Hysteroscopic sterilization is a minimally invasive surgical procedure that has gained popularity in recent years as an alternative to traditional sterilization methods. This procedure involves the placement of a small implant in the fallopian tubes to prevent the eggs from being fertilized. Despite the benefits of hysteroscopic sterilization, there have been reports of a higher failure rate with newer methods. This essay will explore the reasons behind the higher failure rate of newer methods of hysteroscopic sterilization.
Background:
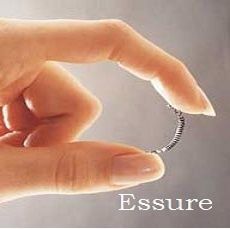
Hysteroscopic sterilization has been in use since the 1970s, but it was only in recent years that it gained popularity as a minimally invasive alternative to traditional sterilization methods. The procedure involves the placement of a small implant, typically made of polyester or nickel-titanium, in the fallopian tubes.
The implant works by inducing an inflammatory response that causes scar tissue to form around it, blocking the fallopian tubes and preventing fertilization. The procedure is performed under local anesthesia, and patients can usually resume their normal activities within a few days.
Failure Rate of Newer Methods:
While hysteroscopic sterilization has been shown to be effective, there have been reports of a higher failure rate with newer methods. In particular, studies have shown that the failure rate of Essure, a newer method of hysteroscopic sterilization, is higher than that of traditional sterilization methods.
The Essure device was approved by the U.S. Food and Drug Administration (FDA) in 2002 and was marketed as a safe and effective method of hysteroscopic sterilization. However, in 2018, the FDA issued a warning about the device, stating that it had received numerous reports of adverse events associated with the device, including chronic pain, perforation of the uterus or fallopian tubes, and migration of the device.
The higher failure rate of Essure and other newer methods of hysteroscopic sterilization can be attributed to several factors, including:
- Improper Placement of the Device:
The success of hysteroscopic sterilization depends on the proper placement of the device. If the device is not placed correctly, it may not induce the desired inflammatory response, and scar tissue may not form around it, leading to failure of the procedure.
Studies have shown that the improper placement of the Essure device is a significant contributor to its higher failure rate. This can be due to the complex nature of the device, which requires a high degree of skill to insert correctly.
- Variability in Anatomy:
Anatomy can vary from person to person, and this can impact the success of hysteroscopic sterilization. The fallopian tubes can be tortuous or have strictures, making it difficult to place the device correctly. In addition, the size of the uterus and the length of the fallopian tubes can also affect the success of the procedure.
Newer methods of hysteroscopic sterilization, such as Essure, are more likely to fail in patients with tortuous or obstructed fallopian tubes. Studies have shown that the failure rate of Essure is higher in women with a history of pelvic inflammatory disease or prior pelvic surgery, which can result in scar tissue and obstructed fallopian tubes.
- Inadequate Follow-Up:
Proper follow-up is essential after hysteroscopic sterilization to ensure the device is properly placed and that the procedure was successful. The failure rate of hysteroscopic sterilization can increase if follow-up is inadequate.
The follow-up period for newer methods of hysteroscopic sterilization, such as Essure, is typically shorter than that of traditional sterilization methods. Studies have shown that a shorter follow-up period can result in missed cases of device failure and may underestimate the failure rate of the procedure.
Lack of Long-Term Data:
Newer methods of hysteroscopic sterilization, such as Essure, have not been in use long enough to have long-term data on their effectiveness and safety. Most studies on newer methods have a follow-up period of only a few years, which may not be sufficient to assess the long-term risks and benefits of the procedure.
The lack of long-term data on newer methods of hysteroscopic sterilization is a concern for both patients and healthcare providers. Long-term data is necessary to determine the true failure rate of the procedure and to identify any long-term risks associated with the device.
Device Design:
The design of the hysteroscopic sterilization device can also impact the success of the procedure. Newer devices, such as Essure, are designed to be more flexible and easier to insert, but this can also make them more prone to migration and perforation.
The design of the device can also affect its ability to induce an inflammatory response and promote scar tissue formation. Some newer devices use materials that are less likely to induce an inflammatory response, which may lead to a higher failure rate.
Operator Experience:
The experience of the operator performing the hysteroscopic sterilization procedure can also affect its success. Proper training and experience are necessary to ensure that the device is placed correctly and that the procedure is performed safely.
Studies have shown that the failure rate of hysteroscopic sterilization is higher in less experienced operators. In addition, newer devices, such as Essure, require a high degree of skill to insert correctly, and the failure rate may be higher in less experienced operators.
Conclusion:
In conclusion, hysteroscopic sterilization is a minimally invasive alternative to traditional sterilization methods. However, newer methods of hysteroscopic sterilization, such as Essure, have been associated with a higher failure rate than traditional methods.
The higher failure rate of newer methods can be attributed to several factors, including improper placement of the device, variability in anatomy, inadequate follow-up, lack of long-term data, device design, and operator experience.
To reduce the failure rate of newer methods of hysteroscopic sterilization, healthcare providers should ensure that they receive proper training and experience in the procedure, and that they carefully select patients who are appropriate candidates for the procedure. Additionally, patients should be informed of the risks and benefits of hysteroscopic sterilization and should be encouraged to discuss all available options with their healthcare provider before making a decision.