameters, complications associated with this procedure have been reported. This essay aims to explore the various complications encountered in laparoscopic gastric banding patients, with a specific focus on the fact that approximately 40% of these patients experience complications. Through an in-depth analysis of the literature and case studies, we will investigate the types of complications, their frequency, potential risk factors, and the implications they have for both patients and healthcare providers. Additionally, strategies to mitigate complications and improve patient outcomes will be discussed.
Introduction:
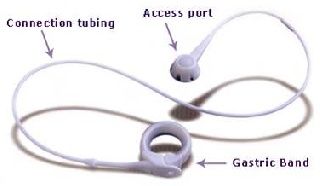
Laparoscopic gastric banding (LGB) has gained significant popularity as a surgical intervention for the management of obesity. It involves the placement of an adjustable silicone band around the upper portion of the stomach, creating a small pouch that limits food intake. LGB is considered a minimally invasive procedure, and it has shown promising results in terms of weight loss and improvement in metabolic parameters such as blood pressure and blood sugar levels. However, despite its benefits, it is crucial to recognize that a substantial proportion of laparoscopic gastric banding patients experience complications. Research suggests that approximately 40% of individuals undergoing this procedure encounter various complications, highlighting the need for a comprehensive analysis of these adverse events.
Complications Associated with Laparoscopic Gastric Banding:
Complications in laparoscopic gastric banding can range from minor issues to more severe complications requiring additional medical intervention. Some of the commonly encountered complications include band slippage, erosion, infection, dysphagia, and inadequate weight loss. Band slippage occurs when the band migrates from its original position, resulting in discomfort, reflux, and a decreased sense of satiety. Band erosion refers to the penetration of the band into the stomach tissue, which can cause infection, abscess formation, and pain. Dysphagia, or difficulty swallowing, may arise due to narrowing of the passage between the small pouch and the rest of the stomach. Inadequate weight loss, although not a direct complication, can be considered an unfavorable outcome of the procedure and may require revision surgery.
Risk Factors for Complications in Laparoscopic Gastric Banding:
Several factors contribute to the occurrence of complications in laparoscopic gastric banding patients. Patient-related factors include age, gender, body mass index (BMI), pre-existing medical conditions, and psychological well-being. Surgeon-related factors encompass surgical experience, expertise, and adherence to best practices. Device-related factors involve the type of gastric band used, its placement technique, and postoperative adjustments. Psychological and behavioral factors such as patient compliance, motivation, and eating habits also play a significant role in determining the risk of complications.
Clinical Implications of Complications in Laparoscopic Gastric Banding:
Complications in laparoscopic gastric banding patients can have profound implications for both patients and healthcare providers. From a patient perspective, complications can lead to physical discomfort, decreased quality of life, and psychological distress. In some cases, complications may necessitate additional surgical procedures or device removal, further impacting the patient's well-being and overall satisfaction with the procedure. From a healthcare standpoint, complications pose a significant economic burden due to the cost of additional interventions, hospital readmissions, and follow-up care. Moreover, the potential for complications can affect the decision-making process for both patients and healthcare providers when considering bariatric surgery options.
Mitigation Strategies and Improving Patient Outcomes:
To minimize complications and improve patient outcomes in laparoscopic gastric banding, several strategies can be implemented. Preoperative assessment and patient selection are crucial to identify individuals who are most likely to benefit from the procedure while minimizing risks. Surgeon training and experience play a vital role in ensuring optimal surgical technique and reducing the likelihood of complications. Device selection, placement technique, and regular postoperative adjustments are essential factors that can influence the occurrence of complications. Additionally, comprehensive postoperative monitoring, patient education, and support programs can help patients adhere to dietary and lifestyle changes, reduce the risk of complications, and achieve better long-term outcomes.
Conclusion:
Laparoscopic gastric banding is an effective surgical intervention for obesity management. However, it is important to acknowledge that a significant proportion of patients undergoing this procedure experience complications. These complications can have physical, psychological, and economic implications for both patients and healthcare providers. By understanding the types and risk factors of complications associated with laparoscopic gastric banding, healthcare providers can develop strategies to mitigate these risks and improve patient outcomes. Preoperative assessment, surgeon training, device selection, and postoperative monitoring are key areas that require attention to reduce the incidence of complications. Additionally, patient education and support programs play a crucial role in ensuring patient compliance and long-term success.
Further research is needed to better understand the underlying mechanisms and risk factors associated with complications in laparoscopic gastric banding. Long-term studies tracking patient outcomes and evaluating the effectiveness of mitigation strategies will contribute to evidence-based guidelines for optimizing patient care. Additionally, exploring alternative surgical interventions and advancements in technology may offer improved outcomes with fewer complications.
In conclusion, while laparoscopic gastric banding has demonstrated success in facilitating weight loss and improving metabolic parameters, complications are prevalent among a substantial percentage of patients. Understanding the types of complications, their risk factors, and the implications they have for patients and healthcare providers is essential for informed decision-making and patient management. By implementing mitigation strategies and improving patient selection, surgical technique, and postoperative care, healthcare providers can strive to reduce complications and enhance the overall success of laparoscopic gastric banding as an effective treatment for obesity.
Top
Introduction:
Laparoscopic gastric banding (LGB) has gained significant popularity as a surgical intervention for the management of obesity. It involves the placement of an adjustable silicone band around the upper portion of the stomach, creating a small pouch that limits food intake. LGB is considered a minimally invasive procedure, and it has shown promising results in terms of weight loss and improvement in metabolic parameters such as blood pressure and blood sugar levels. However, despite its benefits, it is crucial to recognize that a substantial proportion of laparoscopic gastric banding patients experience complications. Research suggests that approximately 40% of individuals undergoing this procedure encounter various complications, highlighting the need for a comprehensive analysis of these adverse events.
Complications Associated with Laparoscopic Gastric Banding:
Complications in laparoscopic gastric banding can range from minor issues to more severe complications requiring additional medical intervention. Some of the commonly encountered complications include band slippage, erosion, infection, dysphagia, and inadequate weight loss. Band slippage occurs when the band migrates from its original position, resulting in discomfort, reflux, and a decreased sense of satiety. Band erosion refers to the penetration of the band into the stomach tissue, which can cause infection, abscess formation, and pain. Dysphagia, or difficulty swallowing, may arise due to narrowing of the passage between the small pouch and the rest of the stomach. Inadequate weight loss, although not a direct complication, can be considered an unfavorable outcome of the procedure and may require revision surgery.
Risk Factors for Complications in Laparoscopic Gastric Banding:
Several factors contribute to the occurrence of complications in laparoscopic gastric banding patients. Patient-related factors include age, gender, body mass index (BMI), pre-existing medical conditions, and psychological well-being. Surgeon-related factors encompass surgical experience, expertise, and adherence to best practices. Device-related factors involve the type of gastric band used, its placement technique, and postoperative adjustments. Psychological and behavioral factors such as patient compliance, motivation, and eating habits also play a significant role in determining the risk of complications.
Clinical Implications of Complications in Laparoscopic Gastric Banding:
Complications in laparoscopic gastric banding patients can have profound implications for both patients and healthcare providers. From a patient perspective, complications can lead to physical discomfort, decreased quality of life, and psychological distress. In some cases, complications may necessitate additional surgical procedures or device removal, further impacting the patient's well-being and overall satisfaction with the procedure. From a healthcare standpoint, complications pose a significant economic burden due to the cost of additional interventions, hospital readmissions, and follow-up care. Moreover, the potential for complications can affect the decision-making process for both patients and healthcare providers when considering bariatric surgery options.
Mitigation Strategies and Improving Patient Outcomes:
To minimize complications and improve patient outcomes in laparoscopic gastric banding, several strategies can be implemented. Preoperative assessment and patient selection are crucial to identify individuals who are most likely to benefit from the procedure while minimizing risks. Surgeon training and experience play a vital role in ensuring optimal surgical technique and reducing the likelihood of complications. Device selection, placement technique, and regular postoperative adjustments are essential factors that can influence the occurrence of complications. Additionally, comprehensive postoperative monitoring, patient education, and support programs can help patients adhere to dietary and lifestyle changes, reduce the risk of complications, and achieve better long-term outcomes.
Conclusion:
Laparoscopic gastric banding is an effective surgical intervention for obesity management. However, it is important to acknowledge that a significant proportion of patients undergoing this procedure experience complications. These complications can have physical, psychological, and economic implications for both patients and healthcare providers. By understanding the types and risk factors of complications associated with laparoscopic gastric banding, healthcare providers can develop strategies to mitigate these risks and improve patient outcomes. Preoperative assessment, surgeon training, device selection, and postoperative monitoring are key areas that require attention to reduce the incidence of complications. Additionally, patient education and support programs play a crucial role in ensuring patient compliance and long-term success.
Further research is needed to better understand the underlying mechanisms and risk factors associated with complications in laparoscopic gastric banding. Long-term studies tracking patient outcomes and evaluating the effectiveness of mitigation strategies will contribute to evidence-based guidelines for optimizing patient care. Additionally, exploring alternative surgical interventions and advancements in technology may offer improved outcomes with fewer complications.
In conclusion, while laparoscopic gastric banding has demonstrated success in facilitating weight loss and improving metabolic parameters, complications are prevalent among a substantial percentage of patients. Understanding the types of complications, their risk factors, and the implications they have for patients and healthcare providers is essential for informed decision-making and patient management. By implementing mitigation strategies and improving patient selection, surgical technique, and postoperative care, healthcare providers can strive to reduce complications and enhance the overall success of laparoscopic gastric banding as an effective treatment for obesity.